Public Health Annual Report 2013
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

STATISTICS for MISSION: Church Groups and Outreach/Community Engagement Activities 2013 District: 12 Cornwall District Circuit: 1 Camborne-Redruth
STATISTICS FOR MISSION: Church Groups and Outreach/Community Engagement Activities 2013 District: 12 Cornwall District Circuit: 1 Camborne-Redruth FX of Led by Years Shared Local Lay Volun- Employ- Pres- Deacon Group Type Group Name (Nos) Running Frequency Initiative Location Church Worship Preacher Officer teer ee byter Circuit Summary 52 2 0 2 3 42 3 1 0 Barripper Church Groups Creative Arts PBK Ladies Group 12 Monthly Ecumenical Church l Premises Community Outreach Activities/Engagement Projects Family Support Foodbank 3 Weekly or More Ecumenical Church Premises Beacon Church Groups Youth/Children - Other () Stay & Play 2 Weekly or More - Church l l Premises Youth/Children - Other () Holiday Club 3 Quarterly - Church l l Premises Mother and Baby/Toddler Praise & Play 2 Monthly - Church l l l Premises Arts & Crafts Flower Club 4 Monthly - Church l Premises Fellowship Group Fellowship 3 Monthly - Church l Premises Fellowship Group Ladies Fellowship 51 Fortnightly - Church l Premises Other () Soup & Sweet 3 Monthly - Church l Premises Other () Homebake 25 Monthly - Church l Premises Community Outreach Activities/Engagement Projects Playgroups/nurseries/pre- Toy Library 3 Weekly or More Ecumenical Church schools Premises Family Support Foodbank 3 Weekly or More Ecumenical Church l Premises Adult fellowship/social Camborne/Redruth 3 Fortnightly Local Authority Communit groups Disabled Club y Space Brea Church Groups - STATISTICS FOR MISSION: Church Groups and Outreach/Community Engagement Activities 2013 District: 12 Cornwall District Circuit: -

Environmentol Protection Report WATER QUALITY MONITORING
5k Environmentol Protection Report WATER QUALITY MONITORING LOCATIONS 1992 April 1992 FW P/9 2/ 0 0 1 Author: B Steele Technicol Assistant, Freshwater NRA National Rivers Authority CVM Davies South West Region Environmental Protection Manager HATER QUALITY MONITORING LOCATIONS 1992 _ . - - TECHNICAL REPORT NO: FWP/92/001 The maps in this report indicate the monitoring locations for the 1992 Regional Water Quality Monitoring Programme which is described separately. The presentation of all monitoring features into these catchment maps will assist in developing an integrated approach to catchment management and operation. The water quality monitoring maps and index were originally incorporated into the Catchment Action Plans. They provide a visual presentation of monitored sites within a catchment and enable water quality data to be accessed easily by all departments and external organisations. The maps bring together information from different sections within Water Quality. The routine river monitoring and tidal water monitoring points, the licensed waste disposal sites and the monitored effluent discharges (pic, non-plc, fish farms, COPA Variation Order [non-plc and pic]) are plotted. The type of discharge is identified such as sewage effluent, dairy factory, etc. Additionally, river impact and control sites are indicated for significant effluent discharges. If the watercourse is not sampled then the location symbol is qualified by (*). Additional details give the type of monitoring undertaken at sites (ie chemical, biological and algological) and whether they are analysed for more specialised substances as required by: a. EC Dangerous Substances Directive b. EC Freshwater Fish Water Quality Directive c. DOE Harmonised Monitoring Scheme d. DOE Red List Reduction Programme c. -

CORNWALL. FAR 1403 Pascoe Wm
TRADES DIRECTORY.] CORNWALL. FAR 1403 Pascoe Wm. Pomeroy,Grampound Road PearceP.Lower Gooneva,Gwinear,Hayle Penge}lyR.Low.Crankan,Gulval,Penznc Pascpe Woodman, Woon, Roche R.S.O PearcePeter, Pellutes, Troon, Camborne Pengelly Richard, Tresquite mill, Lan- Passmore Hy.Penhale,Millbrook,Plymth Pearce Richard, Crill, Budock, Falmth sallos, Polperro R.S.O Paul J.Kirley,Chacewater,ScorrierR.S.O Pearce Richard, Treganver & Pen water, Pengelly Thos.H.Bone,Madron,Penzance PaulJosrah,Chymbder,Gunwalloe,Helstn Broadoak, Lostwithiel Pengelly William, Boscawen'oon, St. Paul Nicholas, Chacewood, Kenwyn,Kea Pearce Richard, Tregoning mill, St. Buryan R.S.O Paul W m.Newham,Otterham, Camelford Keverne R. S. 0 PengillyA. Pednavounder ,St.Kevrn.RSO Paul William, Withevan, Jacobstow, Pearce Samuel, Bodiga & The Glebe, St. Pengilley Alexander,Trice, Grade, Ruan Stratton R.S.O Martin-by-Looe, East Looe R.S.O Minor R.S.O PaulingJ .Marsh gate,Otterhm.Camelfrd Pearce Sidney, Lane end, Camelford Pengilly Mrs. E.Gwavas,Sithney,Helston Paull Henry, Carvanol, Illo5an,Redruth Pearce Stph. Jn, Baldhu, Scorrier R.S.O Pengilly J. Trebarbath,St.KeverneR.S.O Paul John, Chacewater, Scorrier R.S.O Pearce T.Bottonnett,Lezant,Launceston Pengilly P. Church town,SancreedR.S.O Paull John, Forge, Treleigh, Redruth Pearce Thomas,Pendriscott,DuloeR.S.O Penhale William, Trekinner, Laneast, Paull John Truscott, Trelonk, Ruan- Pearce Thomas, Trebarvah, Perran Uth- Egloskerry R.S.O Lanihorne, Grampound Roa:d noe, Marazion R.S.O Penhaligon Andrew, College, Penryn Paull Richard, Carn Brea R.S.O Pearce Thomas Mallow, Pelyne,Talland, Penhaligon Charles, Featherbeds, Ken• 1 Paull Richard, :Forest, Redruth Polperro R.S.O wyn, Truro Paull Thos. -

CORNWALL Extracted from the Database of the Milestone Society
Entries in red - require a photograph CORNWALL Extracted from the database of the Milestone Society National ID Grid Reference Road No Parish Location Position CW_BFST16 SS 26245 16619 A39 MORWENSTOW Woolley, just S of Bradworthy turn low down on verge between two turns of staggered crossroads CW_BFST17 SS 25545 15308 A39 MORWENSTOW Crimp just S of staggered crossroads, against a low Cornish hedge CW_BFST18 SS 25687 13762 A39 KILKHAMPTON N of Stursdon Cross set back against Cornish hedge CW_BFST19 SS 26016 12222 A39 KILKHAMPTON Taylors Cross, N of Kilkhampton in lay-by in front of bungalow CW_BFST20 SS 25072 10944 A39 KILKHAMPTON just S of 30mph sign in bank, in front of modern house CW_BFST21 SS 24287 09609 A39 KILKHAMPTON Barnacott, lay-by (the old road) leaning to left at 45 degrees CW_BFST22 SS 23641 08203 UC road STRATTON Bush, cutting on old road over Hunthill set into bank on climb CW_BLBM02 SX 10301 70462 A30 CARDINHAM Cardinham Downs, Blisland jct, eastbound carriageway on the verge CW_BMBL02 SX 09143 69785 UC road HELLAND Racecourse Downs, S of Norton Cottage drive on opp side on bank CW_BMBL03 SX 08838 71505 UC road HELLAND Coldrenick, on bank in front of ditch difficult to read, no paint CW_BMBL04 SX 08963 72960 UC road BLISLAND opp. Tresarrett hamlet sign against bank. Covered in ivy (2003) CW_BMCM03 SX 04657 70474 B3266 EGLOSHAYLE 100m N of Higher Lodge on bend, in bank CW_BMCM04 SX 05520 71655 B3266 ST MABYN Hellandbridge turning on the verge by sign CW_BMCM06 SX 06595 74538 B3266 ST TUDY 210 m SW of Bravery on the verge CW_BMCM06b SX 06478 74707 UC road ST TUDY Tresquare, 220m W of Bravery, on climb, S of bend and T junction on the verge CW_BMCM07 SX 0727 7592 B3266 ST TUDY on crossroads near Tregooden; 400m NE of Tregooden opp. -
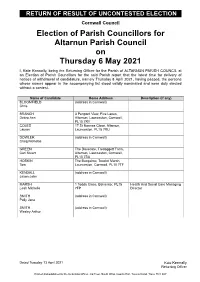
Election of Parish Councillors for Altarnun Parish Council on Thursday 6 May 2021
RETURN OF RESULT OF UNCONTESTED ELECTION Cornwall Council Election of Parish Councillors for Altarnun Parish Council on Thursday 6 May 2021 I, Kate Kennally, being the Returning Officer for the Parish of ALTARNUN PARISH COUNCIL at an Election of Parish Councillors for the said Parish report that the latest time for delivery of notices of withdrawal of candidature, namely Thursday 8 April 2021, having passed, the persons whose names appear in the accompanying list stood validly nominated and were duly elected without a contest. Name of Candidate Home Address Description (if any) BLOOMFIELD (address in Cornwall) Chris BRANCH 3 Penpont View, Five Lanes, Debra Ann Altarnun, Launceston, Cornwall, PL15 7RY COLES 17 St Nonnas Close, Altarnun, Lauren Launceston, PL15 7RU DOWLER (address in Cornwall) Craig Nicholas GREEN The Dovecote, Tredoggett Farm, Carl Stuart Altarnun, Launceston, Cornwall, PL15 7SA HOSKIN The Bungalow, Trewint Marsh, Tom Launceston, Cornwall, PL15 7TF KENDALL (address in Cornwall) Jason John MARSH 1 Todda Close, Bolventor, PL15 Health And Social Care Managing Leah Michelle 7FP Director SMITH (address in Cornwall) Polly Jane SMITH (address in Cornwall) Wesley Arthur Dated Tuesday 13 April 2021 Kate Kennally Returning Officer Printed and published by the Returning Officer, 3rd Floor, South Wing, County Hall, Treyew Road, Truro, TR1 3AY RETURN OF RESULT OF UNCONTESTED ELECTION Cornwall Council Election of Parish Councillors for Antony Parish Council on Thursday 6 May 2021 I, Kate Kennally, being the Returning Officer for the Parish of ANTONY PARISH COUNCIL at an Election of Parish Councillors for the said Parish report that the latest time for delivery of notices of withdrawal of candidature, namely Thursday 8 April 2021, having passed, the persons whose names appear in the accompanying list stood validly nominated and were duly elected without a contest. -

Cornwall. Tam 1343
COURT DIRECTORY.] CORNWALL. TAM 1343 Sowden William George, Helford vi: la, Stephens John, Boldulgate, Lanteglos, r Stribley Misses, South vil.PadstowR.S.O Clinton road, Redruth Camelford Strick Wm.O. New rd.Newlyn,Penzance So well Rev. Charles Richard B. A. Vicar- Stephens John, Lower Bore st. Bodmin 1Stringer Misses, St. Thomas' rd. Launcstn age, Gorran, St. Austell Stephens John, Elm terrace, St. Austell Stripp John Austen, West cliff, Looe Sowell Rev. Richard Herbert B.A. Bank Ste:)hens John, Lambp':Lrk place, Par, West, East Looe R.S.O street, St. Columb Major R S.O Par Sta•ion R.S.O Stripp Mrs. Attercliffe, Loo3 East R.S.O SpargoJohnCo1•nish,Fro2"pool,Gwennap, Stephens John, Rosevean house, Rose- Stripp Samuel, Beech terraca, Looe Perranwell Station R.S.O vean road, Penzance West, East Looe R.S.O Spargo Stephen, Cusgarne, Gwennap, Stephens John Gilbert, The Cottage, Stripp William, West cliff, Looe West, Perranwell Station R.S.O Ashfbld, l<'almouth EasL Looe R.S.O Spargo Thomas, Cusgarne, Gwennap, Stephen!! John Gill, Pentewan,St.Austell Strong John Mortimer, St. Stephen's, Perranwell Station R.S.O StephensMartin,Illogan highway,Redrth Launceston Sparnall Mrs. Esplanade, Fowey R.S.O Stephens Mrs. Hembal, St. Mewan, St. Strong John, Barn street, Liskeard Spear Christopher, Callington R.S.O Austell StrongmanJ.H.32Wellington ter.Falmth Spear Gideon E. Kelly villa, Calstock Stephens Mrs. Hillside, Castle st. Bojmin Stumbles Charles, 3 Tamar ter. Saltash Spear John Gumb, Callington R.S.O Step hens Mrs. 103 Killigrew st. Falmouth Stumbles Mrs. 6 Tamar terrace, :Saltash Spear Matthew, Treverbyn cottage, Stephens Mrs. -

Cornwall. [Kelly S
7 466 GRO CORNWALL. [KELLY S GROCERS & TEA DEALERS-continued. Geary Jn. 15 St. Dominick st. Penzance Hicks & Son, 4 Market st. St. .A.ustell Coath Robert Pill, .Delaware house, George Mrs. Ann, Barn street, Liskeard Hicks J.Sellick,Forest. EastLooe R.S.O Gunnislake, Tavistock George Frank B. Moles worth street, Hicks Miss;\'Iary, Forest. EastLooeR. S. 0 Cobeldick & Co. Fore street, St. Columb Wadebridge R.S.O tHigmanMrs.Emma.,Molesworth street, Major R.S.O George Mrs. Mary, 3 Agar crescent, Wadebridge R.S.O Cock M. A. & Son, to Boscawen Bridge Green Lane, Redruth Hill Henry & Chas. I Taroveor road, & road, Truro George Virilliam Mitchell, Church town, 28 Market place, Penzance Cock James, Leeds Town, Hay le Mullion, Cury Cross Lanes R.S. 0 Hillman Jabez, Calstock, Tavistock Cock Mrs. Jane,gr Green lane, Redrnth Gerrans Mrs. H. Probus R.S.O Hockin Mrs. }<'. Mousehole, Penzance Cock L, C. The Quay, St. Mawes R.S.O Gerry William, Henwood, Linkinhorne, Hockin Fredcrick, Mouschole, Penzance Colenso & Son, Probus R.S.O Callington R.S.O HockinWm.Webb,Markctpl.Camborne Collard W. Tresillian, Probus R.S.O Gerry Wm. A. 1Green market,Penzance Hoc.:king Robt.g4Smithick hill,Falmouth Collett J.St.Just-in-Roseland, Falmouth Gilbart Thoma11 T. Fore st. Camelford Hodge Mrs. Elizabeth, 32 St. Clement Colliver J. G. & Son, Bank street, Gilbert Francis, Pendarves street, Tuck- street Truro St. Columb :Major R.S.O ingmill, Camborne Hodge Mrs. Jane, Probus R.S.O · Cook w·. & Co. Church st. Lannceston Giles Francis Treseder, Polperro R.S.O Hodge R. -
Air Quality Action Plan (AQAP) Within 12-18 Months Setting out Measures It Intends to Put in Place in Pursuit of the Objectives
Information Classification: PUBLIC Cornwall Air Quality Action Plan Updated November 2020 Information Classification: PUBLIC Cornwall Air Quality Action Plan Policy Context 4 Local Air Quality Management (LAQM) 4 Air Pollution in Cornwall 5 Existing Air Quality Management Areas 5 Health Effects of Air Pollution 6 Health-related aims 6 Social Equity 9 Social Equity Related to Air Quality 9 The Cornwall Indices of Multiple Deprivation 2015 9 Taking Account of Social Equity when Determining Air Quality Improvements 12 Fuel Poverty 12 Local policies, programmes and strategies 14 Local Plan Overview 14 Local Plan Policies 14 Development in Cornwall 15 Local Transport Plan 16 Working with Highways England 17 The Cornwall Air Quality Action Plan 20 Air Quality Working Group Overview 20 Air Quality Action Plan 20 Consultation Overview 21 Consultation Process 21 Evaluation of Air Quality Actions 22 Monitoring of the Air Quality Action Plan 22 Conclusion 23 Air Quality Management Area Maps 26 Level of Air Quality Improvement Required 31 Nitrogen Dioxide concentrations 31 Cornwall Council Generic Actions 34 Camborne / Pool / Redruth (CPR) AQMA 53 Bodmin AQMA 59 Tideford AQAP 69 Gunnislake AQMA 76 St Austell AQMA 84 Truro AQMA 92 Cornwall Air Quality Action Plan 2 Updated November 2020 Information Classification: PUBLIC Camelford AQMA 102 Grampound AQMA 112 Launceston AQMA 122 Cornwall Air Quality Action Plan 3 Updated November 2020 Information Classification: PUBLIC Policy Context Local Air Quality Management (LAQM) Section 82 of the Environment Act 1995 provides that every local authority shall review the air quality within its area, both at the present time and the likely future air quality. -

The London Gazette, 13Th June 1986 7975
THE LONDON GAZETTE, 13TH JUNE 1986 7975 port, both in the county of Greater Manchester. Court . TRURO. No. of Matter—1 of 1984. Truste's' T^ame, -^STOCKPORT. No. of Matter—51 of 1984. Trustee's Address and Descrition—Official Receiver, 1st Floor, 63 Name, Address and Description—Official Receiver, Town- New George Street, Plymouth, Devon PL1 1RD; Date bury House, 11 Blackfriars. Street, Salford M3 SAB. of Release—2nd May 1986. -•"*; Date of Release—16th April 1986. COUTSOUBOS, Clifford Charles, of 32 Lodenek Avenue, HUDSON, John Henry, of Woodsmoor, Stockport, BUIL- Padstow, Cornwall, SHARE FISHERMAN, lately resid- DER and DECORATOR, carrying on business under ing at 5 High Street, Padstow, Cornwall, formerly re- the title of Hudsons Builders Plumbers and Decorating siding at 23 Alan Road, Padstow, Cornwall, previously Contractors at Station Approach, Edgeley Side, Stock- residing at Fore Street, Newlyn, Penzance, Cornwall. port. Court-nSTOCKPORT. No. of Matter—1 of 1978. Court—TRURO. No. of Matter-^lA of 1984. Trustee's Trustee's Name, Address and Description—Freeman, Name, Address and Description—Official Receiver, *lst John A., 8 Manchester Road, Bury, Greater Manchester, Floor, 63 New George Street, Plymouth, Devon. Date Chartered Accountant. Date of Release—1st May 1986. of Release—2nd' May 1986. MARSH, Christopher, Builder's labourer, of the Old Post HILL, Stephen Roger,"Computer Assistant, of 11 Corona- Office, Church Lane, Maclesfield, in the county of Che- tion Place> Helston, Cornwall TR13 4AD, lately trading shire, formerly residing at 113 Edgeby Road, Stockport, with others as " Whitegate (Redruth) " at 26 Green Lane, hi the metropolitan county of Greater Manchester, and Redruth, Cornwall as DOUBLE GLAZING & KITCHEN ' JONES, Martin John, Warehouseman, of 27 Park Place, CONTRACTORS. -

Cornwall. Ive
DIRECTORY,] CORNWALL. IVE. 135 Rowe William, grocer ~LcCulloch James ~IcCulloch James, inventor & patentee Saunders Tom, watch maker, jeweller Polkinhorn Henry of the "Little Hercules" rock drill, & general smallware dealer COMMERCIAL. economic air compressor " Rio-Tin- Semmens William, greengrocer Bain, Son & Go. merchants & shipownrs to" & "Cornish" rock drills Serpell John, farmer Bellina Ellen (Mrs.), refreshment rms Penberthy James, shopkeeper Stephens Richard & Son, engineers Be·llina George, photographer Penhaul J oseph, blacksmith Stephens James John, pork butcher Blarney FrancisWilliams,apartments, & Portreath Harbour (D. W. Bain, Stoneman Edwd. Jn. carpente.r & bakr clerk! to school board manager for the Basset estate) Tregajorran Tin Streaming Co. (Jas. Camborne Unionist Association (C. H. Portreath Institute(J.R.Blight,hon.sec) J ewell, manager) Richards, sec) Rogers Thomas, apartments Thomas Charles, shopkeeper Chegwin Eliza (Mss), shopkeeper Russell John, sub-pilot Treglown A. & G. M. grocers, drapers Cock 1Villiam John, master mariner Seymour John, carrier & outfitters, cycle & emigration agts Corin Philip Burne, apartments, Sea Trathen William, carpenter Trevithick Elizabeth (Mrs.), shopkeepr View house, furnished, situated on Tregoning Mary Ann (Mrs.), coffee ho Trezise Stephen, tin streamer the North coast of Cornwall; exten- Vines Thos.Jas.chief coastguard o:ffi.cr Uren Richard, shoe maker sive sea & landscape views, inclosed WebsteT Emma (Mrs.), shopkeeper Williams Zacharias, farmer grounds ; & currier at Redruth PORTH -

NOTICE of POLL Notice Is Hereby Given That
Cornwall Council Election of a Unitary Councillor Altarnun Division NOTICE OF POLL Notice is hereby given that: 1. A poll for the election of a Unitary Councillor for the Division of Altarnun will be held on Thursday 4 May 2017, between the hours of 7:00 AM and 10:00 PM 2. The Number of Unitary Councillors to be elected is One 3. The names, addresses and descriptions of the Candidates remaining validly nominated and the names of all the persons signing the Candidates nomination papers are as follows: Name of Candidate Address Description Names of Persons who have signed the Nomination Paper Peter Russell Tregrenna House The Conservative Anthony C Naylor Robert B Ashford HALL Altarnun Party Candidate Antony Naylor Penelope A Aldrich-Blake Launceston Avril M Young Edward D S Aldrich-Blake Cornwall Elizabeth M Ashford Louisa A Sandercock PL15 7SB James Ashford William T Wheeler Rosalyn 39 Penpont View Labour Party Thomas L Hoskin Gus T Atkinson MAY Five Lanes Debra A Branch Jennifer C French Altarnun Daniel S Bettison Sheila Matcham Launceston Avril Wicks Patricia Morgan PL15 7RY Michelle C Duggan James C Sims Adrian Alan West Illand Farm Liberal Democrats Frances C Tippett William Pascoe PARSONS Congdons Shop Richard Schofield Anne E Moore Launceston Trudy M Bailey William J Medland Cornwall Edward L Bailey Philip J Medland PL15 7LS Joanna Cartwright Linda L Medland 4. The situation of the Polling Station(s) for the above election and the Local Government electors entitled to vote are as follows: Description of Persons entitled to Vote Situation of Polling Stations Polling Station No Local Government Electors whose names appear on the Register of Electors for the said Electoral Area for the current year. -

Ferndale, Chariot Road, Illogan Highway, Redruth, TR15 3LE OIEO £165,000
Modern And Light Ferndale, Chariot Road, Illogan Highway, Redruth, TR15 3LE OIEO £165,000 Perfect Investment Garage And Parking Well presented 3 bedroom property, offering comfortable living accommodation, front and back gardens along with a garage and off road parking. Convenient Location Property Description Goundrys are pleased to bring to the market this conveniently located, semi detached property. A light and generously sized living room welcomes you into this family home. From here you can access the first floor and the kitchen / dining room. The kitchen itself has been tastefully finished and offers a range of base, wall and drawers units along with an electric oven/hob. With ample dining space this room also provides further space for under counter appliances and a useful storage cupboard. Upstairs you will find three bedrooms (two doubles and one single) and the family bathroom. The bathroom benefits from having a modern suite, comprising of a hand wash basin, WC and shower over bath. Although buyers may want to imprint their own cosmetic impressions, this property has been well loved and cared for over the years and presents itself in good order throughout. Externally 'Ferndale' boasts having gardens to both front and back. The rear garden is fully enclosed and provides an area laid to lawn as well as a patio, directly off the kitchen. Perfect for some alfresco dining! While outside, you will also find the garage, and although the driveway serves the neighbouring property also, there is parking for multiple vehicles. To summarise, this is a wonderful opportunity to secure a well-presented family home with great links to the A30 and that's close to all the local amenities.