Adams Safety Training
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Production of Flavored Milk Drinks
Solutions for Your TOUGHEST MIXING Applications in FOOD Production of Flavored Milk Drinks THE FIRST NAME IN HIGH SHEAR MIXERS Production of Flavored Milk Drinks Flavored milk drinks are available in many varieties. Viscosities range from that of whole milk, to “thick milkshake” products which achieve their viscosity through use of thickening additives, sometimes in combination with freezing. Yogurt drinks are similar in composition, but are processed differently and are not covered in this report. Milk ingredients are also used in smoothies to add texture and interest. Find out more about the Manufacture of Smoothies. In most countries, legislation covers the composition and labelling of these products. These regulations restrict the use of certain ingredients and specify minimum content of fat and total solids. Ingredient Typical % Function 0 - 3.5 Fat adds body and mouthfeel. Lower fat contents are more refreshing and suited Milk Fat 1% is to fruit flavors. Chocolate works better in higher fat formulations. typical A blend of milks is used to give a particular fat content. Sugar Various sugars, syrups and artificial sweetener blends is used. 4 - 6 Chocolate milks are usually formulated with higher sugar/sweetener content. Many different flavors are possible, the most common being banana, Flavor 0.1 strawberry and chocolate. The use of flavorings is controlled by legislation in many countries. Both natural and synthetic flavors are used. Color Liquid colors are added to strawberry milks. Choice of color is determined by 0.1 processing conditions, and may be affected by legislation. Stabilizers enhance body and viscosity as required. A blend of products is used Stabilizer 0.1 - 0.3 to obtain a range of properties. -
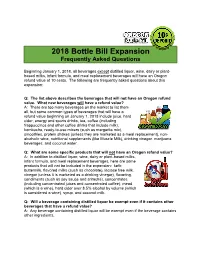
2018 Bottle Bill Expansion: Frequently Asked Questions
2018 Bottle Bill Expansion Frequently Asked Questions Beginning January 1, 2018, all beverages except distilled liquor, wine, dairy or plant- based milks, infant formula, and meal replacement beverages will have an Oregon refund value of 10 cents. The following are frequently asked questions about this expansion: Q: The list above describes the beverages that will not have an Oregon refund value. What new beverages will have a refund value? A: There are too many beverages on the market to list them all, but some common types of beverages that will have a refund value beginning on January 1, 2018 include juice, hard cider, energy and sports drinks, tea, coffee (including frappuccinos and other coffee drinks that include milk), kombucha, ready-to-use mixers (such as margarita mix), smoothies, protein shakes (unless they are marketed as a meal replacement), non- alcoholic wine, nutritional supplements (like Muscle Milk), drinking vinegar, marijuana beverages, and coconut water. Q: What are some specific products that will not have an Oregon refund value? A: In addition to distilled liquor, wine, dairy or plant-based milks, infant formula, and meal replacement beverages, here are some products that will not be included in the expansion: kefir, buttermilk, flavored milks (such as chocolate), lactose free milk, vinegar (unless it is marketed as a drinking vinegar), flavoring, condiments (such as soy sauce and sriracha), concentrates (including concentrated juices and concentrated coffee), mead (which is a wine), hard cider over 8.5% alcohol by volume (which is considered a wine), syrup, and coconut milk. Q: Will a beverage containing distilled liquor be exempt even if it contains other beverages that have a refund value? A: Any beverage containing distilled liquor will be exempt even if the beverage contains other ingredients. -

DF0421 Rutters Profile
Pictured (from left to right) is Rutter’s senior management team: Diane Quinn, PROCESSOR PROFILE customer service manager; Rick RUTTER’S DAIRY Miller, sales/marketing director, Todd Rutter, president; Brett Garner, director of operations; and Smoke Dehoff, director of transportation. A century of local milk Rutter’s Dairy values long-term ties to its community and to the local farmers from which it sources its milk. By Anna Boisseau, managing editor Executive photo by Vito Palmisano Dairy Foods | April 2021 | www.dairyfoods.com PROCESSOR PROFILE RUTTER’S DAIRY ork, Pa., can trace its beginnings back to 1741, when settlers from the YPhiladelphia region founded the city. And Rutter’s Dairy — which is based in this area — has an origin story that goes back almost as far. In 1747, Andrew Rutter was deeded 167 acres in York County, Pa., by Springetts Penn (the great- grandson of William Penn), the company says. This began the Rutter family’s farm operations. But it wasn’t until 1921, when George and Bud Rutter began Rutter’s dairy retail trucks have evolved from their beginning delivering milk to selling milk from said farm, that customers’ homes. Rutter’s Dairy was officially formed. Then known as “Crystal Spring An array of beverages “Central Pennsylvania is the peanut Dairy,” Rutter’s got its start as Rutter’s produces 103 SKUs in the fluid butter capital of the world. Peanut a home delivery business, says milk, tea and juice categories, says butter here is like bacon is to the rest Todd Rutter, president and third- Rick Miller, sales/marketing director. -

Actually Rejected. a Considerable Amount of Off-Flavored Milk and Cream Is Accepted Which Can Not Be Made Into High-Grade Dairy- Products
264 YEARBOOK OF AGRICULTURE, 1927 actually rejected. A considerable amount of off-flavored milk and cream is accepted which can not be made into high-grade dairy- products. The resulting manufactured products must be sold at relatively low prices, and the returns to dairy farmers are correspond- ingly low. No industry, even a prosperous one, can afford to shoulder such a load. If such losses occurred in any other of the giant trade channels of this country, instant steps would be taken to find and correct the trouble. Efficiency experts, factory-management studies, research laboratories, engineers—all would be used to solve the problem. Progress in Dairy Sanitation Is this '^old man of the sea'^ saddled forever upon the dairy indus- try? By no means. His grip is loosening rapidly and he may be shaken off by concerted effort. Two things point to his ultimate elimination. One is the progress already made in dairy sanitation; the other is the fact that the solution of the problem is already pretty well worked out. Great strides have been made in overcom- ing this waste. It was not so many years ago that sour milk on the breakfast table was a fairly common occurrence. Now one can travel almost anywhere and be assured of purchasing sweet, palat- able milk. All this has come about in spite of the fact that the milk supply of this country is much more complex than it used to be. Milk is now transported hundreds of miles to the cit}'^, whereas it used to come from closely adjacent territory. -

Flavored-Milk.Pdf
Dairy Council November | December 2008 Volume 79 ® Number 6 SUMMARY A review of the scientific literature indicates that flavored milk such as chocolate milk Flavored milk is white cow’s milk consumed in moderation does not cause (whole, low-fat, fat-free) with added overweight/obesity, tooth decay, or flavoring (chocolate, strawberry, etc.) hyperactivity and other behavioral disorders and sweetener(s). This highly preferred, in children. Also, chocolate milk contains a nutrient-rich beverage is just as nutritious negligible amount of caffeine and the little as unflavored (white) milk. Both flavored amount of oxalic acid in chocolate milk does and white milk provide several nutrients not impair calcium absorption. Emerging (i.e., calcium, potassium, and magnesium) research indicates that chocolate milk that are low in children’s and adults’ diets. may help adults recover from strenuous, energy-depleting resistance exercise. Currently, more than half of children ages 2 to 8 and three-quarters of adolescents Several health professional organizations fail to consume recommended servings of including the American Academy of low-fat or fat-free milk or milk products. Pediatrics and the American Academy of Therefore, it is important not to limit Pediatric Dentistry support consumption children’s and adolescents’ access to of flavored milk, a nutrient-rich beverage, in flavored milk due to its sugar content. moderation. The 2005 Dietary Guidelines FLAVORED Doing so may have the undesirable effect for Americans state that small amounts MILK: of further reducing intakes of many of sugars added to nutrient-dense foods, essential nutrients provided by milk. such as reduced-fat milk, may increase QUESTIONS & consumption by enhancing palatability, Children’s consumption of flavored milk thus improving nutrient intake without ANSWERS has been shown to increase their total contributing excessive calories. -

Chapter 1530 Department of Agriculture Milk, Milk Products, and Standards
MINNESOTA RULES 2001 250 CHAPTER 1530 DEPARTMENT OF AGRICULTURE MILK, MILK PRODUCTS, AND STANDARDS MILK AND CREAM AND RELATED PRODUCTS 1530.0550 PASTEURIZATION OF CREAMING MIXTURE. 1530.0010 DEFINITIONS. 1530.0560 DIACETYL STARTER DISTILLATE OR 1530.0020 MILK. OTHER FLAVORING SUBSTANCES. 1530.0030 GOAT MILK. 1530.0570 DEFINITIONS. 1530.0040 EWE MILK. 1530.0580 LABEL STATEMENTS. 1530.0050 CREAM. 1530.0590 LABEL STATEMENT REGARDING 1530.0060 HOMOGENIZED CREAM. ARTIFICIAL FLAVORING. 1530.0070 SOUR CREAM, CULTURED SOUR CREAM. 1530.0600 LABEL DECLARATIONS TO BE USED IN 1530.0080 LIGHT CREAM, COFFEE CREAM. OR TABLE CONJUNCTION WITH "CREAMED COTTAGE CREAM. CHEESE." 1530.0090 WHIPPED LIGHT CREAM, COFFEE CREAM. 1530.0610 VITAMIN D MILK AND MILK PRODUCTS. OR TABLE CREAM. 1530.0620 FORTIFIED MILK PRODUCTS. 1530.0100 WHIPPING CREAM. 1530.0630 RECONSTITUTED OR RECOMBINED MILK 1530.0110 LIGHT WHIPPING CREAM. AND MILK PRODUCTS. 1530.0120 HEAVY CREAM OR HEAVY WHIPPING 1530.0640 STERILIZED MILK. CREAM. 1530.0650 HOMOGENIZED MILK AND HOMOGENIZED 1530.0130 WHIPPED CREAM. 1530.0140 HALF AND HALF. MILK PRODUCTS. 1530.0150 SOUR HALF AiND HALF OR CULTURED 1530.0660 WHEY. 1530.0670 CONCENTRATED MILK TO BE HALF AND HALF. 1530.0160 DRY MILK, DRY MILK SOLIDS. RECONSTITUTED FOR FLUID USE. 1530.0680 CONCENTRATED MILK PRODUCTS. 1530.0170 NONFAT DRY MILK. 1530.0690 ACIDIFIED MILK AND MILK PRODUCTS. 1530.0180 INSTANT NONFAT DRY MILK. 1530.0700 MILK PRODUCTS. 1530.0190 CONDENSED SKIM MILK, EVAPORATED 1530.0710 OPTIONAL INGREDIENTS. SKJM MILK, CONCENTRATED SKIM MILK. 1530.0200 SWEETENED CONDENSED SKIM MILK. GRADE A REQUIREMENTS FOR MILK, MILK 1530.0210 DRY BUTTERMILK. PRODUCrS, AND GOAT MILK 1530.0220 DRY WHEY. -

Journal of Milk Technology
'-/· .> Ί ' JOURNAL OF MILK TECHNOLOGY Volu 14 Number 2 MARCH-APRIL, 1941 Official Publication of International Association of Milk Sanitarians (Association Organized 1911) Alto designated publication of California Association of Dairy and Milk Inspectors Central States Milk Sanitarians Chicago Dairy Technology Society Connecticut Association of Dairy and Milk Inspectors Indianapolis Dairy Technology Club Massachusetts Milk Inspectors’ Association Metropolitan Dairy Technology Society Michigan Association of Dairy and Milk Inspectors Missouri Association of Milk Sanitarians New York State Association of Dairy and Milk Inspectors Pacific Northwest Association of Dairy and Milk Inspectors Pennsylvania Association of Dairy Sanitarians Philadelphia Dairy Technology Society Texas Association of Milk Sanitarians West Virginia Association of Milk Sanitarians II A dvertisements PERHAPS as a boy you took many a drink from it without a thought about how insanitary it might be. N ot so today. The patient work of sanitation and pub YOUR DAIRY CUSTOMERS can actually lic health officers has taught you to say see the safe protection of the Welded “nix” to the public drinking cup. And Wire Hood —and seeing is believing. their science, too, has solved many They recognize that you are safeguard problems of dairy sanitation—including ing their health when they see how you how to protect the pouring lip of your protect that pouring lip from contami sterilized milk and cream bottles. nation. Vet, even though the Hood is locked on with welded wire, it comes off HEALTH OFFICERS themselves say that quickly, without effort. they prefer the complete protection of the Welded Wire Hood Seal. It covers FREE INFORMATION-W rite for details the entire pouring lip and top against on Hood Capping and our interesting insanitary dust and filth. -

MAPPINGMAPPING –– BENCHMARKINGBENCHMARKING Dairy & Beverage Market Opportunity Versi
MAPPINGMAPPING –– BENCHMARKINGBENCHMARKING Dairy & Beverage Market Opportunity versi TETRAPAK KeyKey TrendsTrends Urbanization Cost 50% population Consciousness will live in big Affordability and cities convenience Health Fragmented Looking for value Distribution of quality and Available and freshness accessible at both traditional and modern outlets IndonesiaIndonesia A & B AND C & D 210 Million C, D & E Consumers 15 Million A & B Consumers Consumers Modern AND Traditional 3,000 Outlets Trade 2,000,000 Outlets Premium, Value AND Emerging Portfolio IndonesiaIndonesia PackagedPackaged ReadyReady ToTo DrinkDrink 20032003 Beer Soya Sport & Energy 3% 0% 2% Consumption in million liter RTD Tea (exclude powder, concentrate, 13% syrup and bulk) Water 3,585.7 Liquid Dairy Product 215.1 JNSD 108.3 CSD 9% CSD 507.3 RTD Tea 672.3 Sport & Energy 109.2 Beer 146.8 JNSD Soya 10.3 2% LDP 4% Total 2003 5,355.0 Water 67% Source : Tetra Compass 2004 GrowthGrowth PlatformsPlatforms Safety HEALTH • Basic quality • Functional benefits Health GROWTH • Nutritional benefits Nutrition PLATFORM • Branding • Availability Urbanization ON-THE-GO • Ambient products GROWTH • Traditional trade Mobility PLATFORM • Infrastructure • Branding • Attractiveness Big and Young KIDS GROWTH • Impulse purchase Population • Fun elements PLATFORM • Branding PlayersPlayers inin RTDRTD teatea categorycategory “Which are the top global players for RTD tea today?” 1. Unilever Group 10.4 % 2. Kirin Brewery Co 7.8 % 3. Nestlé SA 7.6 % 4. Suntory Ltd 6.7 % 5. Ito En Ltd 5.4 % 6. Asahi Breweries -
Flavored Milk Infographic
Taste good, feel good: the rise of flavored milk As parents and schools have learned, kids are more likely to drink their milk when it’s flavored. That’s sparked some debate about balancing nutritional value and added sugars. of milk consumed #1 source of in American schools 9 essential nutrients 71% 2 is flavored1 in many kids’ diets Flavors find favor New approaches to dairy While the fluid milk category Today’s dairy is finding new fans among adults and label- is down overall, 2010-17 conscious consumers. consumption shows:3 Fewer gallons, more single-serving sizes3 boosts label-friendly appeal 9.2% Health halo increase in chocolate milk Protein power: convenient and inexpensive 2 Less low-fat, more full-fat for satiety 4.8% increase in other flavored milks Innovation, nutrition key to momentum Innovative flavors, Fortified milks Reduced sugar Convenient including fruit, with added calcium, formulations packaging, dessert, seasonal protein, Omega-3’s balance taste single-serve bottles, and coffee flavors and other nutrients and wellness cartons, pouches and flavor concentrates SPORTS FAN: Research indicates that protein and carbohydrates in flavored milk make it an effective workout recovery drink4 All the taste, Cargill Reduced-Sugar Chocolate Milk zero added Featuring ViaTech® Stevia Sweetener sugar 0 added sugars calorie reduction Super-duper 5 25% good!” 2.5g fat per 8 oz. serving 1 Severson, Kim. “A School Fight Over Chocolate Milk.” The New York Times, August 24, 2010. 2 Newton, John. “Trends in Beverage Milk Consumption.” Dairy Business News, January 5, 2018. 3 Packaged Facts. “Dairy and Dairy Alternative Beverage Trends in the U.S., 4th Edition,” 2017. -

USDA Child and Adult Care Food Program Milk Component
USDA CHILD AND ADULT CARE FOOD PROGRAM Milk Component This handout provides information about the new milk requirements for children 1 year and older and adult participants in the Adult Care Component. A separate handout on the new infant meal pattern requirements will be distributed. The term Program refers to all facility types: group child care centers, family day care homes, afterschool programs, emergency shelters and adult care centers. New Requirements Flavored Milk & Syrup Effective October 1, 2017 Children 1 through 5 years old • Flavored milk is not allowed as part of a • Milk served to one year olds must be unflavored whole milk. reimbursable meal. • A one-month transition period is allowed for children 24 • months to 25 months old. They may have whole or reduced- Syrup (including zero calorie and sugar-free fat (2%) milk as they transition to low-fat (1%) or fat-free syrups) cannot be added to unflavored milk because this (skim) milk. turns the beverage into flavored milk. • Flavored milk, including flavored non-dairy beverages, Children ages 6 years and older and adult participants cannot be served to children 1 through 5 years old. • If served, flavored milk must be fat-free. • Fat-free flavored milk and flavored non-dairy beverages can • Syrup (including zero calorie and sugar-free syrups) may only be served to children 6 years and older, as well as adult be added to fat-free (skim) milk. participants. • Adult Care Centers Only: Yogurt (6 ounces by weight or ¾ Why Can’t Flavored Milk be served to cup by volume) may be served to adults in place of fluid milk Children under 6 Years Old? once per day. -

Borden Dairy of Florida 308 Ave G SW Winter Haven, FL 33880 M&B
THE SCHOOL DISTRICT OF LEE COUNTY Borden Dairy of Florida M&B Products, Inc. DEPARTMENT OF PROCUREMENT SERVICES 308 Ave G SW 8601 Harney Road 2855 COLONIAL BLVD. FORT MYERS, FLORIDA 33966 Winter Haven, FL 33880 Temple Terrace, FL 33637 Fresh Milk and Other Dairy Products Phone: 813-230-5689 Phone: 813-988-2211 BID NO. B167267RC OPENING DATE: Tuesday Fax: 863-297-7402 Fax: 813-980-6596 April 21, 2016 @ 2:00 PM *** FOR ALL LINE ITEMS WITH "A" AND "B", THE E-mail: [email protected] E-mail: [email protected] ESTIMATED ANNUAL VOLUME IS COMBINED *** Est. Annual FMO 1/2 FMO 1/2 GROUP District Volume in Units per Brand/ Pint CO-OP Processor Estimated Units per Brand/ Pint CO-OP Processor A Item Description/ Unit of units Pckaging Pckaged Product (Variable Premium Vendor's Assessement Annual Total Pckaging Pckaged Product (Variable Premium Vendor's Assessement Estimated Annual ITEM # Spec Meas. (A) (Case,etc) Qty Code Cost) Cost Fixed Fee Fee Cost (Case,etc) Qty Code Cost) Cost Fixed Fee Fee Total Cost Low Fat Milk, 1%, Recyclable Borden / Cool 1.a Plastic Coated Half Pint 3,400,000 Plastic Case 50 $0.07160 $0.02130 $0.07970 $0.00110 $590,580.00 Corrugated 35 $ 0.10310 $ 0.00860 $ 0.06320 $ 0.00110 $598,400.00 25351 Cow / Paper Cartons Tray 1008 Low Fat Milk, 1%, Plastic Bottle 1.b Half Pint NO BID NO BID *Sample Required* Non Fat, Skim, Flavored Milk, Recyclable Chocolate, 0.4% or Borden/ 2.a Half Pint 7,900,000 Plastic Case 50 $0.05780 $0.01890 $0.09730 $0.00100 $1,382,500.00 Corrugated 35 $ 0.10310 $ 0.00860 $ 0.06470 $ 0.00110 -

Chapter 1530 Department of Agriculture Milk, Milk Products, and Standards
MINNESOTA RULES 1985 MILK, MILK PRODUCTS, AND STANDARDS 776 CHAPTER 1530 DEPARTMENT OF AGRICULTURE MILK, MILK PRODUCTS, AND STANDARDS MILK AND CREAM AND RELATED PRODUCTS 1530.0480 CULTURED MILK OR CULTURED 1530.0010 DEFINITIONS. WHOLE MILK BUTTERMILK. 1530.0020 MILK. 1530.0490 COTTAGE CHEESE. 1530.0030 COAT MILK. 1530.0500 CREAMED COTTAGE CHEESE. 1530.0040 EWE MILK. 1530.0510 CREAMING MIXTURE. 1530.0050 CREAM. 1530.0520 OTHER OPTIONAL INGREDIENTS. 1530.0060 HOMOGENIZED CREAM. 1530.0530 STABILIZING INGREDIENTS. 1530.0070 SOUR CREAM. CULTURED SOUR 1530.0540 DIOCTYL SODIUM SULFOSUCCINATE. CREAM. 1530.0550 PASTEURIZATION OF CREAMING 1530.0080 LIGHT CREAM. COFFEE CREAM. OR MIXTURE. TABLE CREAM. 1530.0560 D1ACETYL STARTER DISTILLATE OR 1530.0090 WHIPPED LIGHT CREAM. COFFEE OTHER FLAVORING SUBSTANCES. CREAM. OR TABLE CREAM. 1530.0570 DEFINITIONS. 1530.0100 WHIPPING CREAM. 1530.0580 LABEL STATEMENTS. 1530.0110 LIGHT WHIPPING CREAM. 1530.0590 LABEL STATEMENT REGARDING 1530.0120 HEAVY CREAM OR HEAVY WHIPPING ARTIFICIAL FLAVORING. CREAM. 1530.0600 LABEL DECLARATIONS TO BE USED 1530.0130 WHIPPED CREAM. IN CONJUNCTION WITH "CREAMED 1530.0140 HALF AND HALF. COTTAGE CHEESE." 1530.0150 SOUR HALF AND HALF OR 1530.0610 VITAMIN D MILK AND MILK CULTURED HALF AND HALF. PRODUCTS. 1530.0160 DRY MILK. DRY MILK SOLIDS. 1530.0620 FORTIFIED MILK PRODUCTS. 1530.0170 NONFAT DRY MILK. 1530.0630 RECONSTITUTED OR RECOMBINED 1530.0180 INSTANT NONFAT DRY MILK. MILK AND MILK PRODUCTS. 1530.0190 CONDENSED SKIM MILK. 1530.0640 STERILIZED MILK. EVAPORATED SKIM MILK. 1530.0650 HOMOGENIZED MILK AND CONCENTRATED SKIM MILK. HOMOGENIZED MILK PRODUCTS. 1530.0200 SWEETENED CONDENSED SKIM 1530.0660 WHEY. MILK. 1530.0670 CONCENTRATED MILK TO BE 1530.0210 DRY BUTTERMILK.