Increase Clean Faces! Decrease Flies!
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Activity Report 2017
INTERNATIONAL ACTIVITY REPORT 2017 www.msf.org THE MÉDECINS SANS FRONTIÈRES CHARTER Médecins Sans Frontières is a private international association. The association is made up mainly of doctors and health sector workers, and is also open to all other professions which might help in achieving its aims. All of its members agree to honour the following principles: Médecins Sans Frontières provides assistance to populations in distress, to victims of natural or man-made disasters and to victims of armed conflict. They do so irrespective of race, religion, creed or political convictions. Médecins Sans Frontières observes neutrality and impartiality in the name of universal medical ethics and the right to humanitarian assistance, and claims full and unhindered freedom in the exercise of its functions. Members undertake to respect their professional code of ethics and to maintain complete independence from all political, economic or religious powers. As volunteers, members understand the risks and dangers of the missions they carry out and make no claim for themselves or their assigns for any form of compensation other than that which the association might be able to afford them. The country texts in this report provide descriptive overviews of MSF’s operational activities throughout the world between January and December 2017. Staffing figures represent the total full-time equivalent employees per country across the 12 months, for the purposes of comparisons. Country summaries are representational and, owing to space considerations, may not be comprehensive. For more information on our activities in other languages, please visit one of the websites listed on p. 100. The place names and boundaries used in this report do not reflect any position by MSF on their legal status. -

NIGER: Carte Administrative NIGER - Carte Administrative
NIGER - Carte Administrative NIGER: Carte administrative Awbari (Ubari) Madrusah Légende DJANET Tajarhi /" Capital Illizi Murzuq L I B Y E !. Chef lieu de région ! Chef lieu de département Frontières Route Principale Adrar Route secondaire A L G É R I E Fleuve Niger Tamanghasset Lit du lac Tchad Régions Agadez Timbuktu Borkou-Ennedi-Tibesti Diffa BARDAI-ZOUGRA(MIL) Dosso Maradi Niamey ZOUAR TESSALIT Tahoua Assamaka Tillabery Zinder IN GUEZZAM Kidal IFEROUANE DIRKOU ARLIT ! BILMA ! Timbuktu KIDAL GOUGARAM FACHI DANNAT TIMIA M A L I 0 100 200 300 kms TABELOT TCHIROZERINE N I G E R ! Map Doc Name: AGADEZ OCHA_SitMap_Niger !. GLIDE Number: 16032013 TASSARA INGALL Creation Date: 31 Août 2013 Projection/Datum: GCS/WGS 84 Gao Web Resources: www.unocha..org/niger GAO Nominal Scale at A3 paper size: 1: 5 000 000 TILLIA TCHINTABARADEN MENAKA ! Map data source(s): Timbuktu TAMAYA RENACOM, ARC, OCHA Niger ADARBISNAT ABALAK Disclaimers: KAOU ! TENIHIYA The designations employed and the presentation of material AKOUBOUNOU N'GOURTI I T C H A D on this map do not imply the expression of any opinion BERMO INATES TAKANAMATAFFALABARMOU TASKER whatsoever on the part of the Secretariat of the United Nations BANIBANGOU AZEY GADABEDJI TANOUT concerning the legal status of any country, territory, city or area ABALA MAIDAGI TAHOUA Mopti ! or of its authorities, or concerning the delimitation of its YATAKALA SANAM TEBARAM !. Kanem WANZERBE AYOROU BAMBAYE KEITA MANGAIZE KALFO!U AZAGORGOULA TAMBAO DOLBEL BAGAROUA TABOTAKI TARKA BANKILARE DESSA DAKORO TAGRISS OLLELEWA -

Arrêt N° 01/10/CCT/ME Du 23 Novembre 2010
REPUBLIQUE DU NIGER Fraternité – Travail – Progrès CONSEIL CONSTITUTIONNEL DE TRANSITION Arrêt n° 01/10/CCT/ME du 23 novembre 2010 Le Conseil Constitutionnel de Transition statuant en matière électorale en son audience publique du vingt trois novembre deux mil dix tenue au Palais dudit Conseil, a rendu l’arrêt dont la teneur suit : LE CONSEIL Vu la proclamation du 18 février 2010 ; Vu l’ordonnance 2010-01 du 22 février 2010 modifiée portant organisation des pouvoirs publics pendant la période de transition ; Vu l’ordonnance n° 2010-031 du 27 mai 2010 portant code électoral et ses textes modificatifs subséquents ; Vu l’ordonnance n° 2010-038 du 12 juin 2010 portant composition, attributions, fonctionnement et procédure à suivre devant le Conseil Constitutionnel de Transition ; Vu le décret n° 2010-668/PCSRD du 1er octobre 2010 portant convocation du corps électoral pour le référendum sur la Constitution de la VIIème République ; Vu la requête en date du 8 novembre 2010 du Président de la Commission Electorale Nationale Indépendante (CENI) et les pièces jointes ; Vu l’ordonnance n° 003/PCCT du 8 novembre 2010 de Madame le Président du Conseil Constitutionnel portant désignation d’un Conseiller-Rapporteur ; Ensemble les pièces jointes ; Après audition du Conseiller – rapporteur et en avoir délibéré conformément à la loi ; EN LA FORME Considérant que par lettre n° 190/P/CENI en date du 8 novembre 2010, le Président de la Commission Electorale Nationale Indépendante (CENI) a saisi le Conseil Constitutionnel de Transition aux fins de valider -

F:\Niger En Chiffres 2014 Draft
Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 1 Novembre 2014 Le Niger en Chiffres 2014 Direction Générale de l’Institut National de la Statistique 182, Rue de la Sirba, BP 13416, Niamey – Niger, Tél. : +227 20 72 35 60 Fax : +227 20 72 21 74, NIF : 9617/R, http://www.ins.ne, e-mail : [email protected] 2 Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 Pays : Niger Capitale : Niamey Date de proclamation - de la République 18 décembre 1958 - de l’Indépendance 3 août 1960 Population* (en 2013) : 17.807.117 d’habitants Superficie : 1 267 000 km² Monnaie : Francs CFA (1 euro = 655,957 FCFA) Religion : 99% Musulmans, 1% Autres * Estimations à partir des données définitives du RGP/H 2012 3 Le Niger en Chiffres 2014 4 Le Niger en Chiffres 2014 Ce document est l’une des publications annuelles de l’Institut National de la Statistique. Il a été préparé par : - Sani ALI, Chef de Service de la Coordination Statistique. Ont également participé à l’élaboration de cette publication, les structures et personnes suivantes de l’INS : les structures : - Direction des Statistiques et des Etudes Economiques (DSEE) ; - Direction des Statistiques et des Etudes Démographiques et Sociales (DSEDS). les personnes : - Idrissa ALICHINA KOURGUENI, Directeur Général de l’Institut National de la Statistique ; - Ibrahim SOUMAILA, Secrétaire Général P.I de l’Institut National de la Statistique. Ce document a été examiné et validé par les membres du Comité de Lecture de l’INS. Il s’agit de : - Adamou BOUZOU, Président du comité de lecture de l’Institut National de la Statistique ; - Djibo SAIDOU, membre du comité - Mahamadou CHEKARAOU, membre du comité - Tassiou ALMADJIR, membre du comité - Halissa HASSAN DAN AZOUMI, membre du comité - Issiak Balarabé MAHAMAN, membre du comité - Ibrahim ISSOUFOU ALI KIAFFI, membre du comité - Abdou MAINA, membre du comité. -
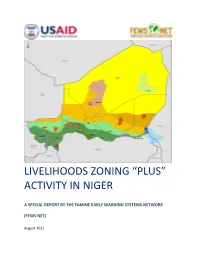
Livelihoods Zoning “Plus” Activity in Niger
LIVELIHOODS ZONING “PLUS” ACTIVITY IN NIGER A SPECIAL REPORT BY THE FAMINE EARLY WARNING SYSTEMS NETWORK (FEWS NET) August 2011 Table of Contents Introduction .................................................................................................................................................. 3 Methodology ................................................................................................................................................. 4 National Livelihoods Zones Map ................................................................................................................... 6 Livelihoods Highlights ................................................................................................................................... 7 National Seasonal Calendar .......................................................................................................................... 9 Rural Livelihood Zones Descriptions ........................................................................................................... 11 Zone 1: Northeast Oases: Dates, Salt and Trade ................................................................................... 11 Zone 2: Aïr Massif Irrigated Gardening ................................................................................................ 14 Zone 3 : Transhumant and Nomad Pastoralism .................................................................................... 17 Zone 4: Agropastoral Belt ..................................................................................................................... -

Niger Rural, Semi-Urban and Urban Electrification Project (Pepern)
AFRICAN DEVELOPMENT BANK GROUP NIGER Public Disclosure Authorized Authorized Disclosure Public RURAL, SEMI-URBAN AND URBAN ELECTRIFICATION PROJECT (PEPERN) ONEC DEPARTMENT Public Disclosure Authorized Authorized Disclosure Public November 2016 Translated Document TABLE OF CONTENTS 1 STRATEGIC ORIENTATION AND RATIONALE .................................................... 1 1.1 Project Linkages to Country Strategy and Objectives ............................................... 1 1.2 Rationale for Bank Involvement ............................................................................... 1 1.3 Aid Coordination ....................................................................................................... 2 2 PROJECT DESCRIPTION ............................................................................................. 2 2.1 Description of Project Components .......................................................................... 2 2.2 Technical Solutions Adopted and Alternative Solutions Considered ....................... 3 2.3 Project Type .............................................................................................................. 3 2.4 Project Cost and Financing Arrangements ................................................................ 3 2.5 Project Area and Beneficiaries .................................................................................. 5 2.6 Participatory Approach to Project Identification, Design and Implementation ........ 5 2.7 Bank Group Experience and Lessons Reflected in Project -

Profil Des Moyens D'existence Région De Zinder
Profil des moyens d’existence région de Zinder Magaria et Dungass – Zone agricole centrale de culture de céréales et des légumineuses Niger1 1 Ce profil a été réalisé en Mars 2016 dans la zone agricole des départements de Magaria et Dungass–région de Zinder. L’étude a touché particulièrement la zone centrale de culture de mil, sorgho, niébé, arachide et sésame. Les informations présentées font référence à l’année de consommation Octobre 2014– Septembre 2015. À l'exception de changements significatifs de moyens d’existence de la zone, ces informations auront une validité d’environ cinq à dix ans. Profil de Moyens d’Existence – Magaria agricole centrale – département de Magaria - Dungass, région de Zinder—Niger I. Contexte 1.1. Description de la zone Mars 2016 Le département de Magaria est situé au sud du Niger dans la région de Zinder. Il couvre une superficie de 8 434 km² et son chef-lieu est Magaria. Suite à la réforme administrative au Niger de 2011, le département de Magaria a été divisé en deux départements notamment le département de Magaria et Dungass. Le département de Magaria couvre dorénavant les communes rurales de Bandé, Dantchiao, Kwaya, Sassoumbroum, Wacha, Yékoua et a une population d’environ 718 440 habitants en 2016. Le nouveau département de Dungass couvre les communes rurales de Gouchi, Mallawa, Dungass et Dogo Dogo et une population estimée en 2016 à 440 044 habitants ce qui donne une densité d’environ 83 habitants par kilomètre carré. Les deux départements sont limités au nord par les départements de Matamèye et Mirriah, à l'Est par le département de Gouré, au Sud par le Nigéria et à l’Ouest par le département de Tessaoua. -

Niger - Région De Zinder - Département De Dungass Date De Production : 1 Février 2019
Pour Usage Humanitaire Uniquement CARTE DE REFERENCE Niger - Région de Zinder - Département de Dungass Date de production : 1 février 2019 9°0'0"E 9°30'0"E 10°0'0"E " " " " " " " " " " " " Rigal Dawon Meche "" Angoual Djibrin Kanwa Garin Bahari " " Garin Hardo Kodjo Madjiram Zabewa Damboa " Na Wash Kalle " Garin Moli Bekerya Mamandi Ii Afounori Hardori Manga Maina Moursouwa Ii Dogon Doutchi " Mamandi Iii " Garbia Gajammi " Kori Dayari I " Baban Zangon " " " Garin Gona Na Wash Kalle Lalachi " " Efadalen Rigal Zarbari" " " " Angoual Salifou " Tsam Guere (R.C.V) Mamandi I Madjiram Djamaare " " " Kanwa ( Rcv) Kori Dayari Ii " Rigal Tata Abdou " " Babban Riga " Janrouwa Jirgou " Kaikai " Chedou " Danganari " " Zongon Karami Angoual Talba Ii Angoual Talba I " Angoua" l Ali Garin Makera " Kona Bawada " " Idini " Garin Taila Mato " " " " Kolkoita Hamdara Hassanou Yacoubari Jetkori Garatchi " Zongon Garatchi " Gatchira Sofoua I " Mirriah " Mamandi Boukari " " Dineye Haoussa Garin Kandili Mamandi Kalili " Agama Oummata Illala Kaila Maitchabi Guidimouni " " Garin Malam Dan Maman " " Garin Dachi " Gouré "" " Dolkiri Kolleram " " Koel Gatchira Sofoua Ii " Matambey Tandou Mabam " " " " Garin Maman " Garin Kondio Keltamet " Illala Liman Souley Garin Chatima " Illala Abdou " Carre " Guinderi Garin Maigari Abdou Keltamat Gatchira Saboua " " Garin Galadima " Gamou Chimboua Daguilwa Garin Toudou Gadjerwa I-Ii " Gamdou " " Saleri Garin Chaibou " Tachibiri " " " " " Damagaram Takaya Boulamari Garin Kabiwa " " Kaguila Chirawa Zinder V " Din Di Pouss " Guegueri -

Niger – Food Insecurity
FACT SHEET #1, FISCAL YEAR (FY) 2011 SEPTEMBER 30, 2011 NIGER – FOOD INSECURITY KEY DEVELOPMENTS Following Niger’s food insecurity and acute malnutrition crisis of 2009/2010, food security in Niger generally improved in FY 2011 due to favorable rainfall and harvest patterns and increased grain price stabilization. The 2010 harvest produced an estimated 5.5 million metric tons (MT) of grain, approximately 40 percent above the five-year average. An evaluation of food security conditions conducted by Niger’s national early warning system in May and June 2011 found that approximately 2.3 million people in Niger were food-insecure, a 63 percent decrease from the same period in 2010. In addition, the quantity of food consumed in Niger remains at normal levels, despite an increase in demand due to the return of migrants from Libya, as a result of targeted food distributions to vulnerable households, according to the USAID-funded Famine Early Warning Systems Network (FEWS NET). Despite improved food security conditions in many areas, extreme weather events, including drought and floods, continue to negatively impact agricultural activities in many parts of Niger, as the majority of the predominantly agro- pastoral population relies on a single rainy season for crop cultivation and pasture renewal. Flooding in mid-August, for instance, affected nearly 14,000 people in Tillabéri and Maradi regions, destroying more than 100,000 hectares of crops and 1,000 houses, according to the U.N. Office for the Coordination of Humanitarian Affairs (OCHA). Due to improved food security and ongoing acute malnutrition relief interventions, the national prevalence of global acute malnutrition (GAM) among children under five years of age decreased to 12.3 percent as of July 2011, a decline from the prevalence of 16.7 percent in November 2010. -

Arrêt N° 18/09/CC/ME Du 27 Novembre 2009
REPUBLIQUE DU NIGER Fraternité -Travail- Progrès COUR CONSTITUTIONNELLE Arrêt N° 18/09/CC/ME du 27 novembre 2009 La Cour Constitutionnelle statuant en matière électorale sur l’éligibilité des listes de candidats présentées par les partis politiques et les indépendants, aux élections municipales du 27 décembre 2009, en son audience publique du 27 novembre tenue au palais de ladite Cour, a rendu l’arrêt dont la teneur suit pour la Région de ZINDER ; LA COUR Vu la Constitution ; Vu l’ordonnance n° 99-37 du 04 septembre 1999 portant Code Electoral et les textes modificatifs subséquents ; Vu la Loi n° 2000-11 du 14 août 2000 déterminant l’Organisation, le Fonctionnement et la Procédure à suivre devant la Cour Constitutionnelle, modifiée par les Lois numéros 001-2002 du 08 Février 2002 et 2004-16 du 13 Mai 2004 ; Vu la Loi n°98-31 du 14 septembre 1998 portant création des régions et fixant leurs limites et le nom de leurs chefs-lieux ; Vu la Loi n°98-32 du 14 septembre 1998 déterminant le statut des communautés urbaines ; Vu la Loi n° 2000-008 du 7 juin 2000 instituant le système de quota dans les fonctions électives, au Gouvernement et dans l’Administration de l’Etat ; Vu la Loi n°2001-023 du 10 août 2001 portant création des circonscriptions administratives et des collectivités territoriales et ses textes modificatifs subséquents ; Vu la Loi n°2002-14 du 11 juin 2002 portant création des communes et fixant le nom de leurs chefs-lieux et ses textes modificatifs subséquents ; Vu la Loi n°2002-012 du 11 juin 2002 déterminant les principes fondamentaux -

«Fichier Electoral Biométrique Au Niger»
«Fichier Electoral Biométrique au Niger» DIFEB, le 16 Août 2019 SOMMAIRE CEV Plan de déploiement Détails Zone 1 Détails Zone 2 Avantages/Limites CEV Centre d’Enrôlement et de Vote CEV: Centre d’Enrôlement et de Vote Notion apparue avec l’introduction de la Biométrie dans le système électoral nigérien. ▪ Avec l’utilisation de matériels sensible (fragile et lourd), difficile de faire de maison en maison pour un recensement, C’est l’emplacement physique où se rendront les populations pour leur inscription sur la Liste Electorale Biométrique (LEB) dans une localité donnée. Pour ne pas désorienter les gens, le CEV servira aussi de lieu de vote pour les élections à venir. Ainsi, le CEV contiendra un ou plusieurs bureaux de vote selon le nombre de personnes enrôlées dans le centre et conformément aux dispositions de création de bureaux de vote (Art 79 code électoral) COLLECTE DES INFORMATIONS SUR LES CEV Création d’une fiche d’identification de CEV; Formation des acteurs locaux (maire ou son représentant, responsable d’état civil) pour le remplissage de la fiche; Remplissage des fiches dans les communes (maire ou son représentant, responsable d’état civil et 3 personnes ressources); Centralisation et traitement des fiches par commune; Validation des CEV avec les acteurs locaux (Traitement des erreurs sur place) Liste définitive par commune NOMBRE DE CEV PAR REGION Région Nombre de CEV AGADEZ 765 TAHOUA 3372 DOSSO 2398 TILLABERY 3742 18 400 DIFFA 912 MARADI 3241 ZINDER 3788 NIAMEY 182 ETRANGER 247 TOTAL 18 647 Plan de Déploiement Plan de Déploiement couvrir tous les 18 647 CEV : Sur une superficie de 1 267 000 km2 Avec une population électorale attendue de 9 751 462 Et 3 500 kits (3000 kits fixes et 500 tablettes) ❖ KIT = Valise d’enrôlement constitués de plusieurs composants (PC ou Tablette, lecteur d’empreintes digitales, appareil photo, capteur de signature, scanner, etc…) Le pays est divisé en 2 zones d’intervention (4 régions chacune) et chaque région en 5 aires. -

Nutrition Causal Analysis in Niger
Nutrition Causal Analysis in Niger Report of Key Findings March 2017 This publication was prepared by Christine McDonald under the United States Agency for International Development Famine Early Warning Systems Network (FEWS NET) Indefinite Quantity Contract, AID-OAA-I-12-00006. The author’s views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development or the United States Government. FEWS NET NCA Research in Niger March 2017 Table of Contents List of Tables and Figures …………………………………………………………………………………………………………………..…………………… 2 Acronyms……...……………………………………………………………………………………………………………………………………………………….… 3 1. Executive Summary………………………………………………………………………………..…………………………………………………………. 4 2. Background……………………………………………………………………………………………………………………………………………………….. 6 3. Rationale for NCA Research.…………………………………………………….……………………………………………………………………….. 7 4. Scope and objectives of the NCA study in Maradi and Zinder.……………………..……………………………………………………. 8 5. Local collaboration……………..……………………………………………………………………………………………………..……………………… 8 6. Study setting.……………………..……………………………………………………….………………………………………………………………….… 9 7. Methodology………………………………………………………..……………………………………………………….……………………………….… 12 7.1 Study design and sample size calculations………………………………………..……………………………….…….………… 12 7.2 Sampling strategy………………………………………..………………………………………………………………………..………….. 12 7.3 Survey procedures………………………………………..……………………………………………………………………….………….. 13 7.4 Data entry and analysis………………………………………..………………………………………………………………….………… 14