Surgical Management of Metastatic Lesions of the Proximal Femur with Pathological Fractures Using Intramedullary Nailing Or Endoprosthetic Replacement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sichuan University(SCU) Is a National Key Comprehensive University, Incorporated
Sichuan University Sichuan University(SCU) is a national key comprehensive university, incorporated from three key universities, namely, the former Sichuan University, Chengdu University of Science and Technology (CUST) and West China University of Medical Science (WCUMS). Sichuan University offers courses in nine major fields of study including humanities, social sciences, natural sciences, engineering and technology, medical sciences,etc. Sichuan University 24,Southen Section1, 1st Ringroad, 610065, Sichuan,Chengdu, P.R. China Tel:+86-28-85402443 FAX:+86-28-85403260 E-mail:[email protected]. cn Contact Us Sitemap FAQ http://www.scu.org.cn/19.09.2003 01:34:23 Sichuan University SichuanUniversity 24,Southen Section1, 1st Ringroad, 610065, Sichuan,Chengdu, P.R. China Tel:+86-28-85402443 FAX:+86-28-85403260 E-mail:[email protected] E-mail:[email protected] http://www.scu.org.cn/CONT.htm19.09.2003 01:34:35 Sichuan University Home Genaral Information History of SCU About SCU A welcome from the President Eximious Schoolfellow Academics Degrees Admission Program Oversea Students Science Technology Medicine Research Literae Humaniores International Cooperation Library Resource Museum Hospital News&Events Map Campus Life Living Service Students' Assn. Foreign Experts Employment Overseas Schoolars http://www.scu.org.cn/sitemap.htm19.09.2003 01:34:52 Sichuan University General Information As one of the national key universities directly under the State Ministry of Education (MOE) as well as one of the State “211 Project” universities enjoying privileged construction in the Ninth Five-Year Plan period, the present Sichuan University (SCU) was first incorporated with Chengdu University of Science and Technology (CUST), another national key university under the MOE in1994, and West China General Information University of Medical Science (WCUMS), a key university directly subordinated to History of SCU the State Ministry of Health in 2000. -

Policy Tool Model and Its Application in the Governance of Characteristic Towns
Open Journal of Social Sciences, 2020, 8, 232-244 https://www.scirp.org/journal/jss ISSN Online: 2327-5960 ISSN Print: 2327-5952 Policy Tool Model and Its Application in the Governance of Characteristic Towns Dameng Luo, Yun Zhang Sichuan University of Arts and Sciences, Dazhou, China How to cite this paper: Luo, D. M., & Abstract Zhang, Y. (2020). Policy Tool Model and Its Application in the Governance of Cha- Policy tools are the mechanism by which policy ideas and policy goals are racteristic Towns. Open Journal of Social transformed into specific policy actions, the bridge connecting goals and re- Sciences, 8, 232-244. sults, and the necessary path for policy implementation. The choice of policy https://doi.org/10.4236/jss.2020.87019 tools will be affected by multiple factors such as policy environment, policy Received: June 26, 2020 objectives, policy objects, governance structure, and tool characteristics. And Accepted: July 19, 2020 constructed a policy tool selection model. Based on this theory, it analyzes the Published: July 22, 2020 selection of policy tools for characteristic towns in the fields of planning, com- Copyright © 2020 by author(s) and prehensive development, operation, investment and financing. The article be- Scientific Research Publishing Inc. lieves that the policy tools that can be used in the planning stage of characte- This work is licensed under the Creative ristic towns are: deregulation, decentralization, families and communities, so- Commons Attribution International cial organizations, public participation, contract outsourcing, etc. The policy License (CC BY 4.0). http://creativecommons.org/licenses/by/4.0/ tools that can be used in comprehensive development are: deregulation, fi- Open Access nancial allocation, contract outsourcing, public-private partnership, etc. -

Proteomic Comparison by Itraq Combined with Mass Spectrometry of Egg White Proteins in Laying Hens (Gallus Gallus) Fed with Soybean Meal and Cottonseed Meal
RESEARCH ARTICLE Proteomic comparison by iTRAQ combined with mass spectrometry of egg white proteins in laying hens (Gallus gallus) fed with soybean meal and cottonseed meal Tao He¤, Haijun Zhang, Jing Wang, Shugeng Wu, Hongyuan Yue, Guanghai Qi* Key Laboratory of Feed Biotechnology of Ministry of Agriculture, Feed Research Institute, Chinese Academy a1111111111 of Agricultural Sciences, Beijing, China a1111111111 ¤ Current address: Sichuan University, Chengdu, Sichuan, China a1111111111 * [email protected] a1111111111 a1111111111 Abstract Cottonseed meal (CSM) is commonly used in hens' diets to replace soybean meal (SBM). OPEN ACCESS However, the molecular consequences of this substitution remains unclear. To investigate the impact of this substitution at the molecular level, iTRAQ combined with biochemical Citation: He T, Zhang H, Wang J, Wu S, Yue H, Qi G (2017) Proteomic comparison by iTRAQ analysis was performed in Hy-Line W-36 hens supplemented with a mixed diet of CSM and combined with mass spectrometry of egg white SBM. Egg weight, albumen height, and Haugh unit were significantly reduced in the CSM100 proteins in laying hens (Gallus gallus) fed with group (100% crude protein of SBM replaced by CSM) compared with the SBM group soybean meal and cottonseed meal. PLoS ONE 12 (P 0.05). A total of 15 proteins, accounting for 75% of egg white proteins with various bio- (8): e0182886. https://doi.org/10.1371/journal. < pone.0182886 logical functions of egg whites, were found to be reduced. This finding may relate to the decrease of albumen quality in the CSM group. Oviduct magnum morphology and hor- Editor: Gotthard Kunze, Leibniz-Institut fur 100 Pflanzengenetik und Kulturpflanzenforschung mone analysis indicated that a reduced level of plasma progesterone caused reduced Gatersleben, GERMANY growth of the tubular gland and epithelial cells in the magnum, further decreasing egg white Received: March 19, 2016 protein synthesis in the magnum. -

Wu Mi's Educational Thoughts and Practice During The
ISSN 1927-0232 [Print] Higher Education of Social Science ISSN 1927-0240 [Online] Vol. 7, No. 1, 2014, pp. 158-167 www.cscanada.net DOI: 10.3968/5013 www.cscanada.org Wu Mi’s Educational Thoughts and Practice During the Period of the People’s Republic of China (PRC) LI Minyan[a],*; CUI Yanqiang[b] [a]Ph.D. Candidate, Faculty of Education, Southwest University, education and have endeavored to apply their rational Chongqing, China. thinking in teaching practice; with their wisdom, they [b]Professor, Faculty of Education, Southwest University, Chongqing, China. have promoted the development of China’s education. *Corresponding author. Wu Mi belongs to such a kind of educator. During the period of the Republic of China, he engaged himself in Received 12 February 2014; accepted 25 June 2014 the preservation of China’s traditional culture and made Published online 27 July 2014 a great contribution to the establishment of China’s comparative literature. Besides, he cultivated several Abstract dozens of scholars who were knowledgeable, had a As an educator who regarded education as his life, Wu thorough knowledge of both China and the West and Mi made a great contribution to the development of owned high moral character such as Qian Zhongshu1, the education of new China. This paper lays emphasis Wu Qichang2, Ji Xianlin3 for China; Wu Mi’s role in the on the investigation of Wu Mi’s educational practice establishment and development of China’s contemporary during the period of PRC, as well as on the expounding academy can never be overlooked. of the quintessence of Wu Mi’s educational practice and Wu Mi (1894-1978), whose personal name was thoughts in allusion to then situation of education through Yuseng and who was from Jingyang, Shannxi, west reading up historical materials. -
Institute of Mineral Resources, CAGS
2014 REPORTAnnual CHINESE ACADEMY OF GEOLOGICAL SCIENCES Geological Publishing House SUMMARY This Annual Report documents the work of the Chinese Academy of Geological Sciences in major aspects of 2014, covering management and supporting services in science and technology, representative research achievements, construction of key laboratories, international collaboration and exchanges, graduate education, and academic publications, and systematically outlines the advances of the Academy in development in the year 2014. The present work can serve as reference for those who are working and studying in the field of earth sciences or dealing with scientific and technological management as regards land and resources, and also for teachers and students engaged in relevant fields at colleges and universities. Technical Editors: TianYe Cataloging-in-Publication Data 2014 Annual Report Edited by Chinese Academy of Geological Sciences. -Beijing: Geological Publishing House, 2015.11 ISBN 978-7-116-09480-2 Ⅰ. ①Chinese... Ⅱ. ①Chinese... Ⅲ. ①Geology-research-China-2014-Annual -English Ⅳ. ①P5-54 Archives Library of Chinese Publications CIP data check number (2015) - 266146 图书在版编目(CIP)数据 中国地质科学院年报 . 2014 :英文 / 中国地质科学院编 . — 北京:地质出版社,2015. 11 ISBN 978-7-116-09480-2 Ⅰ. ①中... Ⅱ. ①中... Ⅲ. ①地质学-研究-中国- 2014 -年报-英文 Ⅳ. ① P5-54 中国版本图书馆 CIP 数据核字(2015)第 266146 号 © Geological Publishing House, 2015 Printed in China All rights reserved. No part of this book may be reproduced in any form without written permission from the publisher. Published and distributed by Geological -
The Chinese Air Force Evolving Concepts, Roles, and Capabilities
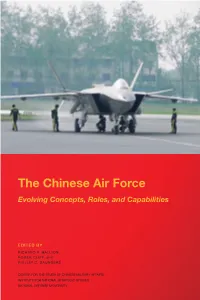
The Chinese Air Force Evolving Concepts, Roles, and Capabilities EDITED BY RICHARD P. HALLION, ROGER CLIFF, and PHILLIP C. SAUNDERS CENTER FOR THE STUDy OF CHINESE Military Affairs INSTITUTE FOR NATIONAL STRATEGIC STUDIES National DEFENSE UNIvERSITy Center for the Study of Chinese Military Affairs (CSCMA) The Center for the Study of Chinese Military Affairs (China Center) was established as an integral part of the National Defense University’s Institute for National Strategic Studies on March 1, 2000, pursuant to Section 914 of the 2000 National Defense Authorization Act. The China Center’s mission is to serve as a national focal point and resource center for multidisciplinary research and analytic exchanges on the national goals and strategic posture of the People’s Republic of China and to focus on China’s ability to develop, field, and deploy an effective military instrument in support of its national strategic objectives. Cover photo: China’s fifth-generation J–20 Stealth Fighter preparing for flight in Chengdu, Sichuan Province. (Photo by CCP/Color China Photo/AP Images) The Chinese Air Force Evolving Concepts, Roles, and Capabilities The Chinese Air Force Evolving Concepts, Roles, and Capabilities EDITED BY RICHARD P. HALLION, ROGER CLIFF, and PHILLIP C. SAUNDERS PUBLISHED BY NATIONAL DEFENSE UNIVERSITY PRESS FOR THE CENTER FOR THE STUDY OF CHINESE MILITARY Affairs INSTITUTE FOR NATIONAL STRATEGIC STUDIES WASHINGTON, D.C. 2012 Opinions, conclusions, and recommendations expressed or implied within are solely those of the contributors and do not necessarily represent the views of the U.S. Department of Defense or any other agency of the Federal Government. -

Sichuan University
SICHUAN UNIVERSITY SPECIAL ISSUE FOR 120TH ANNIVERSARY ISSUE 16 1896-2016 120th Anniversary of Sichuan University Sichuan University P02 Celebrates its 120th Anniversary The International Development P07 Strategy Advisory Board of SCU Established Alumni Worldwide Gather to P20 Promote Development of the Alma Mater Sichuan University 04 05 Sichuan University SICHUAN UNIVERSITY As one of the few prestigious universities in China, Sichuan University is devoted to world-class teaching, learning, and research, and to serving as an innovation engine that propels China to a new stage of development. With 34 colleges and professional graduate schools covering 12 categories of disciplines, Sichuan University is the most comprehensive university in the country. Our over 5200 faculties graduated from world renowned research universities give diverse and in-depth courses to our 37,000 undergraduate students and 20,000 graduate students, as well as over 3000 international students. Sichuan University provides generous financial supports to both domestic and international students. Sichuan University faculties actively engage the global knowledge network and push the limits of human knowledge in new energy, human health, material science, arts, and more. The full-spectrum of disciplines within Sichuan University is comparatively advantageous to encourage researchers of different areas to collaborate for complex challenges. Sichuan University alumni are people of profound social impact, who are policy makers in the central and provincial governments, academic professionals at research universities, and public and private sector professionals involved in today’s dynamic and global economy. Sichuan University has engaged the global academic community by establishing cooperative relationships with INTRODUCTION over 248 world renowned universities and research institutes in 32 countries and regions.