Timothy Kwabena Adjei.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Epidemiological Profile of Malaria and Its Control in Ghana
An Epidemiological Profile of Malaria and its Control in Ghana Report prepared by National Malaria Control Programme, Accra, Ghana & University of Health & Allied Sciences, Ho, Ghana & AngloGold Ashanti Malaria Control Program, Obuasi, Ghana & World Health Organization, Country Programme, Accra, Ghana & The INFORM Project Department of Public Health Research Kenya Medical Research Institute - Wellcome Trust Progamme Nairobi, Kenya Version 1.0 November 2013 Acknowledgments The authors are indebted to the following individuals from the MPHD, KEMRI-Oxford programme: Ngiang-Bakwin Kandala, Caroline Kabaria, Viola Otieno, Damaris Kinyoki, Jonesmus Mutua and Stella Kasura; we are also grateful to the help provided by Philomena Efua Nyarko, Abena Asamoabea, Osei-Akoto and Anthony Amuzu of the Ghana Statistical Service for help providing parasitological data on the MICS4 survey; Catherine Linard for assistance on modelling human population settlement; and Muriel Bastien, Marie Sarah Villemin Partow, Reynald Erard and Christian Pethas-Magilad of the WHO archives in Geneva. We acknowledge in particular all those who have generously provided unpublished data, helped locate information or the geo-coordinates of data necessary to complete the analysis of malaria risk across Ghana: Collins Ahorlu, Benjamin Abuaku, Felicia Amo-Sakyi, Frank Amoyaw, Irene Ayi, Fred Binka, David van Bodegom, Michael Cappello, Daniel Chandramohan, Amanua Chinbua, Benjamin Crookston, Ina Danquah, Stephan Ehrhardt, Johnny Gyapong, Maragret Gyapong, Franca Hartgers, Debbie Humphries, Juergen May, Seth Owusu-Agyei, Kwadwo Koram, Margaret Kweku, Frank Mockenhaupt, Philip Ricks, Sylvester Segbaya, Harry Tagbor and Mitchell Weiss. The authors also acknowledge the support and encouragement provided by the RBM Partnership, Shamwill Issah and Alistair Robb of the UK government's Department for International Development (DFID), Claude Emile Rwagacondo of the West African RBM sub- regional network and Thomas Teuscher of RBM, Geneva. -

Download PDF (346.0
Published by Authority No. 52 FRIDAY, 29th DECEMBER 2000 > CONTENTS Page Notice of Publication of Official Bulletin 388 The National Weekly Lotto Results 388 Licence for the Celebration of Marriages—Public Place of Worship (Rtf Evangelical Presbyterian Church of Ghana, Jasikan.) 388 Licence for the Celebration of Marriages—Public Place of Worship (Ref Christ Baptist Church, Suame-Kumasi) 388 ( Licence lor the Celebration of Marriages — Public Place of Worship (Rtf Revival Charismatic Centre, Kumasi) 388 Licence for the Celebration of Marriages-— Public Place of Worship (Ref. Ebenezer Methodist Church, Gomoa Nyanyano 389 Notice of Publication of List of Provisional Registered Veterinary Surgeons .. 389 390 Notice of Change of Names .. .> GHANA GAZETTE- 29m DECEMBER. 2000 38S NOTICE OF PUBLICATION OF OFFICIAL BULLETIN COMMERCIAL AND INDUSTRIAL No. .0 is published today, price: eS.000 Summary of Contents General 212 Notice of Sale of Overtime Goods—Port of Tema NATIONAL WEEKLY LOTTO RESULTS following numbers were drawn in successive order: 53 -40- 15 - 30 - 86 Col. MARTIN GBKPI Director of National Lotteries PUBLIC PLACE OF WORSHIP LICENCE FOR THE CELEBRATION OF MARRIAGES » Under the provision of section 8, subsection (1) of the Marriages Ordinance (Cap. 127) as amended, I, Steve Sclormcy, Director. Office of the Volta Regional Co-ordinating Council, do hereby license the following public place of worship for the celebration of Marriages! Evangelical Presbyterian Church of Ghana, P.O. Box 98 Jasikan. Given under my hand at the office of ihe Volta Regional Co-ordinating Council, this 18th day of October. 2000. STEVE SELORMEY v Director ____________ __ for: Regional Co-ord. -

Geometry and Genesis of the Giant Obuasi Gold Deposit, Ghana
Geometry and genesis of the giant Obuasi gold deposit, Ghana Denis Fougerouse, BSc, MSc This thesis is presented for the degree of Doctor of Philosophy. Centre for Exploration Targeting School of Earth and Environment The University of Western Australia July 2015 Supervisors: Dr Steven Micklethwaite Dr Stanislav Ulrich Dr John M Miller Professor T Campbell McCuaig ii "It never gets easier, you just go faster" Gregory James LeMond iv Abstract Abstract The supergiant Obuasi gold deposit is the largest deposit hosted in the Paleoproterozoic Birimian terranes of West Africa (62 Moz, cumulative past production and resources). The deposit is hosted in Kumasi Group sedimentary rocks composed of carbonaceous phyllites, slates, psammites, and volcaniclastic rocks intruded by different generations of felsic dykes and granites. In this study, the deformation history of the Obuasi district was re-evaluated and a three stage sequence defined based on observations from the regional to microscopic scale. The D1Ob stage is weakly recorded in the sedimentary rocks as a layer-parallel fabric. The D2Ob event is the main deformation stage and corresponds to a NW-SE shortening, involving tight to isoclinal folding, a pervasive subvertical S2Ob cleavage striking NE, as well as intense sub-horizontal stretching. Finally, a N-S shortening event (D3Ob) formed an ENE-striking, variably dipping S3Ob crenulation cleavage. Three ore bodies characteristic of the three main parallel mineralised trends were studied in details: the Anyankyerem in the Binsere trend; the Sibi deposit in the Gyabunsu trend, and the Obuasi deposit in the main trend. In the Obuasi deposit, two distinct styles of gold mineralisation occur; (1) gold-bearing sulphides, dominantly arsenopyrite, disseminated in metasedimentary rocks and (2) native gold hosted in quartz veins up to 25 m wide. -

Download PDF (891.2
GHANA gazette pi REPUBLIC OF GHANA of Published by Authority No. 81 2012 CONTENTS Page Notice of Publication of an Official Bulletin 2176 2176 Licence for the Celebration of Marriages—Public Place of Worship (Ref. Church of Pentecost, Akaporiso Assembly, Obuasi) 2176 Licence for the Celebration of Marriages—Public Place of Worship (Ref God’s Church of Peace) .. 2176 Licence for the Celebration of Marriages—Public Place of Worship (Ref Anointed Revival Ministry Tantra HrH, Accra) 2177 Appointment of Marriage Officers (House of Faith Ministries, Obuasi) 2177 Appointment of Marriage Officers (Born Again Believers’ Ministry, Obuasi, Ghana) 2177 Appointment of a Marriage Officer (Restoration Community Chapel of Come Back Ministries, Accra) 2177 2178 I Gazetting of Returns on Assets and Liabilities of Bank of Ghana as at 15th October, 2012 I 2179 Change of Names 2185 Change of Dates of Birth 2186 Change of Name of a Church 1 V \ I NOVEMBER ?on APPOINTMENT OF MARRIAGE 2177 -Under the provisions of section 38 of the Marriages Act, 1884 OFFICERS Instrument, 1971 (L.I. 707), the following Minist - 1985 (Cap. 127) and the Ministers Functions for House of Faith Ministries, Obuasi. crs °f Religion are hereby appointed as Marriage Officers 1 Reverend Samuel Kwamc Antwi 2. Reverend Emmanuel Asantc 14. Reverend Kennedy Amponsah Ayim 3. Reverend Michael Jackson Nkansah 15. Reverend Daniel Appiah Aboroso 4. Reverend Alexander Ohcne Amoah 16. Reverend Baffour Asare-Bediako 5. Reverend Isaac Agycn 17. Reverend Augustine Addai 6. Reverend Jonathan Kudjordji 18. Reverend Michael Frimpong 7. Reverend Lawrence Larry-Lawal 19. Reverend Samuel Osei Kwarteng S. -
University of G Institute of African Studies 3U C B
UNIVERSITY OF G INSTITUTE OF AFRICAN STUDIES 18 JUN1969 DEVEL0PMEN1 MUDIES "W 91/ 3 ) W O Jt. LIBRARY 3UCBAJ IS TER 1966 UNIVERSITY OF GHANA INSTITUTE OF AFRICAN STUDIES RESEARCH REVIEW VOL. 3 NO.1 MICHAELMAS TERM 1966 RESEARCH REVIEW CONTENTS INSTITUTE NEWS Staff......................... • • • p. 1 LONG ARTICLE African Studies in Germany, Past and Present.................... p. 2 PRO JECT REPORTS The Ashanti Research Project................ P*|9 Arabic Manuscripts........... ............. .................................. p .19 INDIVIDUAL RESEARCH REPORTS A Study in Urbanization - Progress report on Obuasi Project.................................................................... p.42 A Profile on Music and movement in the Volta Region Part I . ............................................. ........................ p.48 Choreography and the African Dance. ........................ p .53 LIBRARY AND MUSEUM REPORTS Seminar Papers by M .A . Students. .................. p .60 Draft Papers................................................... ........ p .60 Books donated to the Institute of African Studies............. p .61 Pottery..................................................................... p. 63 NOTES A note on a Royal Genealogy............................... .......... p .71 A note on Ancestor Cult in Ghana ................. p .74 Birth rites of the Akans ..................................... p.78 The Gomoa Otsew Trumpet Set........... ............. ............. p.82 ******** THE REVIEW The regular inflow of letters from readers -

Ghana Gazette
GHANA GAZETTE REPUBLIC OF GHANA Published by Authority No. 108 FRIDAY, 28TII NOVEMBER 2014 CONTENTS Page Notice of Publication of a Bill 2040 Licence for the Celebration of Marriages—Public Place of Worship (Lighthouse Chapel International Bread of Life Cathedral, Adenta) 2040 Licence for the Celebration of Marriages—Public Place of Worship (Presbyterian Church of Ghana Resurrection Congregation, New Dormaa/Low Cost, Sunyani) 2040 Licence for the Celebration of Marriages—Public Place of Worship ('Faith Temple Church International IIo) 2040 Licence for the Celebration of Marriages—Public Place of Worship (Presbyterian Church of Ghana 2041 New-Life Congregation, Bomaa) Licence for the Celebration of Marriages—Public Place of Worship (Evangelical Presbyterian Church 2041 ICpcvc Newtown) Marriage Officer (United Bible Church International, Taifa, Accra) 2041 Appointment of a 5 rriage Officer (Calvary Charismatic Baptist Church, Cape Coast) 2041 Appointment of a Ma nd Liabilities of Bank of Ghana as at 14th November, 2014 2042 Gazetting of Returns on Assets a 2043 Change of Names 2049 Change of Dates of Birth ••OIBCFmiRV i FACULTY OF LAW UNIVERSITY OF GHANA I EGON — lsirwJ«w*w;ras;ir>ri' SKruOT jrsrcwaOTVtf.rj. r.HANA GAZETTE, 28th NOVEMBER, 2014 2040 NOTICE OF PUBLICATION OF A BILL The following Bill is published today: The Chartered Institute of Taxation Bill, 2014 PUBLIC PLACE OF WORSHIP LICENCE FOR THE CELEBRATION OF MARRIAGES Under the provisions of section 8, subsection (1) of the Marriage Ordinance (Cap. 127) as amended, I, E. K. Nyagbe, Regional Co-ordinating Director, Office of the Greater Accra Regional Co-ordinating Council, do hereby license the following public place of worship for the celebration of Marriages. -

Church Directory for Ghana
Abilene Christian University Digital Commons @ ACU Stone-Campbell Books Stone-Campbell Resources 10-1-1980 Church Directory for Ghana World Bible School Follow this and additional works at: https://digitalcommons.acu.edu/crs_books Part of the Africana Studies Commons, Biblical Studies Commons, Christian Denominations and Sects Commons, and the Christianity Commons Recommended Citation World Bible School, "Church Directory for Ghana" (1980). Stone-Campbell Books. 591. https://digitalcommons.acu.edu/crs_books/591 This Book is brought to you for free and open access by the Stone-Campbell Resources at Digital Commons @ ACU. It has been accepted for inclusion in Stone-Campbell Books by an authorized administrator of Digital Commons @ ACU. ~••,o CHURCH Dt:ECTORY for GHANA Give Africans The Gospel .. They'll Do Th~ Preaching! "'rT,,Tl"\T,T'T T"'T"\r"IT"'lfT"'ltT~r r\.l...,l\.1\U liLL.LJ\.JLi'iLH .l .J We are endebted to Bro. John Kesse and Bro. Samuel Obeng of Kumasi, Ghana, and to Bro. Ed Mosby our American missionary in Accra, Ghana for coordinating the information in this directory. It is suggested that all W.B.S. teachers notify their students of the information concerning the church nearest them, so they can go to the brethren for further instruc tion and baptism. It is not logical to expect the local preachers to contact the thousands of students, but the people can go to the brethren all over Ghana. The preachers in Ghana who were contacted were in accord with this plan and will give full cooperation. TIMES OF SERVICES: Most congregations in Ghana meet at 9:00 a.m. -
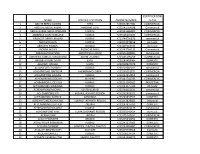
Name Specific Location Phone Number Certification Class
CERTIFICATION NAME SPECIFIC LOCATION PHONE NUMBER CLASS 1 ABAYIE BERKO AKWASI TEPA +233542854981 COMMERCIAL 2 ABDULAI ABDUL-RAZAK MABANG TEPA +233242764598 Commercial 3 ABDUL-KARIM ABDUL RAHMAN KUMASI +233243286809 COMMERCIAL 4 ABEBRESE DJAN ROWLAND KUMASI +233506264844 COMMERCIAL 5 ABOAGYE DANIEL AKWASI KUMASI +233244756870 commercial 6 ABOAGYE ELVIS KUMASI +233242978816 domestic 7 ABOAGYE KWAME BEKWAI +233207163334 domestic 8 ABORAH MOSES BUOHO KUMASI +233247764133 Commercial 9 ABRAHAM BOATENG AKROPONG KUMASI +233246188985 commercial 10 ABROKWA SAMUEL KORANTENG ADUM , KUMASI +233246590209 COMMERCIAL 11 ABUGRI AYAGRI DAVID EJISU +233249458064 DOMESTIC 12 ABUKARI INUSAH EJURA +233200937079 DOMESTIC 13 ACCOMFORD RICHARD KUMASI +233201682011 commercial 14 ACHEAMPONG BAFFOUR AHENEMAKOKOBEN +233248253831 COMMERCIAL 15 ACHEAMPONG AKWASI KUMASI +233242954852 commercial 16 ACHEAMPONG GIDEON MAAKRO +233241744743 COMMERCIAL 17 ACHEAMPONG JOE ELLIS KUMASI +233244560405 INDUSTRIAL 18 ACHEAMPONG KWABENA KUMASI +233243375366 domestic 19 ACHEAMPONG MICHAEL ASAFO-KUMASI +233244102431 commercial 20 ACHEAMPONG NTI KUMASI, ASHANTI REGION +233262428325 commercial 21 ACHEAMPONG PATRICK KONONGO +233249833553 DOMESTIC 22 ACHEAMPONG RICHMOND KUMASI ASHANTI REGION +233243828683 Industrial 23 ACHEAMPONG STEPHEN OBUASI +233247937033 DOMESTIC 24 ACHEAMPONG WILLIAM KUMASI +233203321176 commercial 25 ACHEAMPONG YAW KUMASI,ASHANTI REGION +233265042424 domestic 26 ACKAH JOHN OBUASI +233275247651 COMMERCIAL 27 ACKAH PADMORE BEKWAI +233245340252 DOMESTIC 28 ACKAH PHILIP -

Northern Volta Ashanti Brong Ahafo Western Eastern Upper West
GWCL/AVRL Systems, Service Areas and Towns and Cities Served *# (!BAWKU BAWKU *# Legend Legend (! Upper East Water use in GWCL/AVRL Service Areas (AVRL 2007) NAVRONGO *#!(*# GWCL/AVRL system (AVRL 2007) NAVRONGO Upp(!er East Design plant capacity BOLGATANGA *# < 2000 m^3/day *# 2000 - 5000 m^3/day water use, tanker 5000 - 10000 m^3/day *# water use, domestic connection Upper West water use, commercial connections Upper West *# 10000 - 50000 m^3/day water use, industrial connections water use, industrial connections > 50000 m^3/day *# water use, sachet producers *# water use, unmetered standpipes Served town / city (!WA WA water use, metered standpipes Population (GSS 2000) Main road !( 1000 - 5000 Water body (! 5001 - 15,000 Region *# (! 15,001 - 30,000 !*# (! 30,001 - 50,000 (YENDI Northern YENDI TAMALE Norther(!nTAMALE (!50,001 - 100,000 (!*# DAMONGO (!> 100,000 Link between system and served town Main road Water body Region Brong Ahafo Brong Ahafo *# *# *# *# (!TECHIMAN (! TECHIMAN WORAWORA ! (!*# (BEREKUM *# JASIKAN BEREKUM (!SUNYANI Volta SUNYANI Volta !(*# *# DWOMMO !(*# *# NKONYA AHENKRO! HOHOE (HOHOE (! DWOMMO BIASO *# *# BIASO *# (! M(!AMPONG *# !( TEPA # (!*# MAMPONG ACHERENSUA * !( KPANDU (! SO*#VIE KPANDU AGONA !( TEPA (!*# ANFOEGA DZANA (!*# ACHERENSUA *# (!ASOKORE KPEDZE As*#hanti *# Ashanti *# KUMASI (!KUMASI (! KONONGO *# *# *# *# (! (!HO KONONGO HO ! !( TSITO Eastern N(KAWKAW ANUM NKAWKAW *# *# E(!a*#stern ANYINAM !( (! (! OSINOBEGORO *# KWABENG *#!( *# (! BUNSO *# (! ASUOM JUAPONG *# *#*# (! NEW TAFO # !( # NEW TAFO * -

DREF Operation N° MDRGH008 GLIDE N° EP-2013-000009-GHA 1 February, 2013
Disaster relief emergency fund (DREF) Ghana: Cholera Epidemic DREF operation n° MDRGH008 GLIDE n° EP-2013-000009-GHA 1 February, 2013 The International Federation of Red Cross and Red Crescent (IFRC) Disaster Relief Emergency Fund (DREF) is a source of un-earmarked money created by the Federation in 1985 to ensure that immediate financial support is available for Red Cross and Red Crescent emergency response. The DREF is a vital part of the International Federation’s disaster response system and increases the ability of National Societies to respond to disasters. CHF 205,309 has been allocated from the IFRC’s Disaster Relief Emergency Fund (DREF) to support Ghana Red Cross National Society (GRCS) in delivering immediate assistance to some 12,000 households. Unearmarked funds to repay DREF are encouraged. Summary: Ghana’s health authorities officially declared a cholera outbreak in the Ashanti region on 8th of January 2013. As of 21 January, 18 persons had died and over 250 persons are currently being cared for at the hospitals. Currently, 310 cases have been registered. The affected areas include the Obuasi Municipality District and Ejura/Sekyedumase District both in the Ashanti Region. These districts Hygiene awareness raising done by GRCS volunteers started reporting pockets of cholera cases in Photo: GRCS December 2012. With this DREF operation, GRCS intends to reduce the risks for spread of the cholera infection and assist infected persons through cholera prevention awareness activities targeting 12,000 households in the affected districts, and early detection of cases and referral services. Additionally, water, sanitation and hygiene promotion activities will be implemented in the affected communities in order to reduce risks for water borne diseases with focus on cholera. -
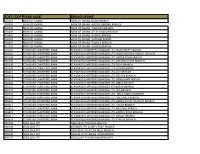
Sort Code Bank Name Branch Name
SORT CODE BANK NAME BRANCH NAME 010101 BANK OF GHANA BANK OF GHANA ACCRA BRANCH 010303 BANK OF GHANA BANK OF GHANA -AGONA SWEDRU BRANCH 010401 BANK OF GHANA BANK OF GHANA -TAKORADI BRANCH 010402 BANK OF GHANA BANK OF GHANA -SEFWI BOAKO BRANCH 010601 BANK OF GHANA BANK OF GHANA -KUMASI BRANCH 010701 BANK OF GHANA BANK OF GHANA -SUNYANI BRANCH 010801 BANK OF GHANA BANK OF GHANA -TAMALE BRANCH 011101 BANK OF GHANA BANK OF GHANA - HOHOE BRANCH 020101 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-HIGH STREET BRANCH 020102 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD- INDEPENDENCE AVENUE BRANCH 020104 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-LIBERIA ROAD BRANCH 020105 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-OPEIBEA HOUSE BRANCH 020106 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-TEMA BRANCH 020108 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-LEGON BRANCH 020112 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-OSU BRANCH 020118 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-SPINTEX BRANCH 020121 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-DANSOMAN BRANCH 020126 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD-ABEKA BRANCH 020127 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH)-ACHIMOTA BRANCH 020129 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD- NIA BRANCH 020132 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD- TEMA HABOUR BRANCH 020133 STANDARD CHARTERED BANK STANDARD CHARTERED BANK(GH) LTD- WESTHILLS BRANCH 020436 -

Support for the Implementation Of
TECHNICAL COOPERATION PROJECT SUMMARY PROJECT TITLE SUPPORT FOR THE IMPLEMENTATION OF TIMEBOUND MEASURES FOR THE ELIMINATION OF THE WORST FORMS OF CHILD LABOR IN GHANA REGION/COUNTRY AFRICA/Ghana PROJECT DURATION September 30, 2004 –June 30, 2009 FISCAL YEAR & FUNDING LEVEL FY 2004: USD 4,750,000 PROBLEM TO BE ADDRESSED Approximately 40 percent of 5 to17 year olds are economically active in Ghana, a large number of whom are engaged in the worst forms of child labor including child domestic work, fishing, head portering (kayaye), commercial sexual exploitation, customary or ritual servitude, mining and quarrying, and commercial agriculture. TARGETS The project targets a total of 10,000 children for withdrawal and prevention from exploitive work through the provision of educational services. The project targets 4,700 children for withdrawal and 5,300 children for prevention, and targets the following sectors: agriculture, fishing, commercial sexual exploitation, domestic work, ritual servitude, head portering (kayaye), and the informal sector. In addition, 3,500 families of targeted children will be provided with assistance for economic empowerment. PROJECT OBJECTIVES To contribute to the elimination of the worst forms of child labor and the creation of strong institutional and socio-economic bases for dealing effectively with all exploitive child labor in Ghana. Immediate objectives include: The Government of Ghana, social partners, community organizations, and NGOs will have the mandate and capacity to undertake effective action against