And Galictis Cuja (Carnivora, Mustelidae): New Hosts in Chile
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
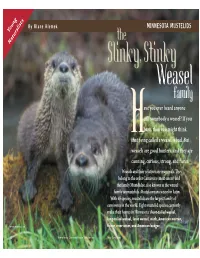
MINNESOTA MUSTELIDS Young
By Blane Klemek MINNESOTA MUSTELIDS Young Naturalists the Slinky,Stinky Weasel family ave you ever heard anyone call somebody a weasel? If you have, then you might think Hthat being called a weasel is bad. But weasels are good hunters, and they are cunning, curious, strong, and fierce. Weasels and their relatives are mammals. They belong to the order Carnivora (meat eaters) and the family Mustelidae, also known as the weasel family or mustelids. Mustela means weasel in Latin. With 65 species, mustelids are the largest family of carnivores in the world. Eight mustelid species currently make their homes in Minnesota: short-tailed weasel, long-tailed weasel, least weasel, mink, American marten, OTTERS BY DANIEL J. COX fisher, river otter, and American badger. Minnesota Conservation Volunteer May–June 2003 n e MARY CLAY, DEMBINSKY t PHOTO ASSOCIATES r mammals a WEASELS flexible m Here are two TOM AND PAT LEESON specialized mustelid feet. b One is for climb- ou can recognize a ing and the other for hort-tailed weasels (Mustela erminea), long- The long-tailed weasel d most mustelids g digging. Can you tell tailed weasels (M. frenata), and least weasels eats the most varied e food of all weasels. It by their tubelike r which is which? (M. nivalis) live throughout Minnesota. In also lives in the widest Ybodies and their short Stheir northern range, including Minnesota, weasels variety of habitats and legs. Some, such as badgers, hunting. Otters and minks turn white in winter. In autumn, white hairs begin climates across North are heavy and chunky. Some, are excellent swimmers that hunt to replace their brown summer coat. -

APROXIMACIÓN AL LENGUAJE REPERTORIAL DE LAS ESTEREOTIPIAS EN MAMIFEROS CARNIVOROS JAGUAR (Panthera Onca), GRISÓN (Galictis
APROXIMACIÓN AL LENGUAJE REPERTORIAL DE LAS ESTEREOTIPIAS EN MAMIFEROS CARNIVOROS JAGUAR (Panthera onca), GRISÓN (Galictis vittata) Y OCELOTE (Leopardus pardalis) DEL ZOOLOGICO GUATIKA, BOYACA – TIBASOSA. Laura Inés Monsalve Zuleta CÓDIGO:2014101101 Trabajo de investigación presentado como requisito parcial para optar al título de: Médica veterinaria especialista en Medicina Homeopática veterinaria Director (a): Néstor Alberto Calderón Maldonado Médico Veterinario – Universidad de la Salle Certificado en Medicina Veterinaria Homeopática – FICH “Luis G. Páez” Especialista en Bioética – Universidad El Bosque Fundación Universitaria Escuela Colombiana de Medicina Homeopática “Luis G. Páez”. Programa de Medicina Homeopática Veterinaria Bogotá, Colombia 2016 2 DEDICATORIA A mi familia, amigos y doctores que me apoyaron en esta etapa de mi vida tanto profesional como personal. 3 AGRADECIMIENTOS Agradezco a mi familia, amigos y Doctores que me ayudaron a culminar esta etapa de mi vida. 4 TABLA DE CONTENIDO: 1. RESUMEN ...................................................................................................................................... 7 2. INTRODUCCIÓN ........................................................................................................................... 8 3. JUSTIFICACIÓN ........................................................................................................................... 9 4. ESTADO DEL ARTE ................................................................................................................. -

Mammalia, Felidae, Canidae, and Mustelidae) from the Earliest Hemphillian Screw Bean Local Fauna, Big Bend National Park, Brewster County, Texas
Chapter 9 Carnivora (Mammalia, Felidae, Canidae, and Mustelidae) From the Earliest Hemphillian Screw Bean Local Fauna, Big Bend National Park, Brewster County, Texas MARGARET SKEELS STEVENS1 AND JAMES BOWIE STEVENS2 ABSTRACT The Screw Bean Local Fauna is the earliest Hemphillian fauna of the southwestern United States. The fossil remains occur in all parts of the informal Banta Shut-in formation, nowhere very fossiliferous. The formation is informally subdivided on the basis of stepwise ®ning and slowing deposition into Lower (least fossiliferous), Middle, and Red clay members, succeeded by the valley-®lling, Bench member (most fossiliferous). Identi®ed Carnivora include: cf. Pseudaelurus sp. and cf. Nimravides catocopis, medium and large extinct cats; Epicyon haydeni, large borophagine dog; Vulpes sp., small fox; cf. Eucyon sp., extinct primitive canine; Buisnictis chisoensis, n. sp., extinct skunk; and Martes sp., marten. B. chisoensis may be allied with Spilogale on the basis of mastoid specialization. Some of the Screw Bean taxa are late survivors of the Clarendonian Chronofauna, which extended through most or all of the early Hemphillian. The early early Hemphillian, late Miocene age attributed to the fauna is based on the Screw Bean assemblage postdating or- eodont and predating North American edentate occurrences, on lack of de®ning Hemphillian taxa, and on stage of evolution. INTRODUCTION southwestern North America, and ®ll a pa- leobiogeographic gap. In Trans-Pecos Texas NAMING AND IMPORTANCE OF THE SCREW and adjacent Chihuahua and Coahuila, Mex- BEAN LOCAL FAUNA: The name ``Screw Bean ico, they provide an age determination for Local Fauna,'' Banta Shut-in formation, postvolcanic (,18±20 Ma; Henry et al., Trans-Pecos Texas (®g. -

Predicting Greater Grison Galictis Vittata Presence from Scarce Records in the Department of Cordoba, Colombia
ORIGINAL CONTRIBUTION Predicting Greater Grison Galictis vittata presence from scarce records in the department of Cordoba, Colombia José F. GONZÁLEZ-MAYA1*, Julio J. CHACÓN PACHECO2, Javier RACERO-CASARRUBIA2, Erika HUMANEZ-LÓPEZ2 & Andrés ARIAS-ALZATE3 1. Proyecto de Conservación de Aguas y Tierras, ProCAT Colombia/Internacional, Calle 97ª # 10-62, Of. 202, Bogotá, Abstract. Colombia. The Greater Grison, Galictis vittata, is a poorly known species in Colombia. Throughout 2. Grupo de Investigación its range major knowledge gaps exist regarding its ecology and conservation. To compile Biodiversidad Unicórdoba, and analyse information about the species´ distribution records in the department of Universidad de Córdoba, Cordoba, Colombia and assess its presence probability according to landscape attributes, Montería, Córdoba, Colombia. we conducted a literature review of all wildlife studies in the region and compiled all possible direct presence records of the species in the department. We generated random 3.Grupo de Mastozoología, location points and characterized each distribution and random location by their distance to landscape attributes and land-cover type and modelled landscape presence using a Instituto de Biología, Multiple Logistic Regression approach. We found 33 records of the species in Cordoba Universidad de Antioquía. with most of the records distributed in the subregion of Alto Sinú (36%). Higher presence Medellín, Colombia. probabilities are localized in areas near forests mostly in the southern parts of the department, showing the species is still related with the largest forest blocks. Grisons Correspondence: appears to potentially tolerate some levels of disturbance but is still dependent to forest. The influence of natural habitats and abundance across the department and other areas José F. -

Controlled Animals
Environment and Sustainable Resource Development Fish and Wildlife Policy Division Controlled Animals Wildlife Regulation, Schedule 5, Part 1-4: Controlled Animals Subject to the Wildlife Act, a person must not be in possession of a wildlife or controlled animal unless authorized by a permit to do so, the animal was lawfully acquired, was lawfully exported from a jurisdiction outside of Alberta and was lawfully imported into Alberta. NOTES: 1 Animals listed in this Schedule, as a general rule, are described in the left hand column by reference to common or descriptive names and in the right hand column by reference to scientific names. But, in the event of any conflict as to the kind of animals that are listed, a scientific name in the right hand column prevails over the corresponding common or descriptive name in the left hand column. 2 Also included in this Schedule is any animal that is the hybrid offspring resulting from the crossing, whether before or after the commencement of this Schedule, of 2 animals at least one of which is or was an animal of a kind that is a controlled animal by virtue of this Schedule. 3 This Schedule excludes all wildlife animals, and therefore if a wildlife animal would, but for this Note, be included in this Schedule, it is hereby excluded from being a controlled animal. Part 1 Mammals (Class Mammalia) 1. AMERICAN OPOSSUMS (Family Didelphidae) Virginia Opossum Didelphis virginiana 2. SHREWS (Family Soricidae) Long-tailed Shrews Genus Sorex Arboreal Brown-toothed Shrew Episoriculus macrurus North American Least Shrew Cryptotis parva Old World Water Shrews Genus Neomys Ussuri White-toothed Shrew Crocidura lasiura Greater White-toothed Shrew Crocidura russula Siberian Shrew Crocidura sibirica Piebald Shrew Diplomesodon pulchellum 3. -

Galictis Cuja Molina, 1782) As Host of Dioctophyme Renale Goeze, 1782 Furão Pequeno (Galictis Cuja Molina, 1782) Como Hospedeiro De Dioctophyme Renale Goeze, 1782
ANIMAL PARASITOLOGY / SCIENTIFIC COMMUNICATION DOI: 10.1590/1808-1657000312016 Lesser Grison (Galictis cuja Molina, 1782) as host of Dioctophyme renale Goeze, 1782 Furão Pequeno (Galictis cuja Molina, 1782) como hospedeiro de Dioctophyme renale Goeze, 1782 Daniela Pedrassani1*, Mayana Worm1, Jéssica Drechmer1, Margareth Cristina Iazzetti Santos1 ABSTRACT: The Dioctophyme renale is a helminth parasite RESUMO: O Dioctophyme renale é um helminto parasita renal of the kidney usually seen in domestic and wild carnivores and observado normalmente em carnívoros domésticos e silvestres e rarely in human beings. This is a report about the parasitism excepcionalmente em seres humanos. Relata-se o parasitismo por D. of D. renale found in the kidney of two roadkill lesser grisons renale em rim de dois furões pequenos (Galictis cuja) encontrados (Galictis cuja) in the North of the state of Santa Catarina, mortos por atropelamento no Norte do estado de Santa Catarina, Brazil. The report of this parasitism in this species is important Brasil. Relatar esse parasitismo nessa espécie é importante, para to complement the records about this native carnivore as a que se possam somar dados relativos a participação deste carnívoro contributor in the epidemiologic chain while host/disseminator nativo na cadeia epidemiológica como hospedeiro/ veiculador desse of this helminth with zoonotic potential. helminto com potencial zoonótico. KEYWORDS: Dioctophyma; wild animal; mustelids; roadkill; PALAVRAS-CHAVE: Dioctophyma; animal silvestre; mustelí- kidney parasitism. deo; atropelamento em rodovia; parasitismo renal. 1Universidade do Contestado (UnC) – Canoinhas (SC), Brazil. *Corresponding author: [email protected] Received on: 04/22/2016. Accepted on: 09/12/2017 Arq. Inst. Biol., v.84, 1-4, e0312016, 2017 1 D. -

Mink: Wildlife Notebook Series
Mink The American mink (Neovison vison) and other fur bearing animals attracted trappers, traders, and settlers to Alaska from around the world. Some of the most valuable furbearers belong to the Mustelidae or weasel family, which includes the American mink. Other members of this family in Alaska include weasels, martens, wolverines, river otters, and sea otters. Mink are found in every part of the state with the exceptions of Kodiak Island, Aleutian Islands, the offshore islands of the Bering Sea, and most of the Arctic Slope. General description: A mink's fur is in prime condition when guard hairs are thickest. Mink are then a chocolate brown with some irregular white patches on the chin, throat, and belly. White patches are usually larger on females and often occur on the abdomen in the area of the mammary glands. Several albino mink have been reported from Alaska. Underfur is usually thick and wavy, not longer than an inch. It is dark gray to light brown in color with some suggestion of light and dark bands. The tail is one third to one fourth of the body length with slightly longer guard hairs than the body. As an adaptation to their aquatic lifestyle, their feet have semiwebbed toes and oily guard hairs tend to waterproof the animal. Adult males range in total length from 19 to 29 inches (48-74 cm). They may weigh from three to almost five pounds (1.4-2.3 kg). Females are somewhat smaller than males. Their movements are rapid and erratic as if they are always ready to either flee or pounce on an unwary victim. -

Notes on the Distribution, Status, and Research Priorities of Little-Known Small Carnivores in Brazil
Notes on the distribution, status, and research priorities of little-known small carnivores in Brazil Tadeu G. de OLIVEIRA Abstract Ten species of small carnivores occur in Brazil, including four procyonids, four mustelids (excluding otters), and two mephitids. On the IUCN Red List of Threatened Species eight are assessed as Least Concern and two as Data Deficient. The state of knowledge of small carnivores is low compared to other carnivores: they are among the least known of all mammals in Brazil. The current delineation of Bassaricyon and Galictis congeners appears suspect and not based on credible information. Research needs include understanding dis- tributions, ecology and significant evolutionary units, with emphasis on theAmazon Weasel Mustela africana. Keywords: Amazon weasel, Data Deficient, Olingo, Crab-eating Raccoon, Hog-nosed Skunk Notas sobre la distribución, estado y prioridades de investigación de los pequeños carnívoros de Brasil Resumen En Brasil ocurren diez especies de pequeños carnívoros, incluyendo cuatro prociónidos, cuatro mustélidos (excluyendo nutrias) y dos mephitidos. De acuerdo a la Lista Roja de Especies Amenazadas de la UICN, ocho especies son evaluadas como de Baja Preocupación (LC) y dos son consideradas Deficientes de Datos (DD). El estado de conocimiento de los pequeños carnívoros es bajo comparado con otros carnívoros y se encuentran entre los mamíferos menos conocidos de Brasil. La delineación congenérica actual de Bassaricyon y Galictis parece sospechosa y no basada en información confiable. Las necesidades de investigación incluyen el entendimiento de las distribuciones, ecología y unidades evolutivas significativas, con énfasis en la ComadrejaAmazónica Mustela africana. Palabras clave: Comadreja Amazónica, Deficiente de Datos, Mapache Cangrejero, Olingo, Zorrillo Introduction 1999), but recently has been recognised (e.g. -

A New Otter of Giant Size, Siamogale Melilutra Sp. Nov. \(Lutrinae
UCLA UCLA Previously Published Works Title A new otter of giant size, Siamogale melilutra sp. nov. (Lutrinae: Mustelidae: Carnivora), from the latest Miocene Shuitangba site in north-eastern Yunnan, south-western China, and a total- evidence phylogeny of lutrines Permalink https://escholarship.org/uc/item/11b1d0h9 Journal Journal of Systematic Palaeontology, 16(1) ISSN 1477-2019 Authors Wang, X Grohé, C Su, DF et al. Publication Date 2018-01-02 DOI 10.1080/14772019.2016.1267666 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Journal of Systematic Palaeontology ISSN: 1477-2019 (Print) 1478-0941 (Online) Journal homepage: http://www.tandfonline.com/loi/tjsp20 A new otter of giant size, Siamogale melilutra sp. nov. (Lutrinae: Mustelidae: Carnivora), from the latest Miocene Shuitangba site in north- eastern Yunnan, south-western China, and a total- evidence phylogeny of lutrines Xiaoming Wang, Camille Grohé, Denise F. Su, Stuart C. White, Xueping Ji, Jay Kelley, Nina G. Jablonski, Tao Deng, Youshan You & Xin Yang To cite this article: Xiaoming Wang, Camille Grohé, Denise F. Su, Stuart C. White, Xueping Ji, Jay Kelley, Nina G. Jablonski, Tao Deng, Youshan You & Xin Yang (2017): A new otter of giant size, Siamogale melilutra sp. nov. (Lutrinae: Mustelidae: Carnivora), from the latest Miocene Shuitangba site in north-eastern Yunnan, south-western China, and a total-evidence phylogeny of lutrines, Journal of Systematic Palaeontology, DOI: 10.1080/14772019.2016.1267666 To link to this article: http://dx.doi.org/10.1080/14772019.2016.1267666 View supplementary material Published online: 22 Jan 2017. Submit your article to this journal View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=tjsp20 Download by: [UCLA Library] Date: 23 January 2017, At: 00:17 Journal of Systematic Palaeontology, 2017 http://dx.doi.org/10.1080/14772019.2016.1267666 A new otter of giant size, Siamogale melilutra sp. -

Museum of Natural History
p m r- r-' ME FYF-11 - - T r r.- 1. 4,6*. of the FLORIDA MUSEUM OF NATURAL HISTORY THE COMPARATIVE ECOLOGY OF BOBCAT, BLACK BEAR, AND FLORIDA PANTHER IN SOUTH FLORIDA David Steffen Maehr Volume 40, No. 1, pf 1-176 1997 == 46 1ms 34 i " 4 '· 0?1~ I. Al' Ai: *'%, R' I.' I / Em/-.Ail-%- .1/9" . -_____- UNIVERSITY OF FLORIDA GAINESVILLE Numbers of the BULLETIN OF THE FLORIDA MUSEUM OF NATURAL HISTORY am published at irregular intervals Volumes contain about 300 pages and are not necessarily completed in any one calendar year. JOHN F. EISENBERG, EDITOR RICHARD FRANZ CO-EDIWR RHODA J. BRYANT, A£ANAGING EMOR Communications concerning purchase or exchange of the publications and all manuscripts should be addressed to: Managing Editor. Bulletin; Florida Museum of Natural Histoty, University of Florida P. O. Box 117800, Gainesville FL 32611-7800; US.A This journal is printed on recycled paper. ISSN: 0071-6154 CODEN: BF 5BAS Publication date: October 1, 1997 Price: $ 10.00 Frontispiece: Female Florida panther #32 treed by hounds in a laurel oak at the site of her first capture on the Florida Panther National Wildlife Refuge in central Collier County, 3 February 1989. Photograph by David S. Maehr. THE COMPARATIVE ECOLOGY OF BOBCAT, BLACK BEAR, AND FLORIDA PANTHER IN SOUTH FLORIDA David Steffen Maehri ABSTRACT Comparisons of food habits, habitat use, and movements revealed a low probability for competitive interactions among bobcat (Lynx ndia). Florida panther (Puma concotor cooi 1 and black bear (Urns amencanus) in South Florida. All three species preferred upland forests but ©onsumed different foods and utilized the landscape in ways that resulted in ecological separation. -

Curiosity in the American Black Bear
CURIOSITYIN THE AMERICANBLACK BEAR ELLISS. BACON,University of Tennessee, Instituteof Ecology,Townsend, TN 37882 Abstract: American black bears (Ursus americanus) were tested to quantify their response to novel objects placed in their environment. The results indicatethat the level of orientationmay be greaterin the black bear than in other North Americancarnivores. The explorationof objects by the black bear is characterizedby a high degree of contact with the objects. This contact consists primarilyof manipulatingthe objects with the forepaws and chewing the objects. The intense curiosity of the black bear should be recognized and consideredin the managementof this species and in the evaluation of bear/humanconflicts. Understand the behavior of an animal and its tive data on behaviors considered as curiosity were relationshipto its environmentis an importantconsid- lacking. eration in management of areas where humans and The curiosity of the bear had primarilybeen related bears come into frequent contact, but it is often over- by anecdotaland narrativeinformation. Everyone has a looked as a topic of research. The relationshipof game good story but no quantitative data. Several authors species to their environmentis usually studied in terms have noted that the bear exhibits a great deal of curios- of populationsand trends without consideringbehavior ity about humans and man-made objects. Leyhausen of individual animals. In practice, however, manage- (1948) and Burghardtand Burghardt(1972) described ment of large, solitary animals such as the black bear in young black bears manipulatingunfamiliar objects and a preserve situation is often on an individual level, food with both mouth and forepaws. Krott and Krott which requires an understandingof their behavior. -

Chewing and Sucking Lice As Parasites of Iviammals and Birds
c.^,y ^r-^ 1 Ag84te DA Chewing and Sucking United States Lice as Parasites of Department of Agriculture IVIammals and Birds Agricultural Research Service Technical Bulletin Number 1849 July 1997 0 jc: United States Department of Agriculture Chewing and Sucking Agricultural Research Service Lice as Parasites of Technical Bulletin Number IVIammals and Birds 1849 July 1997 Manning A. Price and O.H. Graham U3DA, National Agrioultur«! Libmry NAL BIdg 10301 Baltimore Blvd Beltsvjlle, MD 20705-2351 Price (deceased) was professor of entomoiogy, Department of Ento- moiogy, Texas A&iVI University, College Station. Graham (retired) was research leader, USDA-ARS Screwworm Research Laboratory, Tuxtia Gutiérrez, Chiapas, Mexico. ABSTRACT Price, Manning A., and O.H. Graham. 1996. Chewing This publication reports research involving pesticides. It and Sucking Lice as Parasites of Mammals and Birds. does not recommend their use or imply that the uses U.S. Department of Agriculture, Technical Bulletin No. discussed here have been registered. All uses of pesti- 1849, 309 pp. cides must be registered by appropriate state or Federal agencies or both before they can be recommended. In all stages of their development, about 2,500 species of chewing lice are parasites of mammals or birds. While supplies last, single copies of this publication More than 500 species of blood-sucking lice attack may be obtained at no cost from Dr. O.H. Graham, only mammals. This publication emphasizes the most USDA-ARS, P.O. Box 969, Mission, TX 78572. Copies frequently seen genera and species of these lice, of this publication may be purchased from the National including geographic distribution, life history, habitats, Technical Information Service, 5285 Port Royal Road, ecology, host-parasite relationships, and economic Springfield, VA 22161.