Axial Ocular Dimensions and Corneal Astigmatism: the Kuala Pilah Cluster Cataract Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

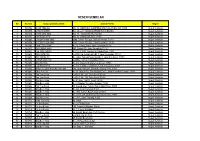
Negeri Ppd Kod Sekolah Nama Sekolah Alamat Bandar Poskod Telefon Fax Negeri Sembilan Ppd Jempol/Jelebu Nea0025 Smk Dato' Undang
SENARAI SEKOLAH MENENGAH NEGERI SEMBILAN KOD NEGERI PPD NAMA SEKOLAH ALAMAT BANDAR POSKOD TELEFON FAX SEKOLAH PPD NEGERI SEMBILAN NEA0025 SMK DATO' UNDANG MUSA AL-HAJ KM 2, JALAN PERTANG, KUALA KLAWANG JELEBU 71600 066136225 066138161 JEMPOL/JELEBU PPD SMK DATO' UNDANG SYED ALI AL-JUFRI, NEGERI SEMBILAN NEA0026 BT 4 1/2 PERADONG SIMPANG GELAMI KUALA KLAWANG 71600 066136895 066138318 JEMPOL/JELEBU SIMPANG GELAMI PPD NEGERI SEMBILAN NEA6001 SMK BAHAU KM 3, JALAN ROMPIN BAHAU 72100 064541232 064542549 JEMPOL/JELEBU PPD NEGERI SEMBILAN NEA6002 SMK (FELDA) PASOH 2 FELDA PASOH 2 SIMPANG PERTANG 72300 064961185 064962400 JEMPOL/JELEBU PPD NEGERI SEMBILAN NEA6003 SMK SERI PERPATIH PUSAT BANDAR PALONG 4,5 & 6, GEMAS 73430 064666362 064665711 JEMPOL/JELEBU PPD NEGERI SEMBILAN NEA6005 SMK (FELDA) PALONG DUA FELDA PALONG 2 GEMAS 73450 064631314 064631173 JEMPOL/JELEBU PPD BANDAR SERI NEGERI SEMBILAN NEA6006 SMK (FELDA) LUI BARAT BANDAR SERI JEMPOL 72120 064676300 064676296 JEMPOL/JELEBU JEMPOL PPD NEGERI SEMBILAN NEA6007 SMK (FELDA) PALONG 7 FELDA PALONG TUJUH GEMAS 73470 064645464 064645588 JEMPOL/JELEBU PPD BANDAR SERI NEGERI SEMBILAN NEA6008 SMK (FELDA) BANDAR BARU SERTING BANDAR SERI JEMPOL 72120 064581849 064583115 JEMPOL/JELEBU JEMPOL PPD BANDAR SERI NEGERI SEMBILAN NEA6009 SMK SERTING HILIR KOMPLEKS FELDA SERTING HILIR 4 72120 064684504 064683165 JEMPOL/JELEBU JEMPOL PPD NEGERI SEMBILAN NEA6010 SMK PALONG SEBELAS (FELDA) FELDA PALONG SEBELAS GEMAS 73430 064669751 064669751 JEMPOL/JELEBU PPD BANDAR SERI NEGERI SEMBILAN NEA6011 SMK SERI JEMPOL -
Executive Summary
Environmental Impact Assessment for Proposed Mixed Development of 136 Acre on Lots Executive S ummary 9164, 422 & 665, Mukim of Tampin Tengah, Tampin District, Negeri Sembilan Darul Khusus. Executive Summary 1. Introduction The Project is a proposed mixed development incorporating residential of low cost houses, individual lot houses, twin houses, super-link houses, commercial lots, club house, a mosque (surau) and primary kindergarten. The proposed Project covers a total area of approximately 136 acres (55.04 hectares). 2. Purpose of Preliminary Environmental Impact Assessment The EIA is prepared to fulfil the Malaysian legislative requirements. The proposed Project is categorised as a prescribed activity under item 7 of the First Schedule of the Environment Quality (Prescribed Activities) (Environmental Impact Assessment) Order, 1987: 7. Housing: (i) Housing development covering an area of 50 hectares or more Thus, this EIA report shall form the basis on which the environmental concerns related to the Project implementation shall be adequately addressed so that all potential impacts brought about by the Project can be monitored and controlled effectively, to ensure a safe and healthy working and also living environment for the surrounding community. 3. Statement of Need It is the local structure plan’s policy to pay attention especially in providing sufficient and affordable houses to the local people. The development by the Project Proponent will help achieve the intention of the government to achieve successful housing provision in the area, which will eventually create more affordable houses for the locals. Apart from that, the local council strategy is to have housing development that has good accessibility and mobility to town, recreational and offices. -

Negeri Sembilan
MALAYSIA LAPORAN SURVEI PENDAPATAN ISI RUMAH DAN KEMUDAHAN ASAS MENGIKUT NEGERI DAN DAERAH PENTADBIRAN HOUSEHOLD INCOME AND BASIC AMENITIES SURVEY REPORT BY STATE AND ADMINISTRATIVE DISTRICT NEGERI SEMBILAN 2019 Pemakluman/Announcement: Kerajaan Malaysia telah mengisytiharkan Hari Statistik Negara (MyStats Day) pada 20 Oktober setiap tahun. Tema sambutan MyStats Day 2020 adalah “Connecting The World With Data We Can Trust”. The Government of Malaysia has declared National Statistics Day (MyStats Day) on 20th October each year. MyStats Day theme is “Connecting The World With Data We Can Trust”. JABATAN PERANGKAAN MALAYSIA DEPARTMENT OF STATISTICS, MALAYSIA Diterbitkan dan dicetak oleh/Published and printed by: Jabatan Perangkaan Malaysia Department of Statistics, Malaysia Blok C6, Kompleks C Pusat Pentadbiran Kerajaan Persekutuan 62514 Putrajaya MALAYSIA Tel. : 03-8885 7000 Faks : 03-8888 9248 Portal : https://www.dosm.gov.my Facebook/Twitter/Instagram : StatsMalaysia Emel/Email : [email protected] (pertanyaan umum/general enquiries) [email protected] (pertanyaan & permintaan data/data request & enquiries) Harga/Price : RM30.00 Diterbitkan pada July 2020/Published on July 2020 Hakcipta terpelihara/All rights reserved. Tiada bahagian daripada terbitan ini boleh diterbitkan semula, disimpan untuk pengeluaran atau ditukar dalam apa-apa bentuk atau alat apa jua pun kecuali setelah mendapat kebenaran daripada Jabatan Perangkaan Malaysia. Pengguna yang mengeluarkan sebarang maklumat dari terbitan ini sama ada yang asal atau diolah semula hendaklah meletakkan kenyataan berikut: “Sumber: Jabatan Perangkaan Malaysia” No part of this publication may be reproduced or distributed in any form or by any means or stored in data base without the prior written permission from Department of Statistics, Malaysia. -

Title Some Observations on Adat and Adat Leadership in Rembau
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Some Observations on Adat and Adat Leadership in Rembau, Negeri Sembilan(<Special Issue>Socio-Economic Change and Title Cultural Transformation in Rural Malaysia : A Preliminary Research Report) Author(s) Norhalim Hj. Ibrahim Citation 東南アジア研究 (1988), 26(2): 150-165 Issue Date 1988-09 URL http://hdl.handle.net/2433/56328 Right Type Journal Article Textversion publisher Kyoto University Southeast Asian Studies, Vol. 26, No.2, September 1988 Some Observations on Adat and Adat Leadership in Rembau, Negeri Sembilan NORHALIM Hj. IBRAHIM* summarized. To some, the system is on its way out due to material advancement Introduction and its influence, which has penetrated the The Malays of N egeri Sembilan are char practising society at all levels since colonial acterized by a matrilineal custom and descent times and continues to do so under the group organization which they refer to as New Economic Policy of Malaysia today. the Adat Perpatih. The ada! is found To others, due to its unique internal char almost exclusively in N egeri Sembilan.I' acteristics, the system is being modified in The people of N egeri Sembilan claim that its practical aspects but philosophically re the Adat Perpatih originated in West Su mains intact. Analysis in depth shows that matra and was subsequently brought to to some extent both views are correct. N egeri Sembilan by Minangkabau immi- The name N egeri Sembilan means "nine grants. states." It refers to the fact that, prior to Due to its unique sociopolitical organiza European contact, Negeri Sembilan was a tion, N egeri Sembilan has, since the earlier confederacy of minor states (luak) with in part of the nineteenth century, been the dependent chiefs (penghulu or undang). -
Negeri Sembilan
NEGERI SEMBILAN Bil No. Est. Nama syarikat/ pemilik Alamat Premis Negeri 1 W00594 CHAN YING SAI NO. 54, LORONG 3, KAMPONG RATA,JALAN BAHAU, 72100 Negeri Sembilan 2 W00595 CHIN HON KEE NO. 26 & 27 TAMAN SORNAM,72100 BAHAU Negeri Sembilan 3 W00596 CHEW ANG NGA NO. 11, TAMAN SATELIT,72100 Negeri Sembilan 4 W00597 CHEW AH LEEK NO. 32 TAMAN SATELIT,72100 Negeri Sembilan 5 W00667 CHEOH THIAN SING 6296, Taman PD Jaya,Jalan Seremban, 71010 Negeri Sembilan 6 W00668 CHEOH THIAN SING 6297, Taman PD Jaya, Jalan Seremban, 71010 Negeri Sembilan 7 W00669 PANG KOK SUNG No 19, Taman Naga, Jalan Seremban,71010 Negeri Sembilan 8 W00670 SIA CHENG KION 567, Taman PD, Jalan Seremban,71010 Negeri Sembilan 9 W00671 LEE POH CHUAN N0. 2, Lot 6005,Taman Tun Sambanthan,71010 Negeri Sembilan 10 W00672 DEE SONG FEI Lot 74B, Kg. Kuala Lukut,Bt. 3, Jalan Seremban ,71010 Negeri Sembilan 11 W00673 DEE SONG FEI No. 4968, Taman Pantai Mas,Bt. 2, Jalan Seremban ,71010 Negeri Sembilan 12 W00674 CHEOK KIAN SIN Lot 5742, Taman Pantai Mas,71000 Negeri Sembilan 13 W00684 Ong Yip Ming No.614, Oakland Commercial Center, 70300 Negeri Sembilan 14 W00685 Law Siong Deng No.17,Lot 4764, Jalan Nilam 2,Taman Jayamas 70300 Negeri Sembilan 15 W00686 Aeries PureBird Nest 9M) Sdn. Bhd 280, Jalan Haruan 1,Oakland Industrial Park,70300 Negeri Sembilan 16 W00687 Chan Poh Tat No 10, tingkat 1&2, Taman Bukit Emas, Jalan Seremban-Tampin, 70300 Negeri Sembilan 17 W00688 Yap Yew Siong Lot 5327,No. 233, Desa Resah,70000 Negeri Sembilan 18 W00689 Yap Yew Siong Lot 5327,No. -

Negeri Sembilan Bil
NEGERI SEMBILAN BIL. NAMA & ALAMAT SYARIKAT NO.TELEFON/FAX JURUSAN ACSAP CORP SDN BHD Tel: 06-6011929 DAGANGAN & 1 NO 58 & 59 JALAN S2 D36,REGENCY AVENUE SEREMBAN 2 CITY Fax: 06-6015936 KHIDMAT CENTRE,70300,SEREMBAN,NEGERI SEMBILAN,DARUL KHUSUS ADVANCE PACT SDN BHD Tel: 06-7652016 DAGANGAN & 2 HOSPITAL TUNKU JAAFAR,JALAN DR MUTHU,70300,SEREMBAN,NEGERI Fax: 06-7652017 KHIDMAT SEMBILAN,DARUL KHUSUS ALIMAN TRAVEL SDN BHD Tel: 06-6013001 3 416 GROUND FLOOR JALAN HARUAN 4,OAKLAND COMMERCIAL TEKNOLOGI Fax: 06-6013001 CENTER,70300,SEREMBAN,NEGERI SEMBILAN,DARUL KHUSUS APEX COMPUTER SERVICES SDN BHD Tel: 03-61877614 4 LOT 2, TINGKAT 2, IT MALL,,TERMINAL 1 SHOPPING CENTRE, JALAN TEKNOLOGI Fax: 03-61877615 LINTANG,70000,SEREMBAN,NEGERI SEMBILAN,DARUL KHUSUS AVILLION ADMIRAL COVE Tel: HOTEL & 5 BATU 5 1/2,JALAN PANTAI,71050,SIRUSA PORT DECKSON,NEGERI Fax: PELANCONGAN SEMBILAN,DARUL KHUSUS AVILLION PORT DICKSON Tel: 06-6476688 HOTEL & 6 BATU 3 JALAN PANTAI,,71000,PORT DICKSON,NEGERI SEMBILAN,DARUL Fax: 06-6464561 PELANCONGAN KHUSUS BABAU TECHNOLOGY SERVICE Tel: 06-4547162 7 NO 20 JALAN MASJID,PUSAT PERNIAGAAN BABAU,72100,BABAU,NEGERI TEKNOLOGI Fax: SEMBILAN,DARUL KHUSUS BAHAGIAN PEMBAHAGIAN TNB Tel: 8 LOT 176, JALAN BESAR,,73000,TAMPIN,NEGERI SEMBILAN,DARUL INFRASTRUKTUR Fax: KHUSUS BAHAGIAN PENJANAAN TNB Tel: 06-6471199 DAGANGAN & 9 SJ TUANKU JA'AFAR,,2600,PORT DICKSON,NEGERI SEMBILAN,DARUL Fax: KHIDMAT KHUSUS BAHAGIAN TEKNOLOGI PENDIDIKAN NEGERI SEMBILAN Tel: 06-6621929 10 KM 14 JALAN PANTAI,TELUK KEMANG,71050,PORT DICKSON,NEGERI TEKNOLOGI Fax: -

Minor and Trace Metals in Slurry Slime in Mined-Out Ponds in the Kinta Valley, Perak
Geological Society of Malaysia Annual Geological Conference 2001 June 2-3 2001, Pangkor Island, Perak Darul Ridzuan, Malaysia Minor and trace metals in slurry slime in mined-out ponds in the Kinta Valley, Perak CHOW WENG SUM Minerals and Geoscience Department Malaysia 201h Floor, Tabung Haji Building, Jalan Tun Razak, P.O.Box 11110, 50736 Kuala Lumpur Abstract: The Kinta Valley was renowned as the largest tin field in the world and up to 1989, there were 70,158 hectares of land under mining leases. Thereafter, the tin mining industry took a down-tum due to falling tin metal prices and what is left of the industry is now mined-out land with abundant abandoned ponds. Stretching from Pengkalan near lpoh to Kampar in the south over a distance of 42km, there is a total of 1,194 mined-out ponds. About 66.7% of these ponds have slurry slime at the pond bottoms, with thickness varying from O.lm to 7.0m. Many of these abandoned ponds are used for the rearing of fish and ducks, or are cultivated with lotus plants. Slime is occasionally admixed with tailing sand for agricultural purposes. As such, should the slime be contaminated with heavy metals the food chain will be affected. Slime from eight ponds in the Kinta Valley was tested for minor and trace metals. Most of the slime contained higher concentrations of uranium and other trace heavy metals such asSn, Hg, Sb, 8i and Cd as compared to the norm in the earth's crust or stream sediments. Amongst the eight test ponds, slime from Pond 881 contained relatively higher concentrations of minor, radioactive and trace metals. -

Senarai Premis Penginapan Pelancong : N.Sembilan
SENARAI PREMIS PENGINAPAN PELANCONG : N.SEMBILAN BIL. NAMA PREMIS ALAMAT POSKOD DAERAH 1 Avillion Port Dickson Batu 3, Jalan Pantai 71000 Port Dickson 2 Bayu Beach Resort 4 1/2 Miles, Jalan Pantai, Si Rusa 71050 Port Dickson 3 ACBE Hotel No 524-526, Lorong 12, Taman ACBE 72100 Bahau 4 Hotel Seri Malaysia Seremban Jalan Sg Ujong 70200 Seremban 5 Thistle Hotel Port Dickson KM 16, Jalan Pantai, Teluk Kemang 71050 Port Dickson 6 Hotel We Young 241E, 7 1/2 Miles, Jalan Pantai, Si Rusa 71050 Port Dickson 7 Casa Rachado Resort Tanjung Biru, Batu 10, Jalan Pantai, Si Rusa 71050 Port Dickson 8 Corus Paradise Resort Port Dickson 3.5KM, Jalan Pantai 71000 Port Dickson 9 Desa Inn Lot 745, Jalan Dato'Abdul Manap 72000 Kuala Pilah 10 Glory Beach Resort Batu 2, Jalan Seremban, Tanjung Gemuk 71000 Port Dickson 11 The Regency Tanjung Tuan Beach Resort 5th. Mile, Jalan Pantai, 71050 Port Dickson 12 Eagle Ranch Resort Lot 544, Batu 14, Jalan Pantai 71250 Port Dickson 13 Tampin Hotel SH29-32, Pekan Woon Hoe Kan 73000 Tampin 14 Bahau Hotel 8-11, Tingkat 2 & 3, Lorong 1, Taman ACBE 72100 Bahau 15 Seremban Inn Hotel No 39, Jalan Tuanku Munawir 70000 Seremban 16 Carlton Star Hotel 47, Jalan Dato'Sheikh Ahmad 70000 Seremban 17 Lido Hotel Batu 8, Jalan Pantai Teluk Kemang 71050 Port Dickson 18 Bougainvilla Resort NO. 1178, Batu 9, JLN KEMANG 12, Teluk Kemang 71050 Port Dickson 19 Kong Ming Hotel KM 13, Jalan Pantai, Teluk Kemang, Si Rusa 71050 Port Dickson 20 Beach Point Hotel Lot 2261, Batu 9, Jalan Pantai, Si Rusa 71000 Port Dickson 21 Hotel Seri Malaysia Port -

Kependudukan Negeri Sembilan
Maklumat Lanjut DOSM/DOSM.NEGERISEMBILAN/1.2020/SIRI 82 NEGERI SEMBILAN Negeri Sembilan meliputi keluasan Jelebu 6,645 km persegi atau 664,591 hektar. Ibu negeri bagi Negeri Sembilan adalah Kuala Jempol Bandar Seremban yang telah mendapat Seremban Pilah status “Bandaraya” pada 1 Januari Tampin 2020. Terdapat 7 daerah iaitu daerah Port Dickson Seremban, Jelebu, Jempol, Rembau, Rembau TK PENDUDUK Tampin, Kuala Pilah, dan Port Dickson. 387,822 1,162,644 KEPENDUDUKAN Jantina,('000) Anggaran jumlah penduduk di Negeri Sembilan pada tahun 2020 adalah 605.8 556.8 sebanyak 1.16 juta orang. Bagi bilangan Tempat Kediaman pula adalah Komposisi Kaum, (000) sebanyak 387 ribu. Bilangan lelaki lebih tinggi daripada perempuan iaitu 605.8 ribu orang dan B u m i p u t e r a 556.8 ribu orang. 663.4 Dari segi komposisi kaum, Bumiputera mencatatkan 663.4 ribu orang. Diikuti kaum Cina adalah sebanyak 244.6 ribu C i n a I n d i a L a i n - l a i n orang dan kaum India adalah 162.4 ribu 244.6 162.4 6.1 orang. Bagi kaum lain-lain mencatatkan Struktur Umur 6.1 ribu orang. Struktur umur untuk kumpulan 0-14 tahun menunjukkan 21.8% manakala 65+ kumpulan umur 65+ adalah sebanyak 0 - 14 8.2%. 15- 64 8.2% 21.8% 69.9% K e l a h i r a n Jangkaan hayat perempuan lebih tinggi Jangkaan Hayat 18,177 daripada lelaki iaitu 77.2 tahun dan 71.4 tahun. Kelahiran dan kematian, tahun K e m a t i a n 2018 masing-masing mencatatkan 18,177 ribu orang dan 7,298 ribu orang. -

Alamat Pejabat Jawatan Dan Nama Telefon/Emel
LEMBAGA HASIL DALAM NEGERI MALAYSIA DIREKTORI LHDNM ALAMAT PEJABAT JAWATAN DAN NAMA TELEFON/EMEL NEGERI SEMBILAN / MELAKA PEJABAT PENGARAH NEGERI PENGARAH T.T.: 06-2531910 SAMB.: 160500 MENARA HASIL MELAKA, TINGKAT 8, DATUK HASSIM B. SHAFIAI emel: [email protected] MITC, HANG TUAH JAYA, 75450 AYER KEROH, MELAKA SETIAUSAHA SAMB.: 160501 NURUL NABILA BT. AZIZ TEL. AM : 06-2858888 FAKS : 06-2531907 CAWANGAN SEREMBAN PENGARAH T.T.: 06-7665001 SAMB.: 160000 MENARA ZURICH, TINGKAT 15-23, MOHD ZAIKI BIN ARIFFIN emel: [email protected] NO.1 JALAN LINTANG, 70200 SEREMBAN, SETIAUSAHA SAMB.: 160001 NEGERI SEMBILAN JULIA BT. SIDEK TEL. AM : 06-7665000 TIMBALAN PENGARAH T.T.: 06-7665022 SAMB.: 160070 FAKS : 06-7625339 RUSLANY B. KAMARUDDIN emel: [email protected] PEGAWAI PERHUBUNGAN T.T.: 06-7665121 SAMB.: 160194 AWAM emel: [email protected] RADHI B. ABU BAKAR [email protected] CAWANGAN MELAKA PENGARAH T.T.: 06-2519911 SAMB.: 160700 MENARA HASIL MELAKA, HISHAM B. RUSLI emel: [email protected] MITC, HANG TUAH JAYA, 75450 AYER KEROH, SETIAUSAHA SAMB.: 160701 MELAKA FUSIAH BT. YUSOH TEL. AM : 06-2858888 TIMBALAN PENGARAH T.T. : 06-2858803 SAMB.: 160551 FAKS : 06-2327729 GHAZALI B. MOHD AMIN emel: [email protected] PEGAWAI PERHUBUNGAN T.T.: 06-2327737 SAMB.: 160772 AWAM emel: [email protected] MOHD HILMI B. SALLEH [email protected] CAWANGAN SIASATAN SEREMBAN PENGARAH T.T.: 06-7665046 SAMB.: 160400 MENARA ZURICH, TINGKAT 15, ROSMAN B. MOHAMAD emel: [email protected] NO.1 JALAN LINTANG, 70200 SEREMBAN, SETIAUSAHA SAMB.: 160401 NEGERI SEMBILAN SALINA BT. -

Klinik Perubatan Swasta Negeri Sembilan Sehingga Disember 2020
Klinik Perubatan Swasta Negeri Sembilan Sehingga Disember 2020 NAMA DAN ALAMAT KLINIK KLINIK SEREMBAN 300 Senawang Jaya 70450 Seremban, Negeri Sembilan KLINIK TEH HENG ONG SDN BHD 2633, Simpang Lukut Jalan Sepang 71010 Port Dickson KLINIK REMBAU 1014, Off Jalan Besar 71300 Rembau Negeri Sembilan KLINIK PAKAR KANAK-KANAK KIDDI CARE No. 293_G, Taman AST Jalan Sg. Ujung, 70200 Seremban Negeri Sembilan POLIKLINIK AMAN 74, Jalan Besar Pekan Nilai 71800 Nilai KLINIK BAKTI 149, Jalan Yam Tuan Raden 72000 Kuala Pilah, Negeri Sembilan KLINIK CARE4ME PT 12948, Jalan BBN 1/7D Putra Indah Bandar Baru Nilai 71800 Nilai, Negeri Sembilan KLINIK HEE, ANNANDAN & SIVA 4 Jalan Lintang 73400 Gemas, Negeri Sembilan KLINIK AMMANPAL 5799, Jalan TS 2/7G, Taman Semarak 2 71800 Nilai, Negeri Sembilan ALEEN MEDICAL CENTRE 519 Jalan Tuanku Antah 70100 Seremban Negeri Sembilan KLINIK HEE No. 32, Jalan Besar Batang Melaka 73300 Tampin, Negeri Sembilan KLINIK PAKAR ORTOPEDIK PHANG & WANITA YANG No. 48, Jalan Tunku Hassan 70000 Seremban, Negeri Sembilan KLINIK A.K. CHONG 57 Jalan Temiang (Grd Floor) 70200 Seremban, Negeri Sembilan KLINIK AISYAH DAN YUSOF B 25, KLIA Business Centre Jalan Pusat Niaga KLIA 2, Kuarters KLIA 71800 Nilai, Negeri Sembilan KLINIK HEE Bangunan UMNO, Gemencheh 73200 Tampin, Negeri Sembilan POLIKLINIK PERDANA & X-RAY PT 9924, Ground Floor & 1st Floor Jalan BBN 1/3 G, Putra Point Fasa II A, Bandar Baru Nilai 71800 Nilai, Negeri Sembilan KLINIK NAGIAH 137, Jalan Damai 72100 Bahau KELINIK LEE 124, Jalan Yam Tuan 72000 Kuala Pilah KLINIK RAMANI 2026 Taman Ria KM 4, Jalan Seremban 71000 Port Dickson KLINIK KHOO 2827, Jalan SJ 3/6A Seremban Jaya 70450 Seremban KLINIK LEE PT 4963, Jalan T/S 2/1 Taman Semarak, Nilai 71800 seremban KLINIK TAN & SURGERY 2742 Main Road 71200 Rantau KLINIK PANTAI Lot 2747, Jalan Besar 71200 Rantau Negeri Sembilan KLINIK CHUA No. -

The Emergence of Abandoned Paddy Fields in Negeri Sembilan, Malaysia
Southeast Asian Studies, Vol. 32, No.2, September 1994 The Emergence of Abandoned Paddy Fields in Negeri Sembilan, Malaysia Tsuyoshi KATO* Introduction William Maxwell, a well-known colonial civil servant of British Malaya, wrote about the Negeri Sembilan Malays of the 1880s in the following way: A purely agricultural life requires that the cultivator be satisfied with poor fare and that his style of living be simple, modest and economical. As satisfying these conditions the Malays of Negri Sembilan are an almost an ideal peasantry [sic]. Their methods of [rice] cultivation are excellent, they preserve their ancient habits and traditions and they are satisfied with little. [quoted in AR KP 1912: 4]1) Martin Lister, first British Superintendent of Negeri Sembilan, reported in 1888: The registration of gardens and paddy fields at so early a stage in the [colonial] administration of these States [districts of Negeri Sembilan] is a matter for congratulation, as both in Johol and Tampin, lands formerly abandoned have received immediate attention on the part of the owners, in consequence of this light taxation and of a feeling of shame on the part of the owners to ignore the property which has descended to them from their ancestors. [Lister 1888: 1365-1366] The District Officer of Kuala Pilah, Negeri Sembilan, noted in 1912: Still the Kuala Pilah Malay lives in a style, simple, modest and economical; . .. The men have no scope to become fishermen; little scope and no inclination to work for wages; they are padi planters first, secondly cultivators of kampong [garden] and beyond that nothing, unless one except a very few special callings such as lembaga [clan head], pawang [village magician], kathi [Islamic official], goldsmith, bullock-carter and so on.