The Use of E-Health During the COVID-19 Pandemic: a Case Study in China’S Hubei Province
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

People's Republic of China: Hubei Enshi Qing River Upstream
Project Administration Manual Project Number: 47048-002 March 2020 People’s Republic of China: Hubei Enshi Qing River Upstream Environment Rehabilitation Contents ABBREVIATIONS iv I. PROJECT DESCRIPTION 1 II. IMPLEMENTATION PLANS 8 A. Project Readiness Activities 8 B. Overall Project Implementation Plan 9 III. PROJECT MANAGEMENT ARRANGEMENTS 12 A. Project Implementation Organizations – Roles and Responsibilities 12 B. Key Persons Involved in Implementation 15 C. Project Organization Structure 16 IV. COSTS AND FINANCING 17 A. Detailed Cost Estimates by Expenditure Category 19 B. Allocation and Withdrawal of Loan Proceeds 20 C. Detailed Cost Estimates by Financier 21 D. Detailed Cost Estimates by Outputs 22 E. Detailed Cost Estimates by Year 23 F. Contract and Disbursement S-curve 24 G. Fund Flow Diagram 25 V. FINANCIAL MANAGEMENT 26 A. Financial Management Assessment 26 B. Disbursement 26 C. Accounting 28 D. Auditing and Public Disclosure 28 VI. PROCUREMENT AND CONSULTING SERVICES 30 A. Advance Contracting and Retroactive Financing 30 B. Procurement of Goods, Works and Consulting Services 30 C. Procurement Plan 31 D. Consultant's Terms of Reference 40 VII. SAFEGUARDS 43 A. Environment 43 B. Resettlement 45 C. Ethnic Minorities 52 VIII. GENDER AND SOCIAL DIMENSIONS 53 A. Summary Poverty Reduction and Social Strategy 53 B. Gender Development and Gender Action Plan 53 C. Social Action Plan 54 IX. PERFORMANCE MONITORING, EVALUATION, REPORTING AND COMMUNICATION 61 A. Project Design and Monitoring Framework 61 B. Monitoring 68 C. Evaluation -

Silencing Complaints Chinese Human Rights Defenders March 11, 2008
Silencing Complaints Chinese Human Rights Defenders March 11, 2008 Chinese Human Rights Defenders (CHRD) Web: http://crd-net.org/ Email: [email protected] One World, One Dream: Universal Human Rights Silencing Complaints: Human Rights Abuses Against Petitioners in China A report by Chinese Human Rights Defenders In its Special Series on Human Rights and the Olympics Abstract As China prepares to host the Olympics, this report finds that illegal interception and arbitrary detention of petitioners bringing grievances to higher authorities have become more systematic and extensive, especially in the host city of the Olympic Games, Beijing. ―The most repressive mechanisms are now being employed to block the steady stream of petitioners from registering their grievances in Beijing. The Chinese government wants to erase the image of people protesting in front of government buildings, as it would ruin the meticulously cultivated impression of a contented, modern, prosperous China welcoming the world to the Olympics this summer,‖ said Liu Debo,1 who participated in the investigations and research for this report. Petitioners, officially estimated to be 10 million, are amongst those most vulnerable to human rights abuses in China today. As they bring complaints about lower levels of government to higher authorities, they face harassment and retaliation. Officially, the Chinese government encourages petitions and has an extensive governmental bureaucracy to handle them. In practice, however, officials at all levels of government have a vested interest in preventing petitioners from speaking up about the mistreatment and injustices they have suffered. The Chinese government has developed a complex extra-legal system to intercept, confine, and punish petitioners in order to control and silence them, often employing brutal means such as assault, surveillance, harassment of family members, kidnapping, and incarceration in secret detention centers, psychiatric institutions and Re-education through Labor camps. -

A Qualitative Study on the Judicial Social Services for Juvenile Delinquents Ningxin LIU Department of Sociology, Wuhan University of Technology, Wuhan, China
2020 2nd International Conference on Pedagogy, Communication and Sociology (ICPCS 2020) ISBN: 978-1-60595-663-3 A Qualitative Study on the Judicial Social Services for Juvenile Delinquents Ningxin LIU Department of Sociology, Wuhan University of Technology, Wuhan, China Keywords: juvenile delinquency, judicial social service, juvenile justice system Abstract. Juvenile delinquents have become one of the groups that gained much attention from society currently. The present situation and the changes attached to this group have become a significant social topic as well. Through the advance and improvement of the Criminal Law of the People’s Republic of China for the group of juvenile delinquents, the Department of Juvenile in many areas has applied the idea of "less arrestment and less litigation” to juvenile delinquents in the procuratorate system as a result of making more effort to provide the future development of juvenile delinquents. And based on this idea, more needs of judicial social services emerged in doing social inquiry reports and following-up monitoring to juvenile delinquents from government departments. This passage is based on the interview with the manager of Department of Juvenile of People's Procuratorate of Enshi City Hubei Province and one of the social workers in Siyecao Social Work Agency in Jingzhou City Hubei Province, and the analysis for the current situation of the judicial social services. And the corresponding suggestions offered in the passage are partially drawing on the experiences of previous studies and cases from other districts. 1. Introduction The revision of the documents published by the Supreme People's Procuratorate of the People's Republic of China showed changes in several aspects of the Juvenile Justice System. -

Table of Codes for Each Court of Each Level
Table of Codes for Each Court of Each Level Corresponding Type Chinese Court Region Court Name Administrative Name Code Code Area Supreme People’s Court 最高人民法院 最高法 Higher People's Court of 北京市高级人民 Beijing 京 110000 1 Beijing Municipality 法院 Municipality No. 1 Intermediate People's 北京市第一中级 京 01 2 Court of Beijing Municipality 人民法院 Shijingshan Shijingshan District People’s 北京市石景山区 京 0107 110107 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Haidian District of Haidian District People’s 北京市海淀区人 京 0108 110108 Beijing 1 Court of Beijing Municipality 民法院 Municipality Mentougou Mentougou District People’s 北京市门头沟区 京 0109 110109 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Changping Changping District People’s 北京市昌平区人 京 0114 110114 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Yanqing County People’s 延庆县人民法院 京 0229 110229 Yanqing County 1 Court No. 2 Intermediate People's 北京市第二中级 京 02 2 Court of Beijing Municipality 人民法院 Dongcheng Dongcheng District People’s 北京市东城区人 京 0101 110101 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Xicheng District Xicheng District People’s 北京市西城区人 京 0102 110102 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Fengtai District of Fengtai District People’s 北京市丰台区人 京 0106 110106 Beijing 1 Court of Beijing Municipality 民法院 Municipality 1 Fangshan District Fangshan District People’s 北京市房山区人 京 0111 110111 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Daxing District of Daxing District People’s 北京市大兴区人 京 0115 -

Summary Environmental Impact Assessment Yichang
SUMMARY ENVIRONMENTAL IMPACT ASSESSMENT YICHANG-WANZHOU RAILWAY PROJECT IN THE PEOPLE'S REPUBLIC OF CHINA June 2003 CURRENCY EQUIVALENTS (as of 31 May 2003) Currency Unit – Yuan (CNY) CNY1.00 = $0.1208 $1.00 = CNY8.277 ABBREVIATIONS ADB – Asian Development Bank CSRC – China Securities Regulatory Commission EIA – environmental impact assessment EPB – environmental protection bureau FABHP – Fisheries Administration Bureau of Hubei Province GDP – gross domestic product HICAS – Hydrobiology Institute of China Academy of Sciences MOR – Ministry of Railways NH – National Highway NOx – nitrogen oxides pH – measure of acidity/alkalinity PRC – People's Republic of China SEPA – State Environmental Protection Agency YNCZCS – Yichang Natural Conservation Zone for Chinese Sturgeon YWR – Yichang-Wanzhou Railway YRARI – Yangtze River Aquaculture Research Institute WEIGHTS AND MEASURES ° – degrees Celsius ha – hectare kg – kilogram km – kilometer m – meter mm – millimeter s – second t – ton y – year NOTE In this report, "$" refers to US dollars. CONTENTS Page Map 1 Map 2 Map 3 I. INTRODUCTION 1 II. DESCRIPTION OF THE PROJECT 1 III. DESCRIPTION OF THE ENVIRONMENT 2 A. Physical Resources 2 B. Ecological Resources 2 C. Human and Economic Development 4 D. Quality of Life Values 4 IV. ALTERNATIVES 6 V. ANTICIPATED ENVIRONMENTAL IMPACTS AND MITIGATION MEASURES 7 A. Noise 9 B. Water 10 C. Air 10 D. Solid Waste 11 E. Flora and Fauna 12 F. Historical, Cultural, and Archeological Sites 13 G. Resettlement 13 H. Safety and Health 14 I. Induced Impacts 14 VI. ECONOMIC ASSESSMENT 15 A. Environmental Protection Costs 15 B. Environmental Benefits 15 VII. INSTITUTIONAL REQUIREMENTS AND ENVIRONMENTAL MONITORING PROGRAM 16 VIII. PUBLIC PARTICIPATION 18 IX. -

Sustainable Sourcing : Markets for Certified Chinese
SUSTAINABLE SOURCING: MARKETS FOR CERTIFIED CHINESE MEDICINAL AND AROMATIC PLANTS In collaboration with SUSTAINABLE SOURCING: MARKETS FOR CERTIFIED CHINESE MEDICINAL AND AROMATIC PLANTS SUSTAINABLE SOURCING: MARKETS FOR CERTIFIED CHINESE MEDICINAL AND AROMATIC PLANTS Abstract for trade information services ID=43163 2016 SITC-292.4 SUS International Trade Centre (ITC) Sustainable Sourcing: Markets for Certified Chinese Medicinal and Aromatic Plants. Geneva: ITC, 2016. xvi, 141 pages (Technical paper) Doc. No. SC-2016-5.E This study on the market potential of sustainably wild-collected botanical ingredients originating from the People’s Republic of China with fair and organic certifications provides an overview of current export trade in both wild-collected and cultivated botanical, algal and fungal ingredients from China, market segments such as the fair trade and organic sectors, and the market trends for certified ingredients. It also investigates which international standards would be the most appropriate and applicable to the special case of China in consideration of its biodiversity conservation efforts in traditional wild collection communities and regions, and includes bibliographical references (pp. 139–140). Descriptors: Medicinal Plants, Spices, Certification, Organic Products, Fair Trade, China, Market Research English For further information on this technical paper, contact Mr. Alexander Kasterine ([email protected]) The International Trade Centre (ITC) is the joint agency of the World Trade Organization and the United Nations. ITC, Palais des Nations, 1211 Geneva 10, Switzerland (www.intracen.org) Suggested citation: International Trade Centre (2016). Sustainable Sourcing: Markets for Certified Chinese Medicinal and Aromatic Plants, International Trade Centre, Geneva, Switzerland. This publication has been produced with the financial assistance of the European Union. -
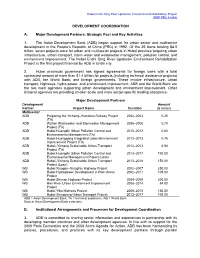
Development Coordination
Hubei Enshi Qing River Upstream Environment Rehabilitation Project (RRP PRC 47048) DEVELOPMENT COORDINATION A. Major Development Partners: Strategic Foci and Key Activities 1. The Asian Development Bank (ADB) began support for urban sector and multisector development in the People’s Republic of China (PRC) in 1992. Of the 39 loans totaling $4.5 billion, seven projects were for urban and multisector projects in Hubei province targeting urban infrastructure, urban transport, storm water and wastewater management, pollution control, and environment improvement. The Hubei Enshi Qing River Upstream Environment Rehabilitation Project is the first project financed by ADB in Enshi city. 2. Hubei provincial government has signed agreements for foreign loans with a total contracted amount of more than $1.4 billion for projects (including technical assistance projects) with ADB, the World Bank, and foreign governments. These involve infrastructure, urban transport, highways, hydro power, and environment improvement. ADB and the World Bank are the two main agencies supporting urban development and environment improvement. Other bilateral agencies are providing smaller-scale and more sector-specific lending assistance. Major Development Partners Development Amount Partner Project Name Duration ($ million) Multisector ADB Preparing the Yichang–Wanzhou Railway Project 2002–2003 0.25 (TA) ADB Wuhan Wastewater and Stormwater Management 2005–2006 0.70 Project (TA) ADB Hubei Huangshi Urban Pollution Control and 2010–2012 0.60 Environmental Management (TA) -

469 Stranded Residents Flown Home
4 | Friday, March 6, 2020 HONG KONG EDITION | CHINA DAILY CORONAVIRUSHK 469 stranded residents fl own home Virus on animal: More flights will be arranged to bring back the rest of HK people in Hubei Owners urged not By GU MENGYAN and HE SHUSI in Hong Kong to abandon pets A two-day operation to evacuate Hong Kong residents stranded in Hubei province — the epicenter of By CHEN ZIMO in Hong Kong the coronavirus epidemic — end- [email protected] ed on Thursday with a total of 469 evacuees flown home aboard four The government and The past month chartered flights arranged by the experts on Thursday urged saw no increase government. members of the public not to in animals being The operation, which began abandon their pets during the on Wednesday, saw a total of 225 outbreak of the novel coro- abandoned in the residents returning on two flights navirus — as no evidence yet city. There were on Thursday, joining 244 others suggests pets can be a source about 10 cases of who were brought back the previ- of COVID-19 infections. ous day. All the residents will be The appeal came after the this being report- quarantined for 14 days at Chun city reported the world’s fi rst ed each week, the Yeung Estate in Fo Tan district, case of an infected dog, which same as before the where more than 200 Hong Kong belongs to a COVID-19 patient. passengers evacuated from the The dog repeatedly tested pneumonia epi- Diamond Princess cruise ship in weak positive for the novel demic.’’ Japan last month were previously coronavirus beginning Feb the Society for the quarantined. -
Yichang to Badong Expressway Project
IPP307 v2 World Bank Financed Highway Project Yiba Expressway in Hubei·P. R. China YBE_05 Public Disclosure Authorized Public Disclosure Authorized Yichang to Badong Expressway Project Social Assessment Report Final Public Disclosure Authorized Public Disclosure Authorized The World Bank Financed Project Office of HPCD Social Survey Research Center of Peking University 22 September 2008 1 Preface Entrusted by the World Bank Financed Project Execution Office (PEO) under the Hubei Provincial Communications Department (HPCD), the Social Survey Research Center of Peking University (SSRCPKU) conducted an independent assessment on the “Project of the Stretch from Yichang to Badong of the Highway from Shanghai to Chengdu”. The Yiba stretch of the highway from Shanghai to Chengdu is lying in the west of Hubei Province which is at the joint of middle reaches and upper reaches of the Yangtze River. The project area administratively belongs to Yiling District Yichang City, Zigui County, Xingshang County and Badong County of Shien Tujia & Miao Autonomous Prefecture. It adjoins Jianghan Plain in the east, Chongqing City in the west, Yangtze River in the south and Shengnongjia Forest, Xiangfan City etc in the north. The highway, extending 173 km, begins in Baihe, connecting Jingyi highway, and ends up in Badong County in the joint of Hubei and Sichuan, joining Wufeng highway in Chongqing. Under the precondition of sticking to the World Bank’s policy, the social assessment is going to make a judgment of the social impact exerted by the project, advance certain measures, and in the meanwhile bring forward supervision and appraisement system. During July 1st and 9th, 2007, the assessment team conducted the social investigation in Yiling District Yichang City, Zigui County, XingshanCounty and Badong County. -

Sustainable Sourcing: Markets for Certified Chinese Medicinal and Aromatic Plants
SUSTAINABLE SOURCING: MARKETS FOR CERTIFIED CHINESE MEDICINAL AND AROMATIC PLANTS In collaboration with 5 - Markets for sustainably certified Chinese plan.pdf 1 2/10/2016 5:37:53 PM 5 - Markets for sustainably certified Chinese plan.pdf 2 2/10/2016 5:38:09 PM SUSTAINABLE SOURCING: MARKETS FOR CERTIFIED CHINESE MEDICINAL AND AROMATIC PLANTS 5 - Markets for sustainably certified Chinese plan.pdf 3 2/10/2016 5:38:09 PM SUSTAINABLE SOURCING: MARKETS FOR CERTIFIED CHINESE MEDICINAL AND AROMATIC PLANTS Abstract for trade information services ID=43163 2016 SITC-292.4 SUS International Trade Centre (ITC) Sustainable Sourcing: Markets for Certified Chinese Medicinal and Aromatic Plants. Geneva: ITC, 2016. xvi, 141 pages (Technical paper) Doc. No. SC-2016-5.E This study on the market potential of sustainably wild-collected botanical ingredients originating from the People’s Republic of China with fair and organic certifications provides an overview of current export trade in both wild-collected and cultivated botanical, algal and fungal ingredients from China, market segments such as the fair trade and organic sectors, and the market trends for certified ingredients. It also investigates which international standards would be the most appropriate and applicable to the special case of China in consideration of its biodiversity conservation efforts in traditional wild collection communities and regions, and includes bibliographical references (pp. 141–142). Descriptors: Medicinal Plants, Spices, Certification, Organic Products, Fair Trade, China, Market Research English For further information on this technical paper, contact Mr. Alexander Kasterine ([email protected]) The International Trade Centre (ITC) is the joint agency of the World Trade Organization and the United Nations. -

Short-Term Program International Education College of China University of Geosciences (Wuhan) Contents
SHORT-TERM PROGRAM INTERNATIONAL EDUCATION COLLEGE OF CHINA UNIVERSITY OF GEOSCIENCES (WUHAN) CONTENTS PART 1 PROGRAM OVERVIEW PART 2 PROFESSIONAL GEOLOGY FIELD PRACTICE PROGRAM PART 3 CHINESE LANGUAGE & REGIONAL CULTURE IMMERSION PROGRAM PART 4 CHINESE JEWELRY BUSINESS IMMERSION PROGRAM PART 5 PROFESSIONAL GEOGRAPHIC INFORMATION SYSTEM IMMERSION PROGRAM PART 6 PROFESSIONAL WILDERNESS SURVIVAL PROGRAM PROGRAM OVERVIEW PART 1 CHINA UNIVERSITY OF GEOSCIENCES (WUHAN) INTERNATIONAL EDUCATION COLLEGE The International Education College of China University of Geosciences (Wuhan) is a specialized institution dedicated to enhancing cultural Learning, Communication, exchanges, enrolling foreign students and offering Chinese language education programs. The IEC combines the functions of international Exploration, Enjoy... students education, Chinese language training, Confucius Institute construction and Sino-foreign education cooperation. The IEC has set up the Department of Chinese Language Training Center for Foreigners, International Student Affairs Office, Confucius Institute Office and Sino- foreign Education Cooperation Office. The IEC takes pride in having a history of over half a century of accepting international students since the 1950s. The IEC has the aim to cultivate high-level, interdisciplinary and outstanding international students as well as friendly messengers of cultural exchanges. The IEC has gradually established a comprehensive international talent cultivation system which focuses on language and culture communication, with -

Resettlement Monitoring Report PRC: Hubei Enshi Qing River Upstream
R esettlement Monitoring Report Project Number: 47048-002 March 2021 PRC: Hubei Enshi Qing River Upstream Environment Rehabilitation Project Prepared by: Shanghai Yiji Construction Consultants Co., Ltd. for the Asian Development Bank This resettlement monitoring report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. External Resettlement Monitoring Report #9 Semiannual Report for July-December 2020 March 2021 PRC: Hubei Enshi Qing River Upstream Environment Rehabilitation Project Prepared by Shanghai Yiji Construction Consultants Co., Ltd. for the Asian Development Bank CURRENCY EQUIVALENTS (As of 20 Oct. 2014) Currency Unit – yuan (CNY) CNY1 = $0.1634 $1 = CNY6.118 ABBREVIATION AAOV Average Annual Output Value ADB Asian Development Bank AH Affected HH AP Affected Person CNY Abbreviation for yuan, PRC’s currency DDR Due Diligence Report DI Design Institute DMS Detailed Measurement Survey EMA External Monitoring Agency ECPMO Enshi City Project Management Office EUCIC Enshi Urban Construction and Investment Co. Ltd. EPDRC Enshi Prefectural Development and Reform Commission EMDP Ethnic Minority Development Plan ERSM