Textbook of Natural Medicine, 4Th Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![Water-Cures [Moss-2]](https://docslib.b-cdn.net/cover/2187/water-cures-moss-2-122187.webp)
Water-Cures [Moss-2]
Fountains ofYouth NEW JERSEY’S WATER-CURES his is a story about the bustling medical by Sandra W. marketplace in nineteenth-century New Moss M.D., M.A. T Jersey, and, in particular, the establishments known as water-cures. What we now call alternative, complementary, or holistic medicine was once referred to as sectarian medicine and its Sandra Moss. M.D., M.A. (History) practitioners as irregulars. Most regular or orthodox is a retired internist and past president of the Medical History Society of New Jersey. Dr. Moss writes and speaks physicians, often called "allopaths" by their critics, about the history of medicine in New Jersey. viewed the endless parade of irregular sectarian Acknowledgements: This paper is dedicated to the memory practitioners as either ignorant quacks or educated, of Professor David L. Cowen (1909-22006), New Jersey’s premier medical historian. Archivist Lois Densky-WWolff, but deluded, quacks. In order to get our bearings, Special Collections, University of Medicine and Dentistry of New Jersey, provided expert research assistance, as did we must look briefly at botanical and homeopathic the staff at Rutgers University Archives and Special sects before turning to the hydropaths, hygeio- Collections. therapists, and naturopaths. Fountains of Youth O Sandra W. Moss, MD, MA O GardenStateLegacy.com Issue 2 O December 2008 FROM JERSEY TEA struggling to make a living. Repeatedly TO JERSEY CURE stymied in its efforts to control Botanical medicine was a mainstay in practice through state licensing, the New Jersey from colonial times. “Herb regular medical establishment dithered “Water” and root” doctors and genuine (or for decades over the problem of by A.S.A. -

ECI Chronology
1 COPYRIGHT NOTICE: Graphs in this file are copyright protected by Joseph C. Keating, Jr., Ph.D., and may not be reproduced without permission; all rights reserved. Most, but not all, text materials are in the public domain. ___________________________________________________________________________________________ Chronology of the Eastern Chiropractic Institute (and other NY schools: New York, Standard, Carver, Columbia; 1944 and earlier; see also CINY/Chrono) word count: 89,820 filename: ECI/Chrono 11/13/97 Joseph C. Keating, Jr., Ph.D. Color Code: 1350 W. Lambert Rd., Apt. 110, La Habra CA 90631 USA Red & Magenta: questionable or uncertain information (310) 690-6499; E-mail: [email protected] Green: for emphasis Messages at LACC: (310) 947-8755, ext. 633 ___________________________________________________________________________________________ Name, date of founding or re-organization, and owner or status of Snyder, Martin, DC; CliniCorp, 31255 Cedar Valley Drive, Westlake several of the ancestor institutions of the: Village CA 91362 (friend of Ed Kimmel, CINY alumnus); (W: 818- 707-7244) Chiropractic Institute of New York Vincent, Richard E. Vincent, DC (CINY '50), F.I.C.C., President, Practice Resource Group, 27 Cambridge Street #100, Burlington MA 01803-4616, (800-545-5241) _____________________________________________ NY Brochures & Journals ordered from the Palmer Archives (items in blue not yet received): Annual Announcement, Columbia Institute [BJ LD 1211 .C7 C65 193-?] Annual Announcement, Standard School of Chiropractic, -

MAKING the CUT : What Exactly Is Naturopathy? By: Dr
MAKING THE CUT : What Exactly Is Naturopathy? By: Dr. William von Peters, N.M.D., Ph.N. President, First National University of Naturopathy and Allied Sciences Several weeks ago a researcher from a Medicine, which means the full scope of practice western University contacted me concerning as passed by Act of Congress and embodied in the First National University of Naturopathy as a Dictionary of Occupational Titles and its successor. part of a research project on the emergence of “We teach Naturopathy as it existed in its natural medicine. heyday of the 1920’s, 1930’s and 1940’s, when it As we spoke she asked me a question which was free to exist as a self-defined system of is commonly batted about in Naturopathy today, medicine, combined with the best of modern and went something like this: “There are two technology and science. It is integrated types of Naturopathy. There is that of the Naturopathic Medicine because we teach the Northwestern schools which espouse a medical integration of the various naturopathic paradigm, and then there is that of the modalities into Naturopathic practice. However, correspondence schools which espouse that of a it is not allopathic or integrated medicalism.” lower level of practice, more like that of a The researcher was astonished to learn that nutritional consultant.” She then asked me, there were more than the two positions. At First “Which is your school?” National University we absolutely stand for true, I responded, “I would like you to change historic Naturopathy. But what is the historical your view. There are actually three positions, not definition of true Naturopathy? two. -
A Comprehensive Listing of Books Written by Naturopaths / Naturopathic Doctors
A Comprehensive Listing of Books Written by Naturopaths / Naturopathic Doctors March 31st, 2019 Author(s) Yr Book Title Type of ISBN / ASIN Language World Region Country Publicati Publication on Abercrombie, Jenny 2018 The Vibrant Mom: Your Transformative Guide to a Restorative Book 978-1726200752 English North America USA Postpartum and a Happy, Healthy Motherhood Aesoph, Lauri M. 1996 How to Eat Away Arthritis: Gain Relief from the Pain and Book 978-0132428927 English North America USA Discomfort of Arthritis Through Nature's Remedies Afonso de Araújo, Manuel 2003 Como Prevenir e Tratar das Dores da Sua Coluna / Preventing Book 9.7973E+12 Portuguese Europe Portugal and Treating Your Pains Afonso de Araújo, Manuel 2003 Naturopatia – O Poder Curativo da Natureza / Naturopathy - Book 979-729-577-447-1 Portuguese Europe Portugal The Healing Power of Nature Afonso de Araújo, Manuel 2008 Osteopatia - Teoria e Prática / Osteopathy - Theory and Practice Book 9.78973E+12 Portuguese Europe Portugal Afonso de Araújo, Manuel 2002 Perca Peso, Ganhando Saúde - Medicina Natural / Lose Weight, Book 9.78973E+12 Portuguese Europe Portugal Gaining Health - Natural Medicine Aggarwal, Ameet 2018 Heal your body cure your mind. Leaky gut, adrenal fatigue, liver Book 978-1537231341 English North America Canada detox, mental health, Anxiety, depression, disease & trauma Ahlbrecht, Jens 2018 Pulsdiagnostik und Homöopathie Book 978-3981352818 German Europe Germany Airola, Paavo 1979 Are You Confused? The Authoritative Answers to Controversial Book B000WN4AWY English -

Naturopathic Physical Medicine
Naturopathic Physical Medicine Publisher: Sarena Wolfaard Commissioning Editor: Claire Wilson Associate Editor: Claire Bonnett Project Manager: Emma Riley Designer: Charlotte Murray Illustration Manager: Merlyn Harvey Illustrator: Amanda Williams Naturopathic Physical Medicine THEORY AND PRACTICE FOR MANUAL THERAPISTS AND NATUROPATHS Co-authored and edited by Leon Chaitow ND DO Registered Osteopath and Naturopath; Former Senior Lecturer, University of Westminster, London; Honorary Fellow, School of Integrated Health, University of Westminster, London, UK; Fellow, British Naturopathic Association With contributions from Additional contributions from Eric Blake ND Hal Brown ND DC Nick Buratovich ND Paul Orrock ND DO Michael Cronin ND Matthew Wallden ND DO Brian Isbell PhD ND DO Douglas C. Lewis ND Co-authors of Chapter 1: Benjamin Lynch ND Pamela Snider ND Lisa Maeckel MA CHT Jared Zeff ND Carolyn McMakin DC Foreword by Les Moore ND Joseph Pizzorno Dean E. Neary Jr ND Jr ND Roger Newman Turner ND DO David Russ DC David J. Shipley ND DC Brian K. Youngs ND DO Edinburgh London New York Oxford Philadelphia St Louis Sydney Toronto 2008 © 2008, Elsevier Limited. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior per- mission of the Publishers. Permissions may be sought directly from Elsevier’s Health Sciences Rights Department, 1600 John F. Kennedy Boulevard, Suite 1800, Philadelphia, PA 19103-2899, USA: phone: (+1) 215 239 3804; fax: (+1) 215 239 3805; or, e-mail: [email protected]. You may also com- plete your request on-line via the Elsevier homepage (http://www.elsevier.com), by selecting ‘Support and contact’ and then ‘Copyright and Permission’. -
Naturopathic Historical Reference
Naturopathic Historical Reference Naturopathic Historical Reference Acknowledgements The World Naturopathic Federation (WNF) greatly appreciates the participation of naturopathic educational institutions in providing the details required for this WNF Naturopathic Historical Reference: Canadian College of Naturopathic Medicine (CCNM), Canada; Collège Européen de Naturopathie Traditionnelle Holistique (CENATHO), France; Centro Andaluz de Naturopatía (CEAN), Spain; Naturopatska Sola (SAEKA), Slovenia; Wellpark College of Natural Therapies, New Zealand. This initiative was led by the Naturopathic Roots Committee with the following members including Heilpraktiker / naturopaths / naturopathic doctors (ND): Tina Hausser, Heilpraktiker, Naturopath - Chair (Spain) Dr. Iva Lloyd, ND (Canada) Dr. JoAnn Yánez, ND, MPH, CAE (United States) Phillip Cottingham, ND (New Zealand) Roger Newman Turner, ND (United Kingdom) Alfredo Abascal, Naturopath (Uruguay) © World Naturopathic Federation July 2017 (date provisional) All rights reserved. Publications of the World Naturopathic Federation can be obtained from our website at www.worldnaturopathicfederation.org. Requests for permission to reproduce or translate WNF publications – whether for sale or for noncommercial distribution – should be addressed to [email protected] All reasonable precautions have been taken by the World Naturopathic Federation to verify the information in this report. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the Copyright 2017 1 www.worldnaturopathicfederation.org interpretation and use of the material lies with the reader. In no event shall the World Naturopathic Federation be liable for damages arising from its use. Printed in Canada. Introduction: The following chart and naturopathic historical timeline is an overview of some of the key individuals that have contributed to the philosophies, theories and principles that make up naturopathy / naturopathic medicine. -
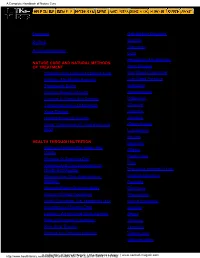
A Complete Handbook of Nature Cure
A Complete Handbook of Nature Cure Contents Foreword 49. Gall-Bladder Disorders 50. Gastritis Preface 51. Glaucoma Acknowledgements 52. Gout PART I . 53. Headaches And Migraine NATURE CURE AND NATURAL METHODS 54. Heart Disease OF TREATMENT 1. Principles And Practice Of Nature Cure 55. High Blood Cholesterol 2. Fasting - The Master Remedy 56. High Blood Pressure 3. Therapeutic Baths 57. Hydrocele 4. Curative Powers Of Earth 58. Hypoglycemia 5. Exercise In Health And Disease 59. Indigestion 6. Therapeutic Value Of Massage 60. Influenza 61. Insomnia 7. Yoga Therapy 8. Healing Power Of Colours 62. Jaundice 9. Sleep : Restorative Of Tired Body And 63. Kidney Stones Mind 64. Leucoderma 65. Neuritis PART II HEALTH THROUGH NUTRITION 66. Nepthritis Optimum Nutrition For Vigour And 10. 67. Obesity Vitality 68. Peptic Ulcer 11. Miracles Of Alkalizing Diet 69. Piles 12. Vitamins And Their Importance In Health And Disease 70. Premature Greying Of Hair 13. Minerals And Their Importance In 71. Prostate Disorders Nutrition. 72. Psoriasis 14. Amazing Power Of Amino Acids 73. Pyorrhoea 15. Secrets Of Food Combining 74. Rheumatism 16. Health Promotion The Vegetarian Way Sexual Impotence 75. 17. Importance Of Dietary Fibre 76. Sinusitis 18. Lecithin - An Amazing Youth Element 77. Stress 19. Role Of Enzymes In Nutrition. 78. Thinness 20. Raw Juice Therapy 79. Tonsillitis 21. Sprouts For Optimum Nutrition 80. Tuberculosis PART III 81. Varicose Veins http://www.healthlibrary.com/reading/ncure/index.htmA Collection of Sacred M (1a gofic 2)k |[5/19/1999 The Eso t9:11:19eric Lib PM]rary | www.sacred-magick.com A Complete Handbook of Nature Cure DISEASES AND THEIR NATURAL 82. -
Homemade Colon Cleansing Made Easy” 318 Chapter 39: What’S Next? Advanced Internal Cleansing 323 Chapter 40: Conclusion 325
©2008 by Mark Ament All rights reserved No part of this documentation may be reproduced, stored or transmitted in any form or by any means or used to produce derivative works, without written permission from the author. Published by: Healing Vibes Productions, 821 Stevens Ave. Solana Beach, CA 92075 USA 2 Legal Disclaimer: While all attempts have been made to verify information provided in this publication, neither the Author nor the Publisher assume any responsibility for errors, omissions or contrary interpretation of the subject matter herein. This publication is intended for informational purposes only. It is not intended to diagnose or treat any disease. And it is in no way intended as a substitute for sound medical advice. If you have any medical concerns whatsoever, consult a competent medical professional as is appropriate for you. This is especially important if you have any life threatening disease. The reader of this publication assumes all responsibility for the use of these materials and information. The Author and the Publisher assume no responsibility or liability whatsoever on the behalf of any purchaser or reader of these materials. This product contains links to web sites operated by other parties. Such links are provided for your convenience and reference only. We are not responsible for the content or products of any linked site or any link contained in a linked site. ©2008 by Mark Ament • www.healingvibes.com 3 TABLE OF CONTENTS INTRODUCTION 5 My Story with Colon Cleansing 5 Chapter 1 Read This First: “5 Steps to -

To the Followers of Naturopathy the Wonderful Human Machi
Index Publishers' Note Mahamrityunjaya Mantra What Is Life? What Is Disease? To the Followers of Naturopathy The Wonderful Human Machine The Human Body The Origin of Disease Health and Nature Cure Health and Law Of Nature Health and Conservation of Energy Health and Clothing The Secret of Living Health and Disease Vital Facts About Health Way to Radiant Health How to Keep Fit and Healthy Health and Psychology What Is Nature Cure'? Philosophy of Nature Cure Naturopathy and Spiritual Life Story of Nature Cure Fundamental Principles of Nature Cure Nature Cure Methods AIR FOR HEALTH AND CURE History of Water-cure How Water Serves As a Medical Agent Water Remedies Efficacy of Baths Cold Sponging Tepid Sponging Cold Rub Mud Cure SUN CURE How to Cure Diseases by Colour Power Influence of Colour on Health To the Celibates Aids to Brahmacharya Yogic Recipes for Brahmacharya Violation of Brahmacharya Self-restraint and Planned Parenthood EXERCISE MASSAGE CHIROPRACTIC SLEEP CARE OF TEETH Nature's Tonics Upanishads on Food Purpose of Food Constituents of Food Digestion Dietetic Treatment Diet and Health Protective Foods Cereals Proteins Pulses Germination of Pulses Vegetables Vegetable Salads Starches Mineral Salts Milk Fruits Fruit Salad Nuts Honey Dietetic Don'ts Different Qualities of Food Articles Incompatible Foods Dietetic Values of Fruits Rejuvenation Through Milk Treatment Fast and Its Importance Fasting and Its Benefits Fast Cure Methodical Breaking of Fasts Barley Bitter Gourd Bottle Gourd Buttermilk Kandang Kathri (kalyant) Mint Papaya -

Board of Health Professions Regulatory Research Committee Virtual
Board of Health Professions August 20, 2020 Regulatory Research Committee 9:09 a.m. Virtual Meeting 9960 Mayland Dr, Henrico, VA 23233 Due to the COVID-19 declared state of emergency and consistent with Amendment 28 to HB29 (Budget Bill for 2018-2020) and the applicable provisions of § 2.2- 3708.2 in the provisions of Freedom of Information Act, the Board convened a virtual meeting to consider such regulatory and business matters as presented on the agenda necessary for the board to discharge its lawful purposes, duties and responsibilities. An audio file of this meeting may be found here: https://www.dhp.virginia.gov/audio/BHP/FullBoardMeeting08202020.mp3 Board Member Attendance Virtual-Louise Hershkowitz, CRNA, MSHA, Board of Nursing Virtual-John Salay, MSW, LCSW, Board of Social Work In-Person-James Wells, RPH, Citizen Member Virtual-Martha S. Rackets, MS, Citizen Member Absent Louis R. Jones, Board of Funeral Directors & Embalmers Maribel Ramos, Citizen Member DHP Staff Virtual-Barbara Allison-Bryan, Chief Deputy Director DHP Virtual-David Brown, DC, Director DHP In-Person-Elizabeth A. Carter, PhD, Executive Director BHP In-Person-Laura Jackson, MSHSA, Operations Manager BHP Virtual-Yetty Shobo, PhD, Deputy Executive Director BHP Virtual-Corie Tillman-Wolf, Executive Director for the Boards of Funeral Directors & Embalmers, Long-Term Care Administrators and Physical Therapy Virtual-Elaine Yeatts, Senior Policy Analyst DHP Virtual Observers- Participant List Ashley Wright Baron Glassgow Ben Traynham C. Barrineau 1 1 Jo Twombly John Hanks K. Wilkinson Marie Rodriguez Mark (last name not provided) Richard Grossman Sarah Giardenelli Tim Faerber Tyler Cox Introductory Comments Chair Mr. -

Copyrighted Material Copyrighted Material
Copyrighted Material Copyrighted Material 3 Practice of Naturopathic Medicine in their own words Edited by SU ss A nn A CZERA N K O , ND, BBE Foreword by SHIRLEY Sno W , ND, DNB, HMD PO RTLA N D , OREG on Copyrighted Material 4 PRACTICE OF NATUR op ATHIC MEDICI N E Managing Editor: Sandra Snyder, Ph.D. Production: Fourth Lloyd Productions, LLC. Design: Richard Stodart Cover illustration: An artist's rendition of the buildings and facilities of Drs. Benedict and Louisa Lust's Health Resort, Yungborn, in Butler, New Jersey at the turn of the century. Back cover photo: Dr. E. K. Stretch © 2015 by NCNM PRESS All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without the prior written permission of the publisher, except where permitted by law. Published by NCNM PRESS National College of Natural Medicine 49 SW Porter Street Portland, Oregon 97201, USA www.ncnm.edu NCNM PRESS gratefully acknowledges the generous and prescient financial support of HEVERT USA which has made possible the creation and distribution of the In Their Own Words historical series. The HEVERT COLLECTION comprises twelve historical compilations which preserve for the healing professions significant and representational works from contributors to the historical Benedict Lust journals. Printed in the United States of America ISBN: 978-0-9771435-8-0 0-9771435-8-9 Library of Congress Control Number: 2015939366 Copyrighted Material 5 Precious and remarkable to honor, a century later, the ingenuity and innovation that the early Naturopaths brought to their mission of building our medicine in North America. -
Copyrighted Material Copyrighted Material
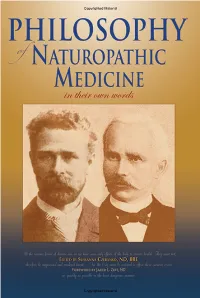
Copyrighted Material Copyrighted Material 3 Philosophy of Naturopathic Medicine in their own words Edited by SUSSA nn A CZERA N KO , ND, BBE Foreword by JARED L. ZEFF , ND PORTLA N D , OREGO N Copyrighted Material 4 PHILOSO P HY OF NATURO P ATHIC MEDICI N E Managing Editor: Sandra Snyder, Ph.D. Production: Fourth Lloyd Productions, LLC. Design: Richard Stodart Front cover photographs: Adolf Just (left) and Louis Kuhne (right). Back cover illustration: Louis Kuhne Sanitarium, 1899. © 2013 by NCNM PRESS All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without the prior written permission of the publisher, except where permitted by law. Published by NCNM PRESS National College of Natural Medicine 49 SW Porter Street Portland, Oregon 97201, USA www.ncnm.edu NCNM PRESS gratefully acknowledges the generous and prescient financial support of HEVERT USA which has made possible the creation and distribution of the In Their Own Words historical series. The HEVERT COLLECTION comprises twelve historical compilations which preserve for the healing professions significant and representational works from contributors to the historical Benedict Lust journals. Printed in the United States of America ISBN: 13-digit number 978-0-9771435-3-5 10-digit number 0-9771435-3-8 Copyrighted Material 5 Philosophy of Naturopathic Medicine is dedicated to Nature, whose immutable laws guided the historical giants of our medicine, Louis Kuhne and Adolf Just, to such a clear and profound understanding of her enduring power in healing.