Lens Epithelium Derived Growth Factor (1-326): A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Potential Applications of Curcumin and Curcumin Nanoparticles: from Traditional Therapeutics to Modern Nanomedicine
Nanotechnol Rev 2015; 4(2): 161–172 Review Mahendra Rai*, Raksha Pandit, Swapnil Gaikwad, Alka Yadav and Aniket Gade Potential applications of curcumin and curcumin nanoparticles: from traditional therapeutics to modern nanomedicine Abstract: Curcumin (diferuloylmethane) is one of the regions throughout the world and widely cultivated in potent, nontoxic, and major bioactive components pre- Asian countries, mostly in India and China [2, 3]. sent in turmeric. The major drawbacks of curcumin are Curcumin was isolated for the first time in 1815, while low absorption and poor bioavailability. The present its chemical structure was determined in 1973 by Rough- review highlights on the methods for the fabrication of ley and Whiting (Figure 1). The melting point of curcumin curcumin nanoparticles and their applications in treat- is 176–177°C, and it forms red to brown-colored salts when ment of cancer and wound infections. Curcumin nano- treated with alkalis [4]. Commercial curcumin possess particles possess remarkable antibacterial, antiviral, and approximately 77% diferuloylmethane, 17% demethoxy- antiprotozoan activity. Hence, curcumin nanoparticle- curcumin (Figure 2), and 6% bisdemethoxycurcumin [5] loaded nano-gel, microemulsion, and nano-cream can be (Figure 3). Curcumin is a natural compound, which is used for drug delivery. hydrophobic in nature. It consists of two polyphenolic rings, which are substituted by methoxy ether at the Keywords: antimicrobial activity; curcumin; curcumin ortho position, and tautomerization of curcumin arises nanoparticles. in a pH-dependent condition [6]; in neutral and acidic conditions, curcumin possesses a bis-keto form [1,7-bis (4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione]. DOI 10.1515/ntrev-2015-0001 Received January 2, 2015; accepted February 4, 2015; previously pub- Curcumin functions as an antioxidant, anti-inflamma- lished online March 19, 2015 tory, and anti-atherosclerotic. -

Undeclared Food Allergens and Gluten in Commercial Food Products Analyzed by ELISA
DOETAL.:JOURNAL OF AOAC INTERNATIONAL VOL. 101, NO. 1, 2018 23 SPECIAL GUEST EDITOR SECTION: FOOD ALLERGENS SURVEYS Undeclared Food Allergens and Gluten in Commercial Food Products Analyzed by ELISA 1 ANDREW B. DO,SEFAT E. KHUDA, and GIRDHARI M. SHARMA U.S. Food and Drug Administration, Center for Food Safety and Applied Nutrition, 8301 Muirkirk Rd, Laurel, MD 20708 Undeclared allergen(s) in commercial food patients avoid the consumption of packaged food products that products are responsible for many food recalls, as contain priority food allergens. In the United States, the Food reported by regulatory agencies in various Allergen Labeling and Consumer Protection Act (FALCPA) was countries, including the United States. Correct enacted in 2004, requiring specific declaration of the eight major allergen labeling practices are essential for the food allergens—egg, milk, peanut, soy, fish, crustacean safety of food-allergic consumers. However, this shellfish, tree nuts, and wheat—when added as ingredients in practice may be hindered by the introduction of labeled food products. Similar legislation also exists in other allergens all along the food supply chain, including countries or regions, such as Canada, Australia, New Zealand, unintentionally through cross-contact. To Japan, and the European Union (EU) (3). However, depending understand the pervasiveness of undeclared on the jurisdiction, additional food allergens, such as sesame, allergen(s) in commercial food products, the mustard, etc., also require declaration. More recently, in 2013, a objective of this review is to summarize the rule for the voluntary use of gluten-free labels on foods was prevalence of undeclared milk, egg, hazelnut, published in the United States. -

Sangram Kendra
Sangram Kendra District Taluka Village VLE Name Akola Akola AGAR PRAMOD R D Akola Akola AKOLA N KASHIRAM A Akola Akola AKOLA JP Shriram Mahajan Akola Akola AKOLA NW RP Vishal Shyam Pandey Akola Akola AKOLA NW RP-AC1 Vishal Shyam Pandey Akola Akola AKOLA OPP CO Dhammapal Mukundrao Umale Akola Akola AKOLA OPP CO-AC1 Dhammapal Mukundrao Umale Akola Akola AKOLA RP Rahul Rameshrao Deshmukh Akola Akola ANVI 2 Ujwala Shriram Khandare Akola Akola APATAPA Meena Himmat Deshmukh Akola Akola BABHULGAON A Jagdish Maroti Malthane Akola Akola BHAURAD MR Jagdish Gulabrao Deshmukh Akola Akola BORGAON M2 Amol Madhukar Ingale Akola Akola BORGAON MANJU N NARAYANRAO A Akola Akola DAHIHANDA RAJESH C T Akola Akola GANDHIGRAM Nilesh Ramesh Shirsat Akola Akola GOREGAON KD 2 Sandip Ramrao Mapari Akola Akola KANSHIVANI Pravin Nagorao Kshirsagar Akola Akola KASALI KHURD Kailash Shankar Shirsat Akola Akola KAULKHED RD DK Jyoti Amol Ambuskar Akola Akola KHADKI BU Kundan Ratangir Gosavi Akola Akola KHARAP BK Ishwar Bhujendra Bhati Akola Akola KOLAMBHI Amol Balabhau Badhe Akola Akola KURANKHED Sanjeevani Deshmukh Akola Akola MAJALAPUR Abdul Anis Abdul Shahid Akola Akola MALKAPUR V RAMRAO G Akola Akola MAZOD Sahebrao Ramkrushna Khandare Akola Akola MHAISANG Bhushan Chandrashekhar Gawande Akola Akola MHATODI Harish Dinkar Bhande Akola Akola MORGAON BHAK Gopal Shrikrishna Bhakare Akola Akola MOTHI UMRI A BHIMRAO KAPAL Akola Akola PALSO Siddheshwar Narayan Gawande Akola Akola PATUR NANDAPUR Atul Ramesh Ayachit Akola Akola RANPISE NAGAR Shubhangi Rajnish Thakare Akola Akola -

Graduation Ceremonies June 2015
GRADUATION CEREMONIES JUNE 2015 CONTENTS The Ceremonies: Morning Ceremony – Thursday 11 June 2015 at 10h00 ………………………………………..…........................4 Faculties of Commerce and Law Afternoon Ceremony – Thursday 11 June 2015 at 15h00 ………………………………………..…....................18 Faculties of Engineering & the Built Environment and Health Sciences Morning Ceremony – Friday 12 June 2015 at 10h00 …………………………………………............................38 Faculty of Commerce – The Graduate School of Business Afternoon Ceremony – Friday 12 June 2015 at 15h00 ………………………………………….........................44 Faculties of Humanities and Science 1 GAUDEAMUS Gaudeamus igitur, juvenes dum sumus, Gaudeamus igitur, juvenes dum sumus, Post jucundam juventutem, post molestam senectutem, Nos habebit humus, nos habebit humus. Ubi sunt qui ante nos in mundo fuere? Ubi sunt qui ante nos in mundo fuere? Vadite ad superos, transite ad inferos, Quos si vis videre, quos si vis videre. Vita nostra brevis est, brevi finietur, Vita nostra brevis est, brevi finietur, Venit mors velociter, rapit nos atrociter, Nemini parcetur, nemini parcetur. Vivat Academia, vivant Professores, Vivat Academia, vivant Professores, Vivat membrum quodlibet, vivant membra quaelibet, Semper sint in flore, semper sint in flore. 2 NATIONAL ANTHEM Nkosi sikelel’ iAfrika Maluphakanyisw’ uphondolwayo, Yizwa imithandazo yethu, Nkosi sikelela, thina lusapho lwayo. Morena boloka etjhaba sa heso, O fedise dintwa la matshwenyeho, O se boloke, O se boloke setjhaba sa heso, Setjhaba sa South Afrika – South Afrika. Uit die blou van onse hemel, Uit die diepte van ons see, Oor ons ewige gebergtes, Waar die kranse antwoord gee, Sounds the call to come together, And united we shall stand, Let us live and strive for freedom, In South Africa our land. 3 FACULTIES OF COMMERCE AND LAW ORDER OF PROCEEDINGS Academic Procession. -

MINUTES Date: Thursday, October 23Rd, 2014 Time: 3:30Pm-5:30Pm Location: Building 2 Room 10
Associated Students of Cañada College MINUTES Date: Thursday, October 23rd, 2014 Time: 3:30pm-5:30pm Location: Building 2 Room 10 Item Presenter/Time I. Call to Order a. Secretary: Andee Liljegren b. Time Keeper: Shawn Martin President Javier Santos calls the meeting to order at 3:31pm II. Roll Call (Quorum :7) President Santos/2 minutes __P___ Javier Santos __P___ Evelyn Bench __P___ Andee Liljegren __P___ Evelyn Valenzuela __P___ Shawn Martin __P___ Jithan Tennakoon __P___ Lina Tsvirkunova __P___ Carlos Lazarte __P___ Omar Gonzalez __P___ Claire Sharif __P___ Moody Metry __P___ Alexandra Wildman III. Adoption of The Agenda President Santos Only changes in the order of the agenda or removal of items from the agenda are allowed. Additions must be in compliance with The Brown Act. Vice-President Evelyn Valenzuela motions to adopt the agenda with the postponements of items 7a and 7b Senator Jithan Tennakoon seconds the motion Motion passes with unanimous consent Senator Andee Liljegren motions to amend the previous motion to include the postponements of items 10a and 10c Treasurer Lina Tsvirkunova seconds the amendment Motion passes with unanimous consent and the agenda is approved with the postponements of items 7a, 7b, 10a and 10c IV. Approval of The Minutes President Santos a. Thursday, October 16th,2014 Commissioner of Activities Claire Sharif motions to accept the minutes from October 16th Treasurer Lina Tsvirkunova seconds the motion Motion passes with unanimous consent V. Hearing of The Public Vice-President Valenzuela This time is reserved for the members of the public who wish to address the Associated Students of Cañada College on non- agenda items. -

Evaluation of Curcumin-Loaded Nanoliposomes for the Treatment and Prevention of Age-Related Macular Degeneration
1 American Psychology Association, 6th ed. ABSTRACT Title of Document: EVALUATION OF CURCUMIN-LOADED NANOLIPOSOMES FOR THE TREATMENT AND PREVENTION OF AGE-RELATED MACULAR DEGENERATION Sriramya Ayyagari, Haris Dar, Vivian Morton, Kevin Moy, Chadni Patel, Lalithasri Ramasubramanian, Nivetita Ravi, Samantha Wood, Andrew Zhao, Melanie Zheng, Kiet Zhou Directed by: Dr. Jose Helim Aranda-Espinoza Associate Professor, Fischell Department of Bioengineering University of Maryland, College Park Age-related macular degeneration (AMD), the most common cause of vision loss for people age 50 and over, is a disease characterized by the buildup of oxidative stress in the back of the eye. Current remedies are limited to intravitreal injections that only target the more severe ‘wet’ form; the common ‘dry’ form has no readily available pharmaceutical solution. Curcumin, a natural antioxidant found in the Indian spice turmeric, has shown potential in combating inflammatory diseases like AMD; however, the molecule also demonstrates poor bioavailability. This research aimed to create curcumin-loaded nanoliposomes (NLs) to be delivered noninvasively to potentially treat and prevent the onset of AMD. The 220 nm NLs were composed of phosphatidylcholine and cholesterol through vacuum evaporation, rehydration, and extrusion. Our curcumin- loaded NLs were assessed using an in vitro oxidative stress model of ARPE-19 cells. MTT cell viability assay results show that the liposomal curcumin complex has been able to improve cell viability with respect to the untreated cells (28% more viable, p < 0.05), 2 and cells that were damaged with peroxide (50% more viable, p < 0.05). As a preventative measure, the liposomal curcumin complex has been able to improve cell viability with respect to untreated cells (55% more viable, p < 0.05). -

Thermosensitive Drug Delivery System SBA-15-PEI for Controlled Release of Nonsteroidal Anti-Inflammatory Drug Diclofenac Sodium
materials Article Thermosensitive Drug Delivery System SBA-15-PEI for Controlled Release of Nonsteroidal Anti-Inflammatory Drug Diclofenac Sodium Salt: A Comparative Study Lubos Zauska 1, Stefan Bova 2, Eva Benova 1, Jozef Bednarcik 3 , Matej Balaz 4 , Vladimir Zelenak 1 , Virginie Hornebecq 5 and Miroslav Almasi 1,* 1 Department of Inorganic Chemistry, Faculty of Science, P. J. Šafárik University, Moyzesova 11, SK-041 01 Košice, Slovakia; [email protected] (L.Z.); [email protected] (E.B.); [email protected] (V.Z.) 2 BovaChem s.r.o, Garbiarska 1919/14, SK-048 01 Rožˇnava,Slovakia; [email protected] 3 Institute of Experimental Physics, Slovak Academy of Sciences, Watsonova 47, SK-040 01 Košice, Slovakia; [email protected] 4 Institute of Geotechnics, Slovak Academy of Sciences, Watsonova 45, SK-040 01 Košice, Slovakia; [email protected] 5 Aix-Marseille University, CNRS, MADIREL, F-133 97 Marseille, France; [email protected] * Correspondence: [email protected]; Tel.: +421 552-342-366 Abstract: Mesoporous SBA-15 silica material was prepared by the sol–gel method and functional- ized with thermosensitive polyethylenimine polymers with different molecular weight (g·mol−1): 800 (SBA-15(C)-800), 1300 (SBA-15(C)-1300) and 2000 (SBA-15(C)-2000). The nonsteroidal anti- Citation: Zauska, L.; Bova, S.; inflammatory drug (NSAID) diclofenac sodium was selected as a model drug and encapsulated Benova, E.; Bednarcik, J.; Balaz, M.; into the pores of prepared supports. Materials were characterized by the combination of infrared Zelenak, V.; Hornebecq, V.; Almasi, M. spectroscopy (IR), atomic force microscopy (AFM), transmission electron microscopy (TEM), photon Thermosensitive Drug Delivery cross-correlation spectroscopy (PCCS), nitrogen adsorption/desorption analysis, thermogravimetry System SBA-15-PEI for Controlled (TG), differential scanning calorimetry (DSC) and small-angle X-ray diffraction (SA-XRD) experi- Release of Nonsteroidal ments. -

Code Date Description Channel TV001 30-07-2017 & JARA HATKE STAR Pravah TV002 07-05-2015 10 ML LOVE STAR Gold HD TV003 05-02
Code Date Description Channel TV001 30-07-2017 & JARA HATKE STAR Pravah TV002 07-05-2015 10 ML LOVE STAR Gold HD TV003 05-02-2018 108 TEERTH YATRA Sony Wah TV004 07-05-2017 1234 Zee Talkies HD TV005 18-06-2017 13 NO TARACHAND LANE Zee Bangla HD TV006 27-09-2015 13 NUMBER TARACHAND LANE Zee Bangla Cinema TV007 25-08-2016 2012 RETURNS Zee Action TV008 02-07-2015 22 SE SHRAVAN Jalsha Movies TV009 04-04-2017 22 SE SRABON Jalsha Movies HD TV010 24-09-2016 27 DOWN Zee Classic TV011 26-12-2018 27 MAVALLI CIRCLE Star Suvarna Plus TV012 28-08-2016 3 AM THE HOUR OF THE DEAD Zee Cinema HD TV013 04-01-2016 3 BAYAKA FAJITI AIKA Zee Talkies TV014 22-06-2017 3 BAYAKA FAJITI AIYKA Zee Talkies TV015 21-02-2016 3 GUTTU ONDHU SULLU ONDHU Star Suvarna TV016 12-05-2017 3 GUTTU ONDU SULLU ONDU NIJA Star Suvarna Plus TV017 26-08-2017 31ST OCTOBER STAR Gold Select HD TV018 25-07-2015 3G Sony MIX TV019 01-04-2016 3NE CLASS MANJA B COM BHAGYA Star Suvarna TV020 03-12-2015 4 STUDENTS STAR Vijay TV021 04-08-2018 400 Star Suvarna Plus TV022 05-11-2015 5 IDIOTS Star Suvarna Plus TV023 27-02-2017 50 LAKH Sony Wah TV024 13-03-2017 6 CANDLES Zee Tamil TV025 02-01-2016 6 MELUGUVATHIGAL Zee Tamil TV026 05-12-2016 6 TA NAGAD Jalsha Movies TV027 10-01-2016 6-5=2 Star Suvarna TV028 27-08-2015 7 O CLOCK Zee Kannada TV029 02-03-2016 7 SAAL BAAD Sony Pal TV030 01-04-2017 73 SHAANTHI NIVAASA Zee Kannada TV031 04-01-2016 73 SHANTI NIVASA Zee Kannada TV032 09-06-2018 8 THOTAKKAL STAR Gold HD TV033 28-01-2016 9 MAHINE 9 DIWAS Zee Talkies TV034 10-02-2018 A Zee Kannada TV035 20-08-2017 -
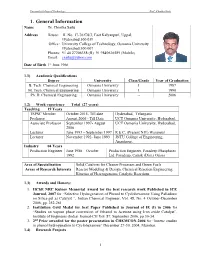
Dr.Chinta Sailu
University College of Technology Prof.. Chintha Sailu 1. General Information Name Dr. Chintha Sailu Address House: H. No. 17-76/C8/3, East Kalyanpuri, Uppal, Hyderabad 500 039 Office: University College of Technology, Osmania University Hyderabad 500 007 Phones: 91 40 27206358 (R) 91 9849636589 (Mobile) Email: [email protected] Date of Birth 1st June 1966 1.1) Academic Qualifications Degree University Class/Grade Year of Graduation B. Tech. Chemical Engineering Osmania University I 1987 M. Tech. Chemical Engineering Osmania University I 1990 Ph. D. Chemical Engineering Osmania University -- 2006 1.2) Work experience Total (27 years) Teaching 19 Years TSPSC Member October 2015- Till date Hyderabad, Telangana Professor August 2006 - Till Date UCT Osmania University, Hyderabad, Associate Professor September 1997- August UCT Osmania University, Hyderabad, 2006 Lecturer June 1993 – September 1997 R E C, (Present NIT) Warangal Lecturer November 1992- June 1993 JNTU College of Engineering, Anantapur, Industry 04 Years Production Engineer June 1988 – October Production Engineer, Paradeep Phasphates 1992 Ltd. Paradeep, Cuttak (Dist.) Orissa Area of Specialization Solid Catalysts for Cleaner Processes and Green Fuels Areas of Research Interests Reactor Modeling & Design, Chemical Reaction Engineering, Kinetics of Heterogeneous Catalytic Reactions 1.3) Awards and Honors: 1. IIChE NRC Kuloor Memorial Award for the best research work Published in ICE Journal, 2007 for “Selective Hydrogenation of Phenol to Cyclohexanone Using Palladium on Silica-gel as Catalyst “, Indian Chemical Engineer, Vol. 48, No. 4 October-December 2006, pp. 252-261 2. Institution Gold Medal for best Paper Published in Journal of IE (I) in 2006 for “Studies on vapour phase conversion of Ethanol to Acetone using Iron oxide Catalyst”. -

R19 M.Pharm. Pharmaceutical Regulatory Affairs Syllabus
R19 M.PHARM PHARMACEUTICAL REGULATORY AFFAIRS JAWAHARLAL NEHRU TECHNOLOGICAL UNIVERSITY HYDERABAD M.PHARMACY (PHARMACEUTICAL REGULATORY AFFAIRS) R19 COURSE STRUCTURE AND SYLLABUS Effective from Academic Year 2019-20 Admitted Batch I YEAR I Semester Course Code Course Title L T P Credits Professional Good Regulatory Practice 3 0 0 3 Core-I Professional Drug Regulatory Affairs 3 0 0 3 Core-II Professional 1. Intellectual Property Rights 3 0 0 3 Elective-I 2. Total Quality Management 3. Pharmaceutical Validation Professional 1. Stability of Drugs and Dosage forms 3 0 0 3 Elective-II 2. Pharmaceutical Formulation Technology 3. Documentation and Regulatory Writing Research methodology and IPR 2 0 0 2 Laboratory- I Regulatory Practice and Documentation Lab 0 0 4 2 Laboratory- II Drug Regulation and Registration Lab 0 0 4 2 Audit - I Audit Course - I 2 0 0 0 Total 16 0 8 18 I YEAR II Semester Course Code Course Title L T P Credits Professional Regulatory aspects of medical devices 3 0 0 3 Core-III Professional Regulatory aspects of herbals and biologicals 3 0 0 3 Core-IV Professional 1. Regulatory aspects of food and Nutraceuticals 3 0 0 3 Elective-III 2. Biostatistics and Research Methodology 3. Nano based Drug delivery systems Professional 1. Clinical research and Pharmacovigilance 3 0 0 3 Elective-IV 2. Nutraceuticals 3. Advanced Drug Delivery Systems Laboratory- III Regulatory aspects of herbals and biologicals Lab 0 0 4 2 Laboratory- IV Regulatory aspects of medical devices Lab 0 0 4 2 Mini Project with Seminar 2 0 0 2 Audit - II Audit Course - II 2 0 0 0 Total 16 0 8 18 1 R19 M.PHARM PHARMACEUTICAL REGULATORY AFFAIRS II YEAR I Semester Course Code Course Title L T P Credits Professional 1. -
LEE-THESIS-2014.Pdf (1.810Mb)
PEDIATRIC CARDIAC SURGERY IN DEVELOPING COUNTRIES OF AFRICA: CURRENT STATE AND FUTURE DIRECTION By K. BENJAMIN LEE Presented to the Faculty of the Medical School The University of Texas Southwestern Medical Center In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF MEDICINE WITH DISTINCTION IN GLOBAL HEALTH The University of Texas at Southwestern Medical Center Dallas, TX Pediatric Cardiac Surgery in Developing Countries of Africa: Current State and Future Direction K. Benjamin Lee The University of Texas Southwestern Medical Center International Medical Exchange Program 2012 - 2013 ABSTRACT: Surgical services are often the most neglected part of medical care in developing countries of Africa. Cardiac surgical care is even less accessible in comparison due to its need for highly skilled individuals and sophisticated equipment. This lack of proper care places the pediatric population affected by cardiac conditions without much hope for the future. Combining my clinical experience overseas with an extensive literature review, I examined the current state of pediatric cardiac surgery in several developing countries of Africa, and possible future efforts for establishing a viable cardiac surgery centers in low-resource settings. I examined in detail the two most prominent cardiac conditions in the developing world: congenital heart disease and rheumatic heart disease. The review of literature showed that cardiac surgical care is a serious need in many developing countries. It also revealed that with careful long-term international collaboration between institutions, a self-sustainable and economically viable cardiac surgical center with reasonable outcome can be established. i TABLE OF CONTENTS I. Introduction……………………………………………………………………………………..1 II. Cardiac Surgery in Africa………………………………………………………...……………2 III. -

(APP) Andhra Pradesh State Branch Organized a National Symposium On
ASU Vol. 2, No. 2 (Dec 2014) ASSOCIATION NEWS APP Telangana State Branch 2014 was announced during National Symposium on “Advances in Pharmaceutical Research” at Maheshwara rd Institute of Pharmacy, Patancheru, Hyderabad, Telangana on 23 July 2014. Association of Pharmacy Professionals (APP) Andhra Pradesh State Branch State branch was leaded by Dr. A. Muralidhar Rao, Principal & Professor, organized a National Symposium on “Advances in Pharmaceutical Maheshwara Institute of Pharmacy, Patancheru, Hyderabad as ‘PRESIDENT’; Research” at Maheshwara Institute of Pharmacy, Patancheru, Hyderabad, Dr. Palnati Narmada, Manager & HOD-Bioanalytical, Natco Research Centre, Telangana on 23rd July, 2014. Symposium was inaugurated by Dr. Rajiv Patancheru, Hyderabad as ‘VICE PRESIDENT’; Dr. Jithan Venkata Aukunuru, Dahiya, President APP and Principal, Globus College of Pharmacy, Principal & Professor, Mother Teresa College of Pharmacy, Rangareddy as Bangrasia, Bhojpur Road, Bhopal, Madhya Pradesh as Chief Guest and ‘SECRETARY’; Mr. Mohammed Omar, Vice Principal, Maheshwara Institute of Organizing Chairman; Dr. Jithan Venkata Aukunuru, Principal & Professor, Pharmacy, Patancheru, Hyderabad as ‘JOINT SECRETARY’; Dr. Shashidhar Mother Teresa College of Pharmacy, Rangareddy, Telangana as Guest of Purra, Associate Professor, Dept. of Pharmaceutics, Gland Institute of Honor; Dr. A. Muralidhar Rao, Principal & Professor, Maheshwara Institute Pharmaceutical Sciences, Shivampet, Medak as ‘JOINT SECRETARY’; Dr. D. of Pharmacy, Patancheru, Hyderabad, Telangana as Organizing Secretary. Ramakrishna, Professor, Dept. of Pharmacognosy, Sushrut Institute of During scientific session, Dr. Jithan V. Aukunuru delivered a lecture on the Pharmacy, Taddanpally, Pulkai, Medak as ‘EXECUTIVE MEMBER’ and Mr. topic ‘Parenteral Sustained Release Dosage Forms: Development with Chittumalla Ramesh, Asst. Professor, Dept. of Pharmaceutical Analysis, TRR Examples’. Dr. Aukunuru explained the fundamental requirements of College of Pharmacy, Patancheru, Medak as ‘EXECUTIVE MEMBER’.