Taurine Depletion and Schwann Cell Dysfunction in Diabetic Neuropathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PROVISIONAL PEER-REVIEWED TOXICITY VALUES for VANADIUM and ITS SOLUBLE INORGANIC COMPOUNDS OTHER THAN VANADIUM PENTOXIDE (CASRN 7440-62-2 and Others)
EPA/690/R-09/070F l Final 9-30-2009 Provisional Peer-Reviewed Toxicity Values for Vanadium and Its Soluble Inorganic Compounds Other Than Vanadium Pentoxide (CASRN 7440-62-2 and Others) Derivation of Subchronic and Chronic Oral RfDs Superfund Health Risk Technical Support Center National Center for Environmental Assessment Office of Research and Development U.S. Environmental Protection Agency Cincinnati, OH 45268 Commonly Used Abbreviations BMD Benchmark Dose IRIS Integrated Risk Information System IUR inhalation unit risk LOAEL lowest-observed-adverse-effect level LOAELADJ LOAEL adjusted to continuous exposure duration LOAELHEC LOAEL adjusted for dosimetric differences across species to a human NOAEL no-observed-adverse-effect level NOAELADJ NOAEL adjusted to continuous exposure duration NOAELHEC NOAEL adjusted for dosimetric differences across species to a human NOEL no-observed-effect level OSF oral slope factor p-IUR provisional inhalation unit risk p-OSF provisional oral slope factor p-RfC provisional inhalation reference concentration p-RfD provisional oral reference dose RfC inhalation reference concentration RfD oral reference dose UF uncertainty factor UFA animal to human uncertainty factor UFC composite uncertainty factor UFD incomplete to complete database uncertainty factor UFH interhuman uncertainty factor UFL LOAEL to NOAEL uncertainty factor UFS subchronic to chronic uncertainty factor i FINAL 9-30-2009 PROVISIONAL PEER-REVIEWED TOXICITY VALUES FOR VANADIUM AND ITS SOLUBLE INORGANIC COMPOUNDS OTHER THAN VANADIUM PENTOXIDE (CASRN 7440-62-2 and others) Background On December 5, 2003, the U.S. Environmental Protection Agency's (U.S. EPA) Office of Superfund Remediation and Technology Innovation (OSRTI) revised its hierarchy of human health toxicity values for Superfund risk assessments, establishing the following three tiers as the new hierarchy: 1) U.S. -

1 Abietic Acid R Abrasive Silica for Polishing DR Acenaphthene M (LC
1 abietic acid R abrasive silica for polishing DR acenaphthene M (LC) acenaphthene quinone R acenaphthylene R acetal (see 1,1-diethoxyethane) acetaldehyde M (FC) acetaldehyde-d (CH3CDO) R acetaldehyde dimethyl acetal CH acetaldoxime R acetamide M (LC) acetamidinium chloride R acetamidoacrylic acid 2- NB acetamidobenzaldehyde p- R acetamidobenzenesulfonyl chloride 4- R acetamidodeoxythioglucopyranose triacetate 2- -2- -1- -β-D- 3,4,6- AB acetamidomethylthiazole 2- -4- PB acetanilide M (LC) acetazolamide R acetdimethylamide see dimethylacetamide, N,N- acethydrazide R acetic acid M (solv) acetic anhydride M (FC) acetmethylamide see methylacetamide, N- acetoacetamide R acetoacetanilide R acetoacetic acid, lithium salt R acetobromoglucose -α-D- NB acetohydroxamic acid R acetoin R acetol (hydroxyacetone) R acetonaphthalide (α)R acetone M (solv) acetone ,A.R. M (solv) acetone-d6 RM acetone cyanohydrin R acetonedicarboxylic acid ,dimethyl ester R acetonedicarboxylic acid -1,3- R acetone dimethyl acetal see dimethoxypropane 2,2- acetonitrile M (solv) acetonitrile-d3 RM acetonylacetone see hexanedione 2,5- acetonylbenzylhydroxycoumarin (3-(α- -4- R acetophenone M (LC) acetophenone oxime R acetophenone trimethylsilyl enol ether see phenyltrimethylsilyl... acetoxyacetone (oxopropyl acetate 2-) R acetoxybenzoic acid 4- DS acetoxynaphthoic acid 6- -2- R 2 acetylacetaldehyde dimethylacetal R acetylacetone (pentanedione -2,4-) M (C) acetylbenzonitrile p- R acetylbiphenyl 4- see phenylacetophenone, p- acetyl bromide M (FC) acetylbromothiophene 2- -5- -

Vanadium in Biosphere and Its Role in Biological Processes
Biological Trace Element Research https://doi.org/10.1007/s12011-018-1289-y Vanadium in Biosphere and Its Role in Biological Processes Deepika Tripathi1 & Veena Mani1 & Ravi Prakash Pal1 Received: 9 July 2017 /Accepted: 26 February 2018 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Ultra-trace elements or occasionally beneficial elements (OBE) are the new categories of minerals including vanadium (V). The importance of V is attributed due to its multifaceted biological roles, i.e., glucose and lipid metabolism as an insulin-mimetic, antilipemic and a potent stress alleviating agent in diabetes when vanadium is administered at lower doses. It competes with iron for transferrin (binding site for transportation) and with lactoferrin as it is secreted in milk also. The intracellular enzyme protein tyrosine phosphatase, causing the dephosphorylation at beta subunit of the insulin receptor, is inhibited by vanadium, thus facilitating the uptake of glucose inside the cell but only in the presence of insulin. Vanadium could be useful as a potential immune-stimulating agent and also as an antiinflammatory therapeutic metallodrug targeting various diseases. Physiological state and dose of vanadium compounds hold importance in causing toxicity also. Research has been carried out mostly on laboratory animals but evidence for vanadium importance as a therapeutic agent are available in humans and large animals also. This review examines the potential biochemical and molecular role, possible kinetics and distribution, essentiality, immunity, and toxicity- related study of vanadium in a biological system. Keywords Metabolic role . Insulin-mimetic . Biological function . Vanadium Introduction essential elements^ which include aluminum (Al), arsenic (As), cobalt (Co), chromium (Cr), fluorine (F), molybdenum Minerals are inorganic elements, without carbon, found in (Mo), nickel (Ni), silicon (Si), tin (Sn), and vanadium (V) [4]. -

Sports Nutrition: a Review of Selected Nutritional Supplements for Bodybuilders and Strength Athletes
Sports Nutrition: A Review of Selected Nutritional Supplements For Bodybuilders and Strength Athletes Gregory S. Kelly, N.D. Abstract Because there is widespread belief among athletes that special nutritional practices will enhance their achievements in competition, the use of supplements has become common. Accompanying the growth in supplementation by athletes has been a corresponding increase in exaggerated claims or misleading information. This article reviews several supplements currently popular among bodybuilders and other strength athletes in order to clarify which products can be expected to produce results. Included in the discussion are creatine monohydrate, beta-hydroxy beta-methylbutyrate, whey protein, phosphatidylserine, and selected amino acids and minerals. (Alt Med Rev 1997; 2(3):184-201) Introduction The increased focus on fitness and subsequent research in the exercise field has ex- panded the role of nutrition as it relates to sports performance. Because there is widespread belief among athletes that special nutritional practices will enhance their achievements in com- petition, the use of supplements has become common. Although some of the supplements have proven benefits, historically a great deal of the information on products is either misleading or exaggerated. This is perhaps best witnessed in the products marketed to bodybuilders and other athletes concerned with size, strength, and body composition. This article reviews some of the supplements currently promoted in this market in an effort to determine which contribute to maximizing results. Included in the review are creatine monohydrate, beta-hydroxy beta- methylbutyrate (HMB), whey protein, phosphatidylserine, and selected amino acids and minerals. Creatine Monohydrate Creatine monohydrate has become one of the most popular supplements in the history of bodybuilding. -

Dietary Supplements Compendium Volume 1
2015 Dietary Supplements Compendium DSC Volume 1 General Notices and Requirements USP–NF General Chapters USP–NF Dietary Supplement Monographs USP–NF Excipient Monographs FCC General Provisions FCC Monographs FCC Identity Standards FCC Appendices Reagents, Indicators, and Solutions Reference Tables DSC217M_DSCVol1_Title_2015-01_V3.indd 1 2/2/15 12:18 PM 2 Notice and Warning Concerning U.S. Patent or Trademark Rights The inclusion in the USP Dietary Supplements Compendium of a monograph on any dietary supplement in respect to which patent or trademark rights may exist shall not be deemed, and is not intended as, a grant of, or authority to exercise, any right or privilege protected by such patent or trademark. All such rights and privileges are vested in the patent or trademark owner, and no other person may exercise the same without express permission, authority, or license secured from such patent or trademark owner. Concerning Use of the USP Dietary Supplements Compendium Attention is called to the fact that USP Dietary Supplements Compendium text is fully copyrighted. Authors and others wishing to use portions of the text should request permission to do so from the Legal Department of the United States Pharmacopeial Convention. Copyright © 2015 The United States Pharmacopeial Convention ISBN: 978-1-936424-41-2 12601 Twinbrook Parkway, Rockville, MD 20852 All rights reserved. DSC Contents iii Contents USP Dietary Supplements Compendium Volume 1 Volume 2 Members . v. Preface . v Mission and Preface . 1 Dietary Supplements Admission Evaluations . 1. General Notices and Requirements . 9 USP Dietary Supplement Verification Program . .205 USP–NF General Chapters . 25 Dietary Supplements Regulatory USP–NF Dietary Supplement Monographs . -

Vanadyl Sulphate EINECS No. 248-652-7; CAS No
Vanadyl sulphate EINECS No. 248-652-7; CAS No. 27774-13-6 The purpose of the Pre-SIEF is for REACH Pre-Registrants to agree upon 'sameness' of substance. Pre-registrants that agree upon the sameness of substance will then pass into the Substance Information Exchange Forum (SIEF) for that substance, where the data-sharing discussion begins and is coordinated by the SIEF Facilitator. All pre-registrants for vanadyl sulphate have received an e-mail to participate in the ‘Substance Sameness’ discussion. Your response to that survey is your participation in the Pre-SIEF ‘sameness’ discussion. If you would like to receive the ‘Substance Sameness’ survey, please contact the Vanadium Consortium. The typical composition for this substance can be checked below. Substance Vanadium oxide sulphate Synonym Vanadyl sulfate Chemical Formula VOSO4 CAS Number 27774-13-6 EINECS Number 248-652-7 Molecular weight (g/mol) 163.0 Typical composition Mass (%) Purity min. 97 Vanadium min. 19.5 Arsenic ≤ Chromium ≤ Aluminum ≤ 1 Calcium ≤ Copper ≤ Iron ≤ 1 Manganese ≤ Molybdenum ≤ Phosphorus ≤ 1 Potassium ≤ 1 Silicon ≤ 0.01 Sodium ≤ 1 Other impurities ≤ 0.01 The REACH Vanadium Consortium, Auer von Welsbach Straße 1, A-9330 Althofen, Austria, www.vanadiumconsortium.com is a voluntary industry scheme that invites all organisations and individuals involved in the vanadium business, which have a current or future interest in the European market, to join the consortium. The Vanadium Consortium and the Consortium Manager do not accept any liability with regard to the content or use of information contained in this website. Users are reminded that the information on this website does not constitute any legal advice. -

Vanadium/ Vanadyl Sulfate
Alternative Medicine Review Volume 14, Number 2 2009 Monograph 23 V 24 Vanadium/ Vanadium Cr Vanadyl Sulfate Chromium 41 42 Nb Mo Niobium Molybdenum Introduction The chemical element vanadium was first discovered by Spanish-born Mexican mineralogist, Andrés Manuel del Río, in 1801. He originally named the element “panchromium” because of the spectrum of colors associated with various oxides of the metal, but changed the name to “erythronium,” because most of the mineral salts turned red upon heating. Later, del Rio was convinced by fellow scientists that he had really found impure chromium and not a new element. To his regret, that same element was “rediscovered” 30 years later by Swedish chemist, Nils Gabriel Sefstrom, who named it vanadium, after the Nordic goddess of beauty, Vanadis (Freyja).1 Nutritionally, vanadium is thought to be a cofactor in various enzymatic reactions. Data from animal and human studies suggest vanadium mimics the action of insulin.2 Consequently, it may serve a beneficial role in promot- ing healthy glucose metabolism in individuals with diabetes or dysglycemia. Dietary sources for vanadium include mushrooms, shellfish, black pepper, parsley, dill seed, and grains. Biochemistry Vanadium is considered an essential nutrient in some animals.3 For instance, vanadium is essential in the diets of chickens; a deficiency has an adverse affect on bones, feathers, and blood. In humans, classification of vanadium as an “essential nutrient” is still a topic of debate among various research groups.3 Some consider vanadium to be an ultra- trace element, requiring dietary intake of only 20 mcg per day.4 Certain mushrooms species, such as Amanita muscaria, contain amavadine, (S,S)-2,20-(hydroxyimino) di- propionic acid (V[hida]2), a natural, vanadium-containing compound thought to act as a mediator in the oxidation of thiol compounds with carboxylic or ester groups, such as cysteine and glutathione.3 Various forms of vanadium are used in foods or supplements, or found in drinking water. -

Kinetic Study of the Dissolution of Vanadyl Sulfate and Vanadium
Kinetic study of the dissolution of vanadyl sulfate and vanadium pentoxide in sulfuric acid aqueous solution Ranine El Hage, Fabien Chauvet, Béatrice Biscans, Laurent Cassayre, L. Maurice, Théodore Tzedakis To cite this version: Ranine El Hage, Fabien Chauvet, Béatrice Biscans, Laurent Cassayre, L. Maurice, et al.. Kinetic study of the dissolution of vanadyl sulfate and vanadium pentoxide in sulfuric acid aqueous solution. Chemical Engineering Science, Elsevier, 2019, 199, pp.123-136. 10.1016/j.ces.2019.01.024. hal- 02290658 HAL Id: hal-02290658 https://hal.archives-ouvertes.fr/hal-02290658 Submitted on 17 Sep 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. OATAO is an open access repository that collects the work of Toulouse researchers and makes it freely available over the web where possible This is an author’s version published in: http://oatao.univ-toulouse.fr/24225 Official URL: https://doi.org/10.1016/j.ces.2019.01.024 To cite this version: El Hage, Ranine and Chauvet, Fabien and Biscans, Béatrice and Cassayre, Laurent and Maurice, L. and Tzedakis, Théo Kinetic study of the dissolution of vanadyl sulfate and vanadium pentoxide in sulfuric acid aqueous solution. -
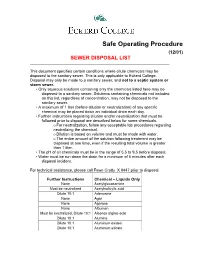
Safe Operating Procedure (12/01) SEWER DISPOSAL LIST ______
Safe Operating Procedure (12/01) SEWER DISPOSAL LIST ________________________________________________________________ This document specifies certain conditions where dilute chemicals may be disposed to the sanitary sewer. This is only applicable to Eckerd College. Disposal may only be made to a sanitary sewer, and not to a septic system or storm sewer. • Only aqueous solutions containing only the chemicals listed here may be disposed to a sanitary sewer. Solutions containing chemicals not included on this list, regardless of concentration, may not be disposed to the sanitary sewer. • A maximum of 1 liter (before dilution or neutralization) of any specific chemical may be placed down an individual drain each day. • Further instructions regarding dilution and/or neutralization that must be followed prior to disposal are described below for some chemicals. o For neutralization, follow any acceptable lab procedures regarding neutralizing the chemical. o Dilution is based on volume and must be made with water. o The entire amount of the solution following treatment may be disposed at one time, even if the resulting total volume is greater than 1 liter. • The pH of all chemicals must be in the range of 5.5 to 9.5 before disposal. • Water must be run down the drain for a minimum of 5 minutes after each disposal incident. For technical assistance, please call Fawn Crotty X 8447 prior to disposal. Further Instructions Chemical – Liquids Only None Acetylglucosamine Must be neutralized Acetylsalicylic acid Dilute 10:1 Adenosine None Agar None Agarose -

Sport Supplementation
Sport Supplementation Richard B. Kreider, PhD, FACSM, FASEP, FISSN, FACN, FNAK Professor & Executive Director, Human Clinical Research Facility Director, Exercise & Sport Nutrition Lab Department of Health & Kinesiology Texas A&M University [email protected] ExerciseAndSportNutritionLab.com hcrf.tamu.edu Disclosures: Receive industry sponsored research grants and serve as a scientific and legal consultant. Diploma in Nutrition and Training for the Change of Body Composition Sport Supplementation (Module 4) Training Stimulus Optimal Training/Diet Overtraining / Inadequate Diet Performance Undertraining/Poor Diet Training Volume/Intensity Kreider, R.B., A.C. Fry, and M.L. O'Toole (Eds.) Overtraining in Sport. Human Kinetics Publishers, Champaign, IL, 1998, 403 p. Diploma in Nutrition and Training for the Change of Body Composition Sport Supplementation (Module 4) Ergogenic Aid Any training technique, mechanical device, nutritional practice, pharmacological method, or psychological technique that can improve exercise performance capacity and/or enhance training adaptations. Kerksick et al., JISSN. In press, 2018 Diploma in Nutrition and Training for the Change of Body Composition Sport Supplementation (Module 4) Ergogenic Aid Analysis • Does the theory make sense? • Is there any scientific evidence supporting the ergogenic value? • Is it legal and/or safe? Kerksick et al., JISSN. In press, 2018 Diploma in Nutrition and Training for the Change of Body Composition Sport Supplementation (Module 4) Ergogenic Aids Scientific Evidence? • Studies on athletes or trained subjects? • Employed a double blind, repeated measures, placebo controlled, randomized clinical design? • Appropriate statistical interpretation? • Do claims match results? • Data presented at reputable scientific meeting and/or published in peer‐reviewed journal? • Results replicated by others? • Disclosures and competing interest declared? Kerksick et al., JISSN. -

The State of the Science in Sport Nutrition
The State of the Science in Sport Nutrition Richard B. Kreider, PhD, FACSM, FASEP, FISSN, FACN, FNAK Professor & Executive Director, Human Clinical Research Facility Director, Exercise & Sport Nutrition Lab Department of Health & Kinesiology Texas A&M University [email protected] ExerciseAndSportNutritionLab.com hcrf.tamu.edu Disclosures: Receive industry sponsored research grants and serve as a scientific and legal consultant. Performance Enhancement Pyramid Ergogenic Aids Optimize Recovery Energy & Macronutrient Sufficient and Well-Timed Diet Science-Based Training Ergogenic Aid Any training technique, mechanical device, nutritional practice, pharmacological method, or psychological technique that can improve exercise performance capacity and/or enhance training adaptations. Kerksick et al., JISSN. 15:38, 2018 Nutritional Ergogenic Aids Categories • Strong Evidence to Support Efficacy and Apparently Safe • Limited or Mixed Evidence to Support Efficacy • Little to No Evidence to Support Efficacy and/or Safety Kerksick et al., JISSN. 15:38, 2018 Nutritional Needs of Active Individuals and Athletes Energy Needs • General Fitness Training (e.g., 30 - 40 min/d; 3 d/wk) . Exercise energy expenditure generally 200 – 400 kcals/workout . Energy needs can be met on normal diet (e.g., 1,800 – 2,400 kcals/day or about 25 - 35 kcals/kg/day for a 50 – 80 kg individual) • Moderate Training (e.g., 2-3 hrs/d; 5-6 d/wk) . Exercise energy expenditure generally 600 – 1,200 kcals/hour . Caloric needs may approach 40 – 70 kcals/kg/day (2,000 – 7,000 kcals/day for a 50 – 100 kg athlete) • Elite Athletes (e.g., 3-6 hrs/d; 5-6 d/wk) . Caloric needs are typically 70 – 90 kcals/kg/day (3,500 – 9,000 kcals/day for a 50 – 100 kg athlete) with energy expenditure in Tour de France reported as high as 12,000 kcals/day (150 - 200 kcals/kg/d for a 60 – 80 kg athlete) . -

The Role for Vitamin and Mineral Supplements in Diabetes Management D
The Role for Vitamin and Mineral Supplements in Diabetes Management D. Enette Larson-Meyer, PhD, RD, FACSM Saturday, February 18, 2017 11:30 a.m. – 12:15 p.m. The American Diabetes Association Standards of Medical Care currently do not support the widespread use of vitamin and mineral supplements for diabetes management because of the lack of sufficient evidence. Cumulative evidence, however, suggests that supplementation with some vitamins and minerals has the potential to improve glycemic control, and macro- and microvascular complications in at least in some patients. This presentation will review key nutrients that may play a role in diabetes management including chromium, magnesium, vanadium, biotin, vitamins C, D, E and B12, and the scientific evidence supporting (or not supporting) their use either in supplemental doses or as part of a healthful diet and lifestyle pattern. References: 1. American Diabetes A. Standards of medical care in diabetes--2014. Diabetes Care 2014; 37 Suppl 1: S14-80. 2. Balk EM, Tatsioni A, Lichtenstein AH et al. Effect of chromium supplementation on glucose metabolism and lipids: a systematic review of randomized controlled trials. Diabetes Care 2007; 30: 2154-63. 3. Schwarz K, Mertz W. Chromium(III) and the glucose tolerance factor. Arch Biochem Biophys 1959; 85: 292-5. 4. Suksomboon N, Poolsup N, Yuwanakorn A. Systematic review and meta-analysis of the efficacy and safety of chromium supplementation in diabetes. J Clin Pharm Ther 2014; 39: 292-306. 5. National Institute of Health. Office of Dietary Supplements. Chromium: Dietary Supplements Fact sheet available at https://ods.od.nih.gov/factsheets/Chromium- HealthProfessional/.