Immune and Inflammatory Cells of the Tumor Microenvironment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients
antibodies Review Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients Andrew T. Lucas 1,2,3,*, Ryan Robinson 3, Allison N. Schorzman 2, Joseph A. Piscitelli 1, Juan F. Razo 1 and William C. Zamboni 1,2,3 1 University of North Carolina (UNC), Eshelman School of Pharmacy, Chapel Hill, NC 27599, USA; [email protected] (J.A.P.); [email protected] (J.F.R.); [email protected] (W.C.Z.) 2 Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-919-966-5242; Fax: +1-919-966-5863 Received: 30 November 2018; Accepted: 22 December 2018; Published: 1 January 2019 Abstract: The rapid advancement in the development of therapeutic proteins, including monoclonal antibodies (mAbs) and antibody-drug conjugates (ADCs), has created a novel mechanism to selectively deliver highly potent cytotoxic agents in the treatment of cancer. These agents provide numerous benefits compared to traditional small molecule drugs, though their clinical use still requires optimization. The pharmacology of mAbs/ADCs is complex and because ADCs are comprised of multiple components, individual agent characteristics and patient variables can affect their disposition. To further improve the clinical use and rational development of these agents, it is imperative to comprehend the complex mechanisms employed by antibody-based agents in traversing numerous biological barriers and how agent/patient factors affect tumor delivery, toxicities, efficacy, and ultimately, biodistribution. -

Cutaneous Adverse Effects of Biologic Medications
REVIEW CME MOC Selena R. Pasadyn, BA Daniel Knabel, MD Anthony P. Fernandez, MD, PhD Christine B. Warren, MD, MS Cleveland Clinic Lerner College Department of Pathology Co-Medical Director of Continuing Medical Education; Department of Dermatology, Cleveland Clinic; of Medicine of Case Western and Department of Dermatology, W.D. Steck Chair of Clinical Dermatology; Director of Clinical Assistant Professor, Cleveland Clinic Reserve University, Cleveland, OH Cleveland Clinic Medical and Inpatient Dermatology; Departments of Lerner College of Medicine of Case Western Dermatology and Pathology, Cleveland Clinic; Assistant Reserve University, Cleveland, OH Clinical Professor, Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH Cutaneous adverse effects of biologic medications ABSTRACT iologic therapy encompasses an expo- B nentially expanding arena of medicine. Biologic therapies have become widely used but often As the name implies, biologic therapies are de- cause cutaneous adverse effects. The authors discuss the rived from living organisms and consist largely cutaneous adverse effects of tumor necrosis factor (TNF) of proteins, sugars, and nucleic acids. A clas- alpha inhibitors, epidermal growth factor receptor (EGFR) sic example of an early biologic medication is inhibitors, small-molecule tyrosine kinase inhibitors insulin. These therapies have revolutionized (TKIs), and cell surface-targeted monoclonal antibodies, medicine and offer targeted therapy for an including how to manage these reactions -

Avelumab (Bavencio®) Prior Authorization Drug Coverage Policy
1 Avelumab (Bavencio®) Prior Authorization Drug Coverage Policy Effective Date: 9/1/2020 Revision Date: n/a Review Date: 3/6/2020 Lines of Business: Commercial Policy type: Prior Authorization This Drug Coverage Policy provides parameters for the coverage of avelumab (Bavencio®). Consideration of medically necessary indications are based upon U.S. Food and Drug Administration (FDA) indications, recommended uses within the Centers of Medicare & Medicaid Services (CMS) five recognized compendia, including the National Comprehensive Cancer Network (NCCN) Drugs & Biologics Compendium (Category 1 or 2A recommendations), and peer-reviewed scientific literature eligible for coverage according to the CMS, Medicare Benefit Policy Manual, Chapter 15, section 50.4.5 titled, “Off-Label Use of Anti-Cancer Drugs and Biologics.” This policy evaluates whether the drug therapy is proven to be effective based on published evidence-based medicine. Drug Description 1-2 Avelumab is a fully human IgG1 monoclonal antibody that specifically binds to PD-L1. This binding blocks the interaction between PD-L1 and its receptors, PD-1 and B7.1. Blocking PD-1 and B7.1 interaction restores anti-tumor T-cell function. FDA Indications 1 Avelumab is FDA indicated for the following: Treatment of metastatic Merkel Cell carcinoma (MCC) in adults and children ≥ 12 years of age. Treatment of locally advanced or metastatic urothelial carcinoma in patients who have disease progression during or following platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. First-line treatment of advanced renal cell carcinoma (RCC) in combination with axitinib Coverage Determinations 1,3 Avelumab will require prior authorization. -

Bavencio; INN-Avelumab
10 December 2020 EMA/CHMP/3166/2021 Committee for Medicinal Products for Human Use (CHMP) Assessment report Bavencio International non-proprietary name: avelumab Procedure No. EMEA/H/C/004338/II/0018 Note Variation assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us An agency of the European Union Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 7 1.1. Type II variation ................................................................................................ 7 1.2. Steps taken for the assessment of the product ....................................................... 8 2. Scientific discussion ................................................................................ 9 2.1. Introduction ...................................................................................................... 9 2.1.1. Problem statement .......................................................................................... 9 2.1.2. About the product ........................................................................................... 9 2.1.3. The development programme/compliance with CHMP guidance/scientific -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -

Biosim™ Natalizumab (Tysabri®) (Human) ELISA
FOR RESEARCH USE ONLY! ™ BioSim Natalizumab (Tysabri®) (Human) ELISA Kit 07/20 (Catalog # E4856-100, 96 assays, Store at 4°C) I. Introduction: Natalizumab is a humanized IgG4k monoclonal antibody produced in murine myeloma cells. Natalizumab contains human framework regions and the complementarity-determining regions of a murine antibody that binds to a4-integrin. Natalizumab is used to treat multiple sclerosis-MS. It is thought to help by preventing patient’s immune system from attacking the nerves in the brain and spinal cord. Natalizumab is also used to treat a bowel condition called Crohn's disease (CD). BioSim™ Natalizumab ELISA kit has been developed for specific quantification of Natalizumab concentration in human serum or plasma with high sensitivity and reproducibility. Natalizumab ELISA kit is based on the sandwich ELISA principle. Standards and samples (serum or plasma) are added in the microtiter plate coated with the reactant for Natalizumab. After incubation, the wells are washed. The HRP conjugated probe is added and binds to Natalizumab captured by the reactant on the surface of the wells. Following incubation wells are washed and the bound enzymatic activity is detected by addition of TMB chromogen substrate. Finally, the reaction is terminated with an acidic stop solution. The color developed is proportional to the amount of Natalizumab in the sample or standard. Results of samples can be determined directly using the standard curve. II. Application: This ELISA kit is used for in vitro quantitative determination of Natalizumab Detection Range: 30 - 1000 ng/ml Sensitivity: 3 ng/ml Assay Precision: Intra-Assay: CV < 30%; Inter-Assay: CV < 30% (CV (%) = SD/mean X 100) Recovery rate: <100±30% with normal human serum samples with known concentrations Cross Reactivity: Except for Natalizumab, there is no cross reaction with other therapeutic antibodies and native serum immunoglobins. -
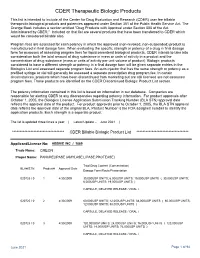
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Antibodies for the Treatment of Brain Metastases, a Dream Or a Reality?
pharmaceutics Review Antibodies for the Treatment of Brain Metastases, a Dream or a Reality? Marco Cavaco, Diana Gaspar, Miguel ARB Castanho * and Vera Neves * Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Av. Prof. Egas Moniz, 1649-028 Lisboa, Portugal * Correspondence: [email protected] (M.A.R.B.C.); [email protected] (V.N.) Received: 19 November 2019; Accepted: 28 December 2019; Published: 13 January 2020 Abstract: The incidence of brain metastases (BM) in cancer patients is increasing. After diagnosis, overall survival (OS) is poor, elicited by the lack of an effective treatment. Monoclonal antibody (mAb)-based therapy has achieved remarkable success in treating both hematologic and non-central-nervous system (CNS) tumors due to their inherent targeting specificity. However, the use of mAbs in the treatment of CNS tumors is restricted by the blood–brain barrier (BBB) that hinders the delivery of either small-molecules drugs (sMDs) or therapeutic proteins (TPs). To overcome this limitation, active research is focused on the development of strategies to deliver TPs and increase their concentration in the brain. Yet, their molecular weight and hydrophilic nature turn this task into a challenge. The use of BBB peptide shuttles is an elegant strategy. They explore either receptor-mediated transcytosis (RMT) or adsorptive-mediated transcytosis (AMT) to cross the BBB. The latter is preferable since it avoids enzymatic degradation, receptor saturation, and competition with natural receptor substrates, which reduces adverse events. Therefore, the combination of mAbs properties (e.g., selectivity and long half-life) with BBB peptide shuttles (e.g., BBB translocation and delivery into the brain) turns the therapeutic conjugate in a valid approach to safely overcome the BBB and efficiently eliminate metastatic brain cells. -

Avelumab) Name
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: 761049Orig1s009 Trade Name: Bavencio injection, for intravenous use Generic or Proper (avelumab) Name: Sponsor: EMD Serono Approval Date: June 30, 2020 Indication: For the maintenance treatment of patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed with first-line platinum-containing chemotherapy. CENTER FOR DRUG EVALUATION AND RESEARCH 761049Orig1s009 CONTENTS Reviews / Information Included in this NDA Review. Approval Letter X Other Action Letters Labeling X REMS Officer/Employee List Multidiscipline Review(s) X • Summary Review • Office Director • Cross Discipline Team Leader • Clinical • Non-Clinical • Statistical • Clinical Pharmacology • Clinical Microbiology/Virology Product Quality Review(s) X Other Reviews X Risk Assessment and Risk Mitigation Review(s) Proprietary Name Review(s) Administrative/Correspondence Document(s) CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761049Orig1s009 APPROVAL LETTER BLA 761049/S-009 SUPPLEMENT APPROVAL/ FULFILLMENT OF POSTMARKETING REQUIREMENT EMD Serono, Inc. Attention: Jennifer L. Stevens, JD Executive Director US Hub Lead/Global Regulatory Program Lead 45A Middlesex Turnpike Billerica, MA 01821 Dear Ms. Stevens: Please refer to your supplemental biologics license application dated April 7, 2020, received April 7, 2020, and your amendments, submitted under section 351(a) of the Public Health Service Act for Bavencio (avelumab) Injection. This Prior Approval supplemental biologics application provides for a new indication for the maintenance treatment of patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed with first-line platinum-containing chemotherapy. We also refer to your biologics license application (BLA) 761078, approved May 9, 2017, under the regulations at 21 CFR 601 Subpart E for Accelerated Approval of Biological Products for Serious or Life-Threatening Illnesses. -

Immune Checkpoint Inhibitors for the Treatment of Bladder Cancer
cancers Review Immune Checkpoint Inhibitors for the Treatment of Bladder Cancer Antonio Lopez-Beltran 1,*,† , Alessia Cimadamore 2,† , Ana Blanca 3, Francesco Massari 4 , Nuno Vau 5, Marina Scarpelli 2, Liang Cheng 6 and Rodolfo Montironi 2,* 1 Unit of Anatomic Pathology, Department of Morphological Sciences, Cordoba University Medical School, 14004 Cordoba, Spain 2 Pathological Anatomy, School of Medicine, United Hospitals, Polytechnic University of the Marche Region, 60126 Ancona, Italy; [email protected] (A.C.); [email protected] (M.S.) 3 Maimonides Biomedical Research Institute of Cordoba, Department of Urology, University Hospital of Reina Sofia, 14004 Cordoba, Spain; [email protected] 4 Division of Oncology, IRCCS Azienda Ospedaliero-Universitaria di Bologna, 40138 Bologna, Italy; [email protected] 5 Medical Oncology, Champalimaud Clinical Center, 1400-038 Lisbon, Portugal; [email protected] 6 Department of Pathology and Laboratory Medicine, School of Medicine, Indiana University, Indianapolis, IN 46202, USA; [email protected] * Correspondence: [email protected] or [email protected] (A.L.-B.); [email protected] (R.M.); Tel.: +34-9-5721-8992 (A.L.-B.); +39-0-71-596-4830 (R.M.); Fax: +34-9-5721-8229 (A.L.-B.) † These authors contributed equally to the work. Simple Summary: In this review, we examined relevant clinical trial results with immune check- point inhibitors in patients with metastatic urothelial cancer. We also focused on the potential of immunotherapy in the adjuvant and neoadjuvant setting or as part of drug combinations. Finally, we briefly review the current landscape of biomarkers of response to immune checkpoint inhibitors, such as programmed death-ligand 1 (PD-L1) expression, tumor mutation burden, molecular subtypes Citation: Lopez-Beltran, A.; of bladder cancer, and immune-gene expression profiling. -

Libtayo® (Cemiplimab-Rwlc)
Libtayo® (cemiplimab-rwlc) (Intravenous) -E- Document Number: IC-0473 Last Review Date: 07/01/2021 Date of Origin: 07/01/2019 Dates Reviewed: 07/2019, 10/2019, 01/2020, 04/2020, 07/2020, 10/2020, 01/2021, 04/2021, 07/2021 I. Length of Authorization Coverage will be provided for six months and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Libtayo 350 mg/7 mL single-use vial: 1 vial per 21 days B. Max Units (per dose and over time) [HCPCS Unit]: 350 billable units every 21 days III. Initial Approval Criteria 1 Coverage is provided for the following conditions: • Patient is at least 18 years of age; AND Universal Criteria 1 • Patient has not received previous therapy with a programmed death (PD-1/PD-L1)-directed therapy (e.g., avelumab, pembrolizumab, atezolizumab, durvalumab, nivolumab, dostarlimab, etc.), unless otherwise specified; AND • Used as single-agent therapy; AND • Patient has not received previous therapy with a cytotoxic T-lymphocyte antigen 4 (CTLA-4) targeting agent (e.g., ipilimumab, etc.) within the 4 weeks prior to therapy; AND • Patient does not have a history of a solid organ transplant; AND Cutaneous Squamous Cell Carcinoma (CSCC) † 1-5 • Patient has nodal or distant metastatic disease, locally advanced disease, inoperable or not fully resectable regional disease, or regional recurrence; AND • Patient is not a candidate for curative surgery or curative radiation therapy Basal Cell Carcinoma (BCC) † 1,2,6 • Patient has locally advanced OR nodal, regional, or distant metastatic disease; AND Moda Health Plan, Inc. Medical Necessity Criteria Page 1/10 Proprietary & Confidential © 2021 Magellan Health, Inc. -

BAVENCIO (Avelumab) RATIONALE for INCLUSION in PA PROGRAM
BAVENCIO (avelumab) RATIONALE FOR INCLUSION IN PA PROGRAM Background Bavencio (avelumab) is a programmed death ligand-1 (PD-L1) blocking antibody. This interaction releases the inhibitory effects of PD-L1 on the immune response resulting in the restoration of immune responses, including anti-tumor immune responses. Bavencio has also been shown to induce antibody-dependent cell-mediated cytotoxicity (ADCC) in vitro (1). Regulatory Status FDA-approved indications: Bavencio is a programmed death ligand-1 (PD-L1) blocking antibody indicated for: 1. Merkel Cell Carcinoma (MCC) a. Adults and pediatric patients 12 years and older with metastatic Merkel cell carcinoma (MCC) 2. Urothelial Carcinoma (UC) a. Maintenance treatment of patients with locally advanced or metastatic UC that has not progressed with first-line platinum-containing chemotherapy b. Patients with locally advanced or metastatic urothelial carcinoma who: i. Have disease progression during or following platinum-containing chemotherapy ii. Have experienced disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy 3. Renal Cell Carcinoma (RCC) a. First-line treatment, in combination with axitinib, of patients with advanced renal cell carcinoma (RCC) Bavencio can cause immune-mediated pneumonitis, hepatitis, colitis, and nephritis. Monitor patients for signs and symptoms of these adverse reactions and evaluate patients suspected of them. Discontinue Bavencio if the immune-mediated reactions become life-threatening (1). Bavencio can cause fetal harm when administered to a pregnant woman. Females of reproductive potential should use effective contraception while taking Bavencio and for one month after completion or discontinuation of therapy (1). Bavencio FEP Clinical Rationale BAVENCIO (avelumab) Bavencio in combination with axitinib can cause hepatotoxicity with higher than expected frequencies of Grade 3 and 4 ALT and AST elevation.