Item 4.4 PRINCIPLES for DELIVERING out of HOURS UNSCHEDULED CARE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aroma Café & Gift Shop, Mellon Charles, AULTBEA, IV22 2JL Offers
Aroma Café & Gift Shop, Mellon Charles, AULTBEA, IV22 2JL Offers Over £495,000 REF: 57207 Located within the beautiful crofting community of Mellon Charles, close to the village of Aultbea, the Aroma Café and Gift Shop represent a unique lifestyle opportunity along with a successful and profitable business. Built around an original crofthouse, the building has significant local provenance. Owners accomodation of approximately 830 sq ft on the ground floor plus some additional upstairs space, can be created within the building and a pre-planning application advises "there are no other material planning considerations identified at this time that would prevent the granting of the permission." The property, which was purpose built in 2006, has two main income streams and currently trades for 7 months of the year, 6 days a week from 10am-5pm, leaving ample scope to increase profits. The Café, which seats around 32 covers, is finished in a bistro-style and provides a calm, contemporary atmosphere. A freestanding wood burning stove with bespoke Caithness Stone hearth provides an additional welcoming focal point. The Café also enjoys spectacular uninterrupted views across Loch Ewe, towards the Torridon mountains and the Islands of Harris and Lewis. The Café boasts a "Taste our Best" certificate and has featured in national newspaper reviews. As the current owners do not take a day to day role, the Café is presently operated by two full-time staff (one being the manager), supplemented by two part-time staff in the busiest part of the season. The Café offers light lunches, soups, snacks, beverages and an excellent range of home baking. -

Wester Ross Ros An
Scottish Natural Heritage Explore for a day Wester Ross Ros an lar Wester Ross has a landscape of incredible beauty and diversity Historically people have settled along the seaboard, sustaining fashioned by a fascinating geological history. Mountains of strange, themselves by combining cultivation and rearing livestock with spectacular shapes rise up from a coastline of diverse seascapes. harvesting produce from the sea. Crofting townships, with their Wave battered cliffs and crevices are tempered by sandy beaches small patch-work of in-bye (cultivated) fields running down to the or salt marsh estuaries; fjords reach inland several kilometres. sea can be found along the coast. The ever changing light on the Softening this rugged landscape are large inland fresh water lochs. landscape throughout the year makes it a place to visit all year The area boasts the accolade of two National Scenic Area (NSA) round. designations, the Assynt – Coigach NSA and Wester Ross NSA, and three National Nature Reserves; Knockan Crag, Corrieshalloch Symbol Key Gorge and Beinn Eighe. The North West Highland Geopark encompasses part of north Wester Ross. Parking Information Centre Gaelic dictionary Paths Disabled Access Gaelic Pronunciation English beinn bayn mountain gleann glyown glen Toilets Wildlife watching inbhir een-er mouth of a river achadh ach-ugh field mòr more big beag bake small Refreshments Picnic Area madainn mhath mat-in va good morning feasgar math fess-kur ma good afternoon mar sin leat mar shin laht goodbye Admission free unless otherwise stated. 1 11 Ullapool 4 Ullapul (meaning wool farm or Ulli’s farm) This picturesque village was founded in 1788 as a herring processing station by the British Fisheries Association. -
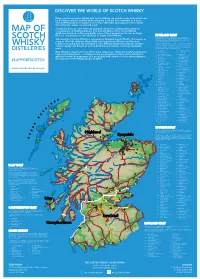
2019 Scotch Whisky
©2019 scotch whisky association DISCOVER THE WORLD OF SCOTCH WHISKY Many countries produce whisky, but Scotch Whisky can only be made in Scotland and by definition must be distilled and matured in Scotland for a minimum of 3 years. Scotch Whisky has been made for more than 500 years and uses just a few natural raw materials - water, cereals and yeast. Scotland is home to over 130 malt and grain distilleries, making it the greatest MAP OF concentration of whisky producers in the world. Many of the Scotch Whisky distilleries featured on this map bottle some of their production for sale as Single Malt (i.e. the product of one distillery) or Single Grain Whisky. HIGHLAND MALT The Highland region is geographically the largest Scotch Whisky SCOTCH producing region. The rugged landscape, changeable climate and, in The majority of Scotch Whisky is consumed as Blended Scotch Whisky. This means as some cases, coastal locations are reflected in the character of its many as 60 of the different Single Malt and Single Grain Whiskies are blended whiskies, which embrace wide variations. As a group, Highland whiskies are rounded, robust and dry in character together, ensuring that the individual Scotch Whiskies harmonise with one another with a hint of smokiness/peatiness. Those near the sea carry a salty WHISKY and the quality and flavour of each individual blend remains consistent down the tang; in the far north the whiskies are notably heathery and slightly spicy in character; while in the more sheltered east and middle of the DISTILLERIES years. region, the whiskies have a more fruity character. -

Strategic Transport Projects Review Report 1 – Review of Current and Future Network Performance
Transport Scotland Strategic Transport Projects Review Report 1 – Review of Current and Future Network Performance 7.2 Corridor 2: Inverness to Ullapool and Western Isles 7.2.1 Setting the Context Corridor 2 extends north and west from Inverness to northwest Scotland and includes onward connections to the Western Isles (Eilean Siar), as shown in Figure 7.2.1. It connects the city of Inverness with Ullapool, which are approximately 92 kilometres apart. Ullapool has an onward ferry connection to Stornoway. The population of the corridor (excluding Eilean Siar) is approximately 16,000 and little change is forecast over the period to 2022333. In contrast, the population of Eilean Siar is forecast to decline over this period by almost 15 per cent334. However the largest change in population overall, shown in Figure 7.2.2, is in and around Inverness. It is expected that there will be employment growth of approximately four per cent in the Highland council area as a whole, but a decline of similar magnitude in Eilean Siar335. Areas of greatest change are shown in Figure 7.2.2. The national level of car ownership, measured as a percentage of households with access to a car, is 67 per cent. Within the corridor, car ownership levels are above average, as expected, due to the rural nature of the corridor: • Highland council area: 75 per cent; and • Eilean Siar: 70 per cent336. The economic inactivity rate within the Highlands and Eilean Siar was around 16 per cent in 2005. This is slightly below the Scottish average of 21 per cent337. -
Caithness & Sutherland Report
www.hie.co.uk OUR NEXT GENERATION Young People in Caithness and Sutherland Attitudes and aspirations. Research report September 2015 TABLE OF CONTENTS 1 INTRODUCTION 1 APPROACH 1 STUDY CONTEXT 1 THE CAITHNESS AND SUTHERLAND CONTEXT 1 2 STAYING AND LEAVING 6 SELF-IDENTIFICATION 6 PERCEPTIONS OF STAYERS AND LEAVERS 7 ASPIRATIONS OF SCHOOL LEAVERS 9 FACTORS INFLUENCING DECISIONS AFTER LEAVING SCHOOL 10 3 LEARNING IN CAITHNESS AND SUTHERLAND 12 FURTHER AND HIGHER EDUCATION PROVISION 12 AWARENESS OF UHI AND ITS OFFER 13 INVERNESS CAMPUS 14 GRADUATE PLACEMENTS 15 4 WORKING IN CAITHNESS AND SUTHERLAND 17 EMPLOYMENT-RELATED FACTORS IN THE LOCAL AREA 17 EMPLOYMENT-RELATED FACTORS IN THE H&I 18 IDEAL PLACE TO WORK 20 VIEWS ON H&I GROWTH SECTORS 21 DESIRED QUALITIES IN EMPLOYERS 22 5 LIFE ASPIRATIONS IN CAITHNESS AND SUTHERLAND 24 HOUSING 24 TRANSPORT 25 DIGITAL CONNECTIVITY 27 ARTS, LEISURE AND CULTURE 29 COMMUNITY 30 6 FUTURE ASPIRATIONS OF YOUNG PEOPLE IN CAITHNESS AND SUTHERLAND 32 MAKING CAITHNESS AND SUTHERLAND AN ATTRACTIVE PLACE TO LIVE IN 32 FUTURE ASPIRATIONS 33 HOW THE H&I HAS CHANGED 34 7 CONCLUSIONS 36 KEY SUMMARY FINDINGS 36 CONCLUDING REMARKS 39 A. ANNEX 1: SURVEY RESPONSE PROFILE 40 NUMBER OF RESPONDENTS 40 AGE 40 GENDER 40 GEOGRAPHY 41 STATUS 41 SUMMARY 41 1 Introduction 1.1 This report presents the findings of a wide-ranging study to explore the attitudes and aspirations of young people aged 15-30 in relation to the Highlands and Islands (H&I) of Scotland, with a particular focus on young people in Caithness and Sutherland. -

Offers Over £79,500 Building Plot, Aultbea, IV22
Building Plot, Aultbea, IV22 2JA Building Plot with full planning permission granted, extending to approximately 0.60 acre appreciating a superb open aspect across Loch Ewe and to the surrounding hills Electricity and water on site & drainage to the public sewer Access road and gate in place Offers over £79,500 DESCRIPTION This building plot appreciates an elevated location appreciating a superb aspect across Loch Ewe and to the surrounding hills, Detailed planning permission is in place for a one and a half storey, 4 bedroom property extending to approximately 139sqm with an integrated double garage (04/00250/FULRC), details of which can be provided upon request. The plot is serviced with electricity and water and drainage would be to the public sewer. The plot extends to approximately 0.60 acre with gate and access road in place. Build service available upon request. LOCATION The building plot is situated in of the village of Aultbea, which sits nestled on the north east shore of Loch Ewe on the west coast of the Scottish Highlands. The centre of the village is within walking distance and is a thriving community with a primary school and a pre-school nursery. Secondary school children are transported by daily bus to attend school in Gairloch. In Aultbea there is a general store, church, hotels, a doctors surgery and there is a mobile banking and library service. There are sandy beaches within a short drive of the property and the area is a superb location for outdoor pursuits including fishing, walking, kayaking and climbing. Ideal location for the avid bird watcher. -

Horse Island, Fada and Tanera Ece Estimates 2018
SSF SUMMER ISLES ECE ESTIMATES 2018 SCOTTISH SEA FARMS SSF) SUMMER ISLES: HORSE ISLAND, FADA AND TANERA ECE ESTIMATES 2018 REPORT SUMMER ISLES 002.DOCX For: Scottish Sea Farms Ltd Laurel House Laurel Hill Business Park Stirling FK7 9JQ REPORT 1 SUMMER ISLES 002. DOCX SSF SUMMER ISLES ECE ESTIMATES 2018 SUMMARY This report outlines the hydrography of the area around the Summer Isles, to estimate the effect of existing fish farms at Fada and Tanera, and of a potential fish farm at Horse Island, on local nutrient concentrations via the ' Equilibrium Concentration Enhancement' ( ECE) approach. Tidal and residual flows near the Summer Isles sites have been estimated to be sufficient to dilute the nitrogen released from existing consented sites at Fada and Tanera, and from the potential site at Horse Island, such that the likely ECE of nitrogen in waters local to the sites and in the surrounding waterbodies is less than about 20 µgN.litre-1. The estimated values of ECE compare favourably with various relevant or regulatory standards that relate to: typical background concentrations a previous Environmental Quality Standard for available nitrogen of 168 gN.litre-1 OSPAR & Water Framework Directive Reference Conditions: in offshore waters such as these (salinity above 34), the DIN (Dissolved Inorganic Nitrogen) reference value is 10M and the threshold 15M. Increases are therefore limited to 5 M (70 gN.l-1). In the circumstances examined here, the predicted ECE values are therefore insignificant within the Summer Isles water bodies. REPORT 2 SUMMER ISLES 002. DOCX SSF SUMMER ISLES ECE ESTIMATES 2018 CONTENTS 1 INTRODUCTION .......................................................................................................... -

Atlantic Coast (Wester Ross) Project Tourism And
Atlantic Coast (Wester Ross) Project Topic Paper: Tourism and recreation 1. Introduction This paper is one of a series prepared to help inform the future use and development of the coast and inshore waters of Loch Broom, Little Loch Broom, the Summer Isles and Gruinard Bay. The paper is the result of basic survey and evaluation work and should not be regarded as a policy document. It is however intended to help in the formulation of policy and to promote discussion. The Atlantic Coast project seeks to develop and test an integrated coastal zone plan for this area which can help in the evaluation of development proposals, guide investment, and minimise conflicts of interest. It aims to promote a balanced approach: one that can safeguard the area’s core natural assets and sustain or enhance its productivity over the longer term. This is an area which provides opportunities for a wide range of leisure activities. It has a dramatic and varied coastline, the attractive and lively fishing village of Ullapool, one of Scotland’s most scenic groups of small offshore islands, remote communities, sheltered anchorages, abundant wildlife, fine beaches, archaeological sites, some good wreck diving and a rich underwater environment. It is a popular holiday destination for tourists from the UK and overseas, many of whom are drawn by the beauty of the surroundings and the opportunities provided by the coast, sea and islands. Sailing and kayaking are increasingly popular with both tourists and locals, while cruise boats give visitors an opportunity to explore the islands and to see seals, porpoises and other wildlife at close quarters. -

Interaction Between Bedrock and Quaternary Geology in the Ullapool
Digital surface models and the landscape: Interaction between Bedrock and Glacial geology in the Ullapool area K.M. Goodenough, M. Krabbendam, T. Bradwell, A. Finlayson and A.G.Leslie British Geological Survey, Murchison House, West Mains Road, Edinburgh EH9 3LA Corresponding author: [email protected] Abstract The front cover image for this volume is a hill-shaded digital surface model (DSM) of the Ullapool area, created using NEXTMap Britain elevation data from Intermap Technologies. This is a classic area for bedrock geology, transected by the Moine Thrust Zone, and in recent years has also been studied in detail for its glacial history. Perhaps equally important, this is one of Scotland’s most iconic landscapes. The geology of the area comprises a number of distinct sequences, each of which has a characteristic landscape expression as illustrated by the DSM. This paper considers the influence of the bedrock geology on the glacial geomorphology, and shows that the interplay of the two has led to the development of the different landscape elements of this spectacular area. Introduction This paper is based on the front cover image for this volume, which is a hill-shaded digital surface model (DSM) of the area around Ullapool in the North West Highlands 1 of Scotland (Figure 1). The DSM was created using NEXTMap Britain elevation data from Intermap Technologies, and has been processed to produce a hill-shaded image with apparent illumination from the north-west. The data were obtained by airborne Inferometric Synthetic Aperture radar, flown at a height of 6000 – 9000m. The horizontal resolution is 2-5 m, and the elevation resolution is about 1m. -

Aultbea Caravans Loch Ewe Scottish Highlands
Aultbea Caravans Loch Ewe Scottish Highlands Aultbea Caravans Loch Ewe Scottish Highlands Alexander MacKenzie Daytime Phone: 0*1+445 7031 233 435 Evening Phone: 0*1+445 7031 233 435 Mobile Phone: 0*7+761680517293 4 3*0+ Mell0o1n2 3C4h5a6r7l8e9s A*u+ltbea0 T*h+e Hig0h1l2a3n4d5s6 I*V+22 2J0N1 Scotland £ 260.00 - £ 350.00 per week Two self catering caravans, one six berth and one 5 berth, situated on private crofts overlooking Loch Ewe in Aultbea Ross-shire, North West Scottish Highlands.Both caravans have outside decking. Open all year Round. Pets welcome. Facilities: Room Details: Entertainment: Number of Pitches: 6 TV 2 Hard Standings Kitchen: Cooker, Fridge, Grill, Microwave, Oven, Toaster 1 Toilet Block Laundry: Ironing Board \ Iron, Tumble Dryer, Washing Machine Outside Area: Enclosed Garden, Outside Seating, Patio \ Outside Dining Area, Private Garden, Private Parking Price Included: Electricity and Fuel, Linen Special: Highchairs Available Standard: Very Good Suitable For: Elderly, Families, Romantic getaways, Short Breaks © 2021 LovetoEscape.com - Brochure created: 23 September 2021 Aultbea Caravans Loch Ewe Scottish Highlands About Aultbea and The Highlands Situated in the wild far north west of Scotland the area has many intersting walks, some on your doorstep and some just a short drive away. Fishing is also very popular and available for both sea and fresh water lochs. Beautiful beaches nearby. Nearest Bus Stop: 3 Miles Nearest Train Station: Achnasheen Ross-shire Nearest Airport: Dalcross Inverness 75miles © 2021 LovetoEscape.com - Brochure created: 23 September 2021 Aultbea Caravans Loch Ewe Scottish Highlands Recommended Attractions 1. Gairloch Chandlery Tours and Trips, Boat Trips, Guided Tours and Day Trips Fishing trips, whale watching, trips to see the puffins on the Shiant Gairloch, IV21 2BQ, The Highlands, Islands Scotland 2. -

West Highland and Islands Local Development Plan Plana Leasachaidh Ionadail Na Gàidhealtachd an Iar Agus Nan Eilean
West Highland and Islands Local Development Plan Plana Leasachaidh Ionadail na Gàidhealtachd an Iar agus nan Eilean Adopted Plan September 2019 www.highland.gov.uk How to Find Out More | Mar a Gheibhear Tuilleadh Fiosrachaidh How to Find Out More This document is about future development in the West Highland and Islands area, including a vision and spatial strategy, and identified development sites and priorities for the main settlements. If you cannot access the online version please contact the Development Plans Team via [email protected] or 01349 886608 and we will advise on an alternative method for you to read the Plan. (1) Further information is available via the Council's website . What is the Plan? The West Highland and Islands Local Development Plan (abbreviated to WestPlan) is the third of three new area local development plans that, along with the Highland-wide Local Development Plan (HwLDP) and Supplementary Guidance, forms "the development plan" that guides future development in the Highlands. WestPlan focuses on where development should and should not occur in the West Highland and Islands area over the next 20 years. In preparing this Plan, The Highland Council have held various consultations firstly with a "Call for Sites" followed by a Main Issues Report then an Additional Sites Consultation followed by a Proposed Plan. The comments submitted during these stages have helped us finalise this Plan. This is the Adopted Plan and is now part of the statutory "development plan" for this area. 1 http://highland.gov.uk/whildp Adopted WestPlan The Highland Council 1 How to Find Out More | Mar a Gheibhear Tuilleadh Fiosrachaidh What is its Status? This Plan is an important material consideration in the determination of planning applications. -

Lochbroom During Ww2
LOCHBROOM DURING WW2 Extracts from A Hundred Years in Wester Ross by Donald Shaw, pub. 2002 1939: Britain declared war on Germany on 3rd September. Local territorials were mobilised. The 4th Seaforths, as part of 152 (Highland) Brigade of the 51st Highland Division, were sent to Saarland to guard the Maginot Line. Ullapool Charities Entertainment and Linen League sent Christmas boxes to 94 servicemen in December. Each box contained one iced Christmas cake with regimental badge, a large box of mixed biscuits, a box of sweets, a pair of socks or helmet, a pocket testament, and 50 cigarettes. Non-smokers received (instead of cigarettes) a box of cheese, a packet of dates, a half-pound of chocolate, and a packet of stamped letter-cards. The pocket testament was inscribed with an “encouraging message” from Mrs Fraser, Leckmelm. 1940: Rationing and other restrictions began to affect daily life at home. From January, sugar, bacon and butter were rationed. Meat was not rationed until March, but housewives were still required to register with a nominated butcher in January. The Ross-shire Journal reported that the county had survived the first week of rationing without problems. Supplies had been plentiful. The War Secretary announced that the kilt would no longer be worn by troops, and would be replaced by battledress. For walking out, all ranks in possession of kilts will wear them until they are worn out. There will be no further issue during the war except to pipers and drummers. Severe storms caused damage in February. The wooden pier at the head of Loch Broom, built by German prisoners during the last war, was wrecked, floating down the loch in two pieces, which were caught by locals and used for firewood.