Psychotherapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Cognitive Behavioral Therapy for Perfectionism Over Time (DVD)
Cognitive-Behavioral Therapy for Perfectionism Presented by Martin M. Antony, PhD, ABPP Department of Psychology, Ryerson University Website: www.martinantony.com E-mail: [email protected] Handouts and slides from this presentation may not be reproduced without permission of the presenter April 9, 2015 ©2015 Martin M. Antony, PhD Professor and Chair, Department of Psychology, Ryerson University, Toronto Director of Research, Anxiety Treatment and Research Center, St. Joseph’s Healthcare, Hamilton 1 Anxiety and Depression Association of America Outline Cognitive-Behavioral Therapy for § Overview of perfectionism Perfectionism § Causes of perfectionism § Assessment of perfectionism April 9, 2015 § Introduction to cognitive-behavioral therapy Martin M. Antony, PhD, ABPP § Changing perfectionistic thinking Professor and Chair, Department of Psychology, § Changing perfectionistic behavior Ryerson University, Toronto § Mindfulness and acceptance-based Director of Research, Anxiety Treatment and approaches Research Centre, St. Joseph’s Healthcare, Hamilton § Emerging research on treating perfectionism www.martinantony.com § Recommended books and DVDs Definition of Perfectionism Perfectionism is a disposition to regard anything short of perfection OVERVIEW OF as unacceptable PERFECTIONISM Merriam Webster Dictionary Definition of Clinical Perfectionism Historical Perspectives “The overdependence of self- § “Tyranny of the shoulds” (Horney, 1950) evaluation on the determined pursuit § “Musterbation” (Ellis & Harper, 1961) (and achievement) of self-imposed, § Normal vs. neurotic perfectionism personally demanding standards of (Hamacheck, 1978) performance in at least one salient domain, despite the occurrence of adverse consequences.” Shafran, Cooper, & Fairburn, 2002 2 Examples of Perfectionists Perfectionism in the Context of OCPD § A woman struggles to be a perfect parent, a perfect wife, and a perfect employee, often to the detriment of her own emotional and physical health. -

First Episode Psychosis an Information Guide Revised Edition
First episode psychosis An information guide revised edition Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) i First episode psychosis An information guide Sarah Bromley, OT Reg (Ont) Monica Choi, MD, FRCPC Sabiha Faruqui, MSc (OT) A Pan American Health Organization / World Health Organization Collaborating Centre ii Library and Archives Canada Cataloguing in Publication Bromley, Sarah, 1969-, author First episode psychosis : an information guide : a guide for people with psychosis and their families / Sarah Bromley, OT Reg (Ont), Monica Choi, MD, Sabiha Faruqui, MSc (OT). -- Revised edition. Revised edition of: First episode psychosis / Donna Czuchta, Kathryn Ryan. 1999. Includes bibliographical references. Issued in print and electronic formats. ISBN 978-1-77052-595-5 (PRINT).--ISBN 978-1-77052-596-2 (PDF).-- ISBN 978-1-77052-597-9 (HTML).--ISBN 978-1-77052-598-6 (ePUB).-- ISBN 978-1-77114-224-3 (Kindle) 1. Psychoses--Popular works. I. Choi, Monica Arrina, 1978-, author II. Faruqui, Sabiha, 1983-, author III. Centre for Addiction and Mental Health, issuing body IV. Title. RC512.B76 2015 616.89 C2015-901241-4 C2015-901242-2 Printed in Canada Copyright © 1999, 2007, 2015 Centre for Addiction and Mental Health No part of this work may be reproduced or transmitted in any form or by any means electronic or mechanical, including photocopying and recording, or by any information storage and retrieval system without written permission from the publisher—except for a brief quotation (not to exceed 200 words) in a review or professional work. This publication may be available in other formats. For information about alterna- tive formats or other CAMH publications, or to place an order, please contact Sales and Distribution: Toll-free: 1 800 661-1111 Toronto: 416 595-6059 E-mail: [email protected] Online store: http://store.camh.ca Website: www.camh.ca Disponible en français sous le titre : Le premier épisode psychotique : Guide pour les personnes atteintes de psychose et leur famille This guide was produced by CAMH Publications. -

Resource Document on Social Determinants of Health
APA Resource Document Resource Document on Social Determinants of Health Approved by the Joint Reference Committee, June 2020 "The findings, opinions, and conclusions of this report do not necessarily represent the views of the officers, trustees, or all members of the American Psychiatric Association. Views expressed are those of the authors." —APA Operations Manual. Prepared by Ole Thienhaus, MD, MBA (Chair), Laura Halpin, MD, PhD, Kunmi Sobowale, MD, Robert Trestman, PhD, MD Preamble: The relevance of social and structural factors (see Appendix 1) to health, quality of life, and life expectancy has been amply documented and extends to mental health. Pertinent variables include the following (Compton & Shim, 2015): • Discrimination, racism, and social exclusion • Adverse early life experiences • Poor education • Unemployment, underemployment, and job insecurity • Income inequality • Poverty • Neighborhood deprivation • Food insecurity • Poor housing quality and housing instability • Poor access to mental health care All of these variables impede access to care, which is critical to individual health, and the attainment of social equity. These are essential to the pursuit of happiness, described in this country’s founding document as an “inalienable right.” It is from this that our profession derives its duty to address the social determinants of health. A. Overview: Why Social Determinants of Health (SDOH) Matter in Mental Health Social determinants of health describe “the causes of the causes” of poor health: the conditions in which individuals are “born, grow, live, work, and age” that contribute to the development of both physical and psychiatric pathology over the course of one’s life (Sederer, 2016). The World Health Organization defines mental health as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community” (World Health Organization, 2014). -

An "Authentic Wholeness" Synthesis of Jungian and Existential Analysis
Modern Psychological Studies Volume 5 Number 2 Article 3 1997 An "authentic wholeness" synthesis of Jungian and existential analysis Samuel Minier Wittenberg University Follow this and additional works at: https://scholar.utc.edu/mps Part of the Psychology Commons Recommended Citation Minier, Samuel (1997) "An "authentic wholeness" synthesis of Jungian and existential analysis," Modern Psychological Studies: Vol. 5 : No. 2 , Article 3. Available at: https://scholar.utc.edu/mps/vol5/iss2/3 This articles is brought to you for free and open access by the Journals, Magazines, and Newsletters at UTC Scholar. It has been accepted for inclusion in Modern Psychological Studies by an authorized editor of UTC Scholar. For more information, please contact [email protected]. An "Authentic Wholeness" Synthesis of Jungian and Existential Analysis Samuel Minier Wittenberg University Eclectic approaches to psychotherapy often lack cohesion due to the focus on technique and procedure rather than theory and wholeness of both the person and of the therapy. A synthesis of Jungian and existential therapies overcomes this trend by demonstrating how two theories may be meaningfully integrated The consolidation of the shared ideas among these theories reveals a notion of "authentic wholeness' that may be able to stand on its own as a therapeutic objective. Reviews of both analytical and existential psychology are given. Differences between the two are discussed, and possible reconciliation are offered. After noting common elements in these shared approaches to psychotherapy, a hypothetical therapy based in authentic wholeness is explored. Weaknesses and further possibilities conclude the proposal In the last thirty years, so-called "pop Van Dusen (1962) cautions that the differences among psychology" approaches to psychotherapy have existential theorists are vital to the understanding of effectively demonstrated the dangers of combining existentialism, that "[when] existential philosophy has disparate therapeutic elements. -

Exposure and Cognitive Interventions for Anxiety 1
Exposure and Cognitive Interventions for Anxiety 1 Running head: EXPOSURE AND COGNITIVE INTERVENTIONS FOR ANXIETY Exposure Therapy and Cognitive Interventions for the Anxiety Disorders: Overview and Newer Third Generation Perspectives John P. Forsyth, Velma Barrios, and Dean T. Acheson University at Albany, State University of New York Forsyth, J. P., Barrios, V., & Acheson, D. (2007). Exposure therapy and cognitive interventions for the anxiety disorders: Overview and newer third-generation perspectives. In D. C. S. Richard & D. Lauterbach (Eds.), Handbook of the exposure therapies (pp. 61-108). New York: Academic Press. Exposure and Cognitive Interventions for Anxiety 2 Author Biosketches John P. Forsyth, Ph.D. John P. Forsyth, Ph.D. earned his Ph.D. degree in clinical psychology from West Virginia University in 1997, after serving as Chief Resident in the Department of Psychiatry and Human Behavior at the University of Mississippi Medical Center. He is an Associate Professor and Director of the Anxiety Disorders Research Program in the Department of Psychology at the University at Albany, SUNY. His basic and applied research focuses on variables and processes that contribute to the etiology, maintenance, and treatment of anxiety-related disorders. He has written widely on acceptance and experiential avoidance, and the role of emotion regulatory processes in the etiology and treatment of anxiety disorders. Dr. Forsyth was the recipient of the 2000 B. F. Skinner New Research Award by Division 25 of the American Psychological Association and the 1999 Outstanding Dissertation Award by the Society for a Science of Clinical Psychology. He has authored over 50 scientific journal articles, numerous book chapters, and several teaching supplements for courses in abnormal psychology. -

Theory in the Practice of Psychotherapy
CAE Theory in the Practice of Psychotherapy Muay owe, M.. There are striking discrepancies between theory and practice in psychother- apy. The therapist's theoretical assumptions about the nature and origin of emotional illness serve as a blueprint that guides his thinking and actions during psychotherapy. This has always been so, even though "theory" and " therapeutic method" have not always been clearly defined. Primitive medi- cine men who believed that emotional illness was the result of evil spirits had some kind of theoretical notions about the evil spirits that guided their therapeutic method as they attempted to free the person of the spirits. I believe that theory is important now even though it might be difficult to define the specific connections between theory and practice. I have spent almost three decades on clinical research in psychotherapy. A major part of my effort has gone toward clarifying theory and also toward developing therapeutic approaches consistent with the theory. I did this in the belief it would add to knowledge and provide better structure for research. A secondary gain has been an improvement in the predictability and outcome of therapy as the therapeutic method has come into closer proximity with the theory. Here I shall first present ideas about the lack of clarity between theory and practice in all kinds of psychotherapy; in the second section I will deal specifically with family therapy. In discussing my own Family Systems theory, certain parts will be presented almost as previ- ously published (1,2). Other parts will be modified slightly, and some new concepts will be added. -
Spanish Clinical Language and Resource Guide
SPANISH CLINICAL LANGUAGE AND RESOURCE GUIDE The Spanish Clinical Language and Resource Guide has been created to enhance public access to information about mental health services and other human service resources available to Spanish-speaking residents of Hennepin County and the Twin Cities metro area. While every effort is made to ensure the accuracy of the information, we make no guarantees. The inclusion of an organization or service does not imply an endorsement of the organization or service, nor does exclusion imply disapproval. Under no circumstances shall Washburn Center for Children or its employees be liable for any direct, indirect, incidental, special, punitive, or consequential damages which may result in any way from your use of the information included in the Spanish Clinical Language and Resource Guide. Acknowledgements February 2015 In 2012, Washburn Center for Children, Kente Circle, and Centro collaborated on a grant proposal to obtain funding from the Hennepin County Children’s Mental Health Collaborative to help the agencies improve cultural competence in services to various client populations, including Spanish-speaking families. These funds allowed Washburn Center’s existing Spanish-speaking Provider Group to build connections with over 60 bilingual, culturally responsive mental health providers from numerous Twin Cities mental health agencies and private practices. This expanded group, called the Hennepin County Spanish-speaking Provider Consortium, meets six times a year for population-specific trainings, clinical and language peer consultation, and resource sharing. Under the grant, Washburn Center’s Spanish-speaking Provider Group agreed to compile a clinical language guide, meant to capture and expand on our group’s “¿Cómo se dice…?” conversations. -

Eating Disorders: About More Than Food
Eating Disorders: About More Than Food Has your urge to eat less or more food spiraled out of control? Are you overly concerned about your outward appearance? If so, you may have an eating disorder. National Institute of Mental Health What are eating disorders? Eating disorders are serious medical illnesses marked by severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may be signs of an eating disorder. These disorders can affect a person’s physical and mental health; in some cases, they can be life-threatening. But eating disorders can be treated. Learning more about them can help you spot the warning signs and seek treatment early. Remember: Eating disorders are not a lifestyle choice. They are biologically-influenced medical illnesses. Who is at risk for eating disorders? Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Although eating disorders often appear during the teen years or young adulthood, they may also develop during childhood or later in life (40 years and older). Remember: People with eating disorders may appear healthy, yet be extremely ill. The exact cause of eating disorders is not fully understood, but research suggests a combination of genetic, biological, behavioral, psychological, and social factors can raise a person’s risk. What are the common types of eating disorders? Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. If you or someone you know experiences the symptoms listed below, it could be a sign of an eating disorder—call a health provider right away for help. -
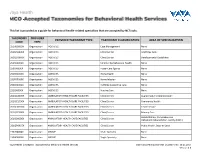
This List Is Provided As a Guide for Behavioral Health-Related Specialties That Are Accepted by Nctracks
This list is provided as a guide for behavioral health-related specialties that are accepted by NCTracks. TAXONOMY PROVIDER PROVIDER TAXONOMY TYPE TAXONOMY CLASSIFICATION AREA OF SPECIALIZATION CODE TYPE 251B00000X Organization AGENCIES Case Management None 261QA0600X Organization AGENCIES Clinic/Center Adult Day Care 261QD1600X Organization AGENCIES Clinic/Center Developmental Disabilities 251S00000X Organization AGENCIES Community/Behavioral Health None 253J00000X Organization AGENCIES Foster Care Agency None 251E00000X Organization AGENCIES Home Health None 251F00000X Organization AGENCIES Home Infusion None 253Z00000X Organization AGENCIES In-Home Supportive Care None 251J00000X Organization AGENCIES Nursing Care None 261QA3000X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Augmentative Communication 261QC1500X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Community Health 261QH0100X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Health Service 261QP2300X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Primary Care Rehabilitation, Comprehensive 261Q00000X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Outpatient Rehabilitation Facility (CORF) 261QP0905X Organization AMBULATORY HEALTH CARE FACILITIES Clinic/Center Public Health, State or Local 193200000X Organization GROUP Multi-Specialty None 193400000X Organization GROUP Single-Specialty None Vaya Health | Accepted Taxonomies for Behavioral Health Services Claims and Reimbursement | Content rev. 10.01.2017 Version -

Cognitive Behaviour Therapy (CBT) and Stroke Rehabilitation
Cognitive Behaviour Therapy (CBT) and Stroke Rehabilitation Amy Quilty OT Reg. (Ont.), Occupational Therapist Cognitive Behavioural Therapy (CBT) Certificate Program, University of Toronto Quinte Health Care: [email protected] Learning Objectives • To understand that CBT: • has common ground with neuroscience • principles are consistent with stroke best practices • treats barriers to stroke recovery • is an opportunity to optimize stroke recovery Question? Why do humans dominate Earth? The power of THOUGHT • Adaptive • Functional behaviours • Health and well-being • Maladaptive • Dysfunctional behaviours • Emotional difficulties Emotional difficulties post-stroke • “PSD is a common sequelae of stroke. The occurrence of PSD has been reported as high as 30–60% of patients who have experienced a stroke within the first year after onset” Canadian Stroke Best Practice Recommendations: Mood, Cognition and Fatigue Following Stroke practice guidelines, update 2015 http://onlinelibrary.wiley.com/doi/10.1111/ijs.12557/full • Australian rates: (Kneeborne, 2015) • Depression ~31% • Anxiety ~18% - 25% • Post Traumatic Stress ~10% - 30% • Emotional difficulties post-stroke have a negative impact on rehabilitation outcomes. Emotional difficulties post-stroke: PSD • Post stroke depression (PSD) is associated with: • Increased utilization of hospital services • Reduced participation in rehabilitation • Maladaptive thoughts • Increased physical impairment • Increased mortality Negative thoughts & depression • Negative thought associated with depression has been linked to greater mortality at 12-24 months post-stroke Nursing Best Practice Guideline from RNAO Stroke Assessment Across the Continuum of Care June : http://rnao.ca/sites/rnao- ca/files/Stroke_with_merged_supplement_sticker_2012.pdf Cognitive Behavioral Therapy (CBT) https://www.youtube.com/watch?v=0ViaCs0k2jM Cognitive Behavioral Therapy - CBT A Framework to Support CBT for Emotional Disorder After Stroke* *Figure 2, Framework for CBT after stroke. -

Eating Disorders
Eating Disorders NDSCS Counseling Services hopes the following information will help you gain a better understanding of eating disorders. If you believe you or someone you know is experiencing related concerns and would like to visit with a counselor, please call NDSCS Counseling Services for an appointment - 701.671.2286. Definition There is a commonly held view that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that cause severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may also signal an eating disorder. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. Signs and Symptoms Anorexia nervosa People with anorexia nervosa may see themselves as overweight, even when they are dangerously underweight. People with anorexia nervosa typically weigh themselves repeatedly, severely restrict the amount of food they eat, and eat very small quantities of only certain foods. Anorexia nervosa has the highest mortality rate of any mental disorder. While many young women and men with this disorder die from complications associated with starvation, others die of suicide. In women, suicide is much more common in those with anorexia than with most other mental disorders. Symptoms include: • Extremely restricted eating • Extreme thinness (emaciation) • A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight • Intense fear of gaining weight • Distorted body image, a self-esteem -

Understanding Mental Health
UNDERSTANDING MENTAL HEALTH WHAT IS MENTAL HEALTH? Our mental health directly influences how we think, feel and act: it also affects our physical health. Work, in fact, is actually one of the best things for protecting our mental health, but it can also adversely affect it. Good mental health and well-being is not an on-off A person’s mental health moves back and forth along this range during experience. We can all have days, weeks or months their lifetime, in response to different stressors and circumstances. At where we feel resilient, strong and optimistic, the green end of the continuum, people are well; showing resilience regardless of events or situations. Often that can and high levels of wellbeing. Moving into the yellow area, people be mixed with or shift to a very different set of may start to have difficulty coping. In the orange area, people have thoughts, feelings and behaviours; or not feeling more difficulty coping and symptoms may increase in severity and resilient and optimistic in just one or two areas of frequency. At the red end of the continuum, people are likely to be our life. For about twenty-five per cent of us, that experiencing severe symptoms and may be at risk of self-harm or may shift to having a significant impact on how suicide. we think, feel and act in many parts of our lives, including relationships, experiences at work, sense of connection to peer groups and our personal sense of worth, physical health and motivation. This could lead to us developing a mental health condition such as anxiety, depression, substance misuse.