Early and High SARS-Cov-2 Neutralizing Antibodies Are Associated with Severity in COVID-19 Patients from India
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA -

Pune Hospitals
PUNE PPN LIST OF HOSPITALS S No HOSPITAL NAME ADDRESS CITY STATE PIN CODE 1 Aadhar Hospital Off Bank Of India,Bombay Pune Highway,Dehuroad Pune Maharashtra 412101 Chakan Talegaon Road, Opp Marathi Shala, Ranubai Mala, 2 Aarogyam Multispeciality Hospital Pune Maharashtra 410501 Chakan 3 Aditya Birla Memorial Hospital Aditya Birla Memorial marg chinchwad Pune Maharashtra 411033 4 Aditya Eye Clinic M G Road Camp J A Kumar Plaza, Next To Wonderland Pune Maharashtra 411001 5 Aims Hospital & Research Centre Sr/No 154 Near Marutrao Gaikwad Garden Aundh Pune Maharashtra 411007 613,614 Sonkar Building, Behind Nav Maharashtra 6 Amrut Hospital Pune Maharashtra 411017 Vidyalaya, Pimpri-Waghere 7 Amrut Hospital & Research Centre Markal Road Alandi Devachi In front of TJSB Tal Khed Pune Maharashtra 412105 8 Anand Hospital Balaji Tower M.Phule Chowk Pune Maharashtra 410501 9 Anand Hospital Bhosari Opp. PMT Bus Stop, Bhosari Main CHowk, Bhosari Pune Maharashtra 411039 10 Ankur Multispeciality Hospital Sr No 40, Keshavnagar, Mundhwa, Pune Pune Maharashtra 411036 11 Ankur Nursing Home Plot No 11 Tanaji nagar, Link Road, Opp Hearitage Plaza Pune Maharashtra 411033 Sr No. 13/12, Pawar Nagar, Kalewadi Phata, Aundh-Ravet 12 Apex Hospital Pune Maharashtra 411033 Road, Thergaon, Pune Plot No.1,Sec-9,Sant Nagar,Spine Rood 13 Ashtavinayak Hospital Pune Maharashtra 412105 ,P.C.N.T.DA,Moshi Sakar 10, 3rd Floor, Above Fab India, Sassoon Road, Opp 14 Asian Eye Hospital Pune Maharashtra 411001 Jehangir Hospital 15 Astha Hospital SPINE ROAD PCMC Pune Maharashtra 411019 -

Hdfc Bank Branch List
HDFC BANK BRANCH LIST Sr. No. Branch Name Address Address : 93, Rajyog Creations Anand Park Off Iti Road 1 AUNDH Aundh Pune-411007 Maharashtra India 2 Address : S No 265 / 2 Baner Road Opposite Bharat Gas BANER Petrol Pump Baner Pune-411045 Maharashtra India Address : Patil Palace Ground Floor S. No 2/1 Nda 3 Pashan Road Bawdhan Pune 411021 Pune Bengaluru BAWDHAN Highway Bawdhan Pune-411021 Maharashtra India Address : Laukik Appt. , Ground Floor , Plot No. 3 , Cts 4 BHANDARKAR No. 870 Bhandarkar Rd Bhandarkar Road Pune-411004 ROAD Maharashtra India Address : S. No. 571, Crystal Room, Near Suryaprabha 5 Garden Kenjale Nagar Bibvewadi - Kondhwa Road BIBVEWADI Bibvewadi Pune-411037 Maharashtra India 6 Address : 9 / 2, Kalptaru Garden Opposite Narangi BOAT CLUB Baug Boat Club Road, Pune-411001 Maharashtra India Address : K. P. Housing Soceity General Thimmaiya 7 Road Camp, East Street Camp, Pune Pune-411001 EAST STREET Maharashtra India Address : Gr. Floor, Saraswati Commercial Complex, 8 Pune Satara Road, Opp Kushboo Hotel, Balaji Nagar, DHANKAWADI Dhankawadi Pune-411043 Maharashtra India Address : S. No 18 / B, P. No 06, “ Aargya Apartment “ Appartment No 101 / 102 Ground Floor Near Alankar 9 Police Chowky Erandvane Pune-411038 Maharashtra KARVE NAGAR India Address : Shop No. 22 Bldg. A, Tain Square Fatima 10 Nagar Road Wanowrie Fatima Nagar Pune-411013 WANOWRIE Maharashtra India Address : Destination Centre Upper Ground Floor 11 Magarpatta City Branch Hadapsar Pune-411013 MAGARPATTA Maharashtra India Address : Ground Floor, Dyandeep Complex, Jai 12 MOHAMMEDWA Bhavani Complex Mohammedwadi Hadapsar Pune- DI 411060 Maharashtra India Address : Upper Ground Floor Shop No.101,Victoria 13 Building Fortaleza Kalyani Nagar Pune-411006 KALYANINAGAR Maharashtra India Address : Ruby House - Sr. -
Sudarshan Chemical Industries Limited 162 Wellesley Road, Pune ‐ 411 001
SUDARSHAN CHEMICAL INDUSTRIES LIMITED 162 WELLESLEY ROAD, PUNE ‐ 411 001 Listi of Shareholders whose Interim Dividend for FY 2019‐20 is unpaid / unclaimed Investor First Name Investor Middle Name Investor Last Name Address Country State District Pin Code Folio Number DP Id‐Client Id‐ Unclaimed Account Amount Number A ANURADHA 11‐5‐453, F‐31 SRI SAI INDIA Andhra Pradesh 500004 SUDA0000000 6300.00 KRUPA APTS. RED HILLS 000A02697 HYDERABAD A ARUMUGASAMY BHARAT OFFSET INDIA MAHARASHTRA 444444 SUDA0000000 11781.00 PRINTERS 15 MEERA 000A00600 HUSAIN ST SIVAKASI A G NAIR RAM MEENA INDIA Kerala 682016 SUDA0000000 945.00 VALANJAMBALAM, 000A00855 COCHIN A GUNASEKARAN 31 BALAJI NAGAR 1ST INDIA Tamil Nadu 600014 SUDA0000000 2331.00 STREET ROYAPETTAH 000A00895 CHENNAI A K CHANDRASEKARAN C‐147, II CROSS STREET INDIA Tamil Nadu 600082 SUDA0000000 4725.00 JAWAHAR NAGAR 000A00771 CHENNAI A K PSCONSULTANTSPV C/O RPS SIDHU HOUSE INDIA Chandigarh 160010 IN300513‐ 819.00 TLTD NO 549 SECTOR 10 A 23467671‐0000 CHANDIGARH CHANDIGARD A K SMUTHUSAMY 3/3 RAMNAGAR 4TH INDIA Tamil Nadu 638602 SUDA0000000 2331.00 STREET TIRUPUR 000A00879 A KRISHNAMURTI 19 III BLOCK INDIA Karnataka 560011 SUDA0000000 1575.00 JAYANAGAR 000A00823 BANGALORE A N KRISHNAN NO 83/240‐4 (190/A) INDIA Karnataka 560075 SUDA0000000 1890.00 IST CROSS CHURCH 000A02251 STREET NEW THIPPASANDRA BANGALORE A PALANISAMY M/S KALAIVANI DYEING INDIA Tamil Nadu 638601 SUDA0000000 2331.00 FACTORY 1ST STREET 000A00881 PETHICHETTY PURAM TIRUPUR A R SHANTHA 13/1,7TH MAIN ROAD INDIA Karnataka 560019 SUDA0000000 1575.00 9TH CROSS N R COLONY 000A02098 BANGALORE A VIJAYASEKARAN C/O SAFIRE PRINTING INDIA Tamil Nadu 626123 SUDA0000000 2331.00 INKS N R K 000A00894 RAJARATNAM ROAD SIVAKASI ABDUL QADIR ABDULGANI SHIVPRASAD BUILDING INDIA Maharashtra 400052 IN300513‐ 252.00 2ND FLOOR FLAT NO 21 84058646‐0000 S V ROAD OLD KHAR WEST MUMBAI MUMBAI MAHARASHTRA ABDUL QADIR ABDULGANI SHIVPRASAD BUILDING INDIA Maharashtra 400052 12019101‐ 315.00 IInd FLOOR FLAT NO‐ 00560855‐SU00 21, S.V. -
Top Hundred Unpaid Challan Offender List Date 20-03-2020
TOP HUNDRED UNPAID CHALLAN OFFENDER LIST DATE 20-03-2020 Unpaid Challan Sr no Vehicle Number DIV NAME Unpaid Amount Vahan owner Name Vahan Permant Address Count DAGDU GANPATI MANDIR, WADULEBK, TAL- 1 MH14DC9134 A.NAGAR 44 8800 DAMAL SHIVAJI VINAYAK SHEVGAON, Ahmadnagar-414502 PLOT NO 16 SHIVAM SIDDHESHWAR, OPP 2 MH12NS2489 BANDGARDAN 37 15900 MAYURI PANDIT AMBEDKAR KRIDA SANKUL PADA , PUNE, -411009 13 TADIWALA RD, PUNE, PUNE 9762145368, - 3 MH12MY0472 bandgardan 35 17300 SATISH DAYARAM JAGTAP 411001 1482/13 , BHIMPURA LANE NR BABASAHE, 4 MH12JS5072 bandgarden 34 9100 GAUTAM KAMBLE AMBEDKAR BHAVAN , CAMP, PUNE, -411001 H.NO 190 VIDHYA NGR, S.NO 20/1 KATRAJ - 5 MH12KD9312 BHARATI.V 32 15800 RAJPUT DATTA SIDRAM KONDHWA ROAD, PUNE, -411046 S NO 18/2/7/3 FLAT NO10 SUMAN VIHAR, 6 MH12MJ5477 BHARATI.V 32 13300 LEENA THOPTE SUKHASAGAR KATRAJ, PUNE, -411046 S NO 36 SWAMI SAMARTH NAGAR, KATRAJ 7 MH12NM3144 BHARATI.V 32 14200 BHISE NEETA KONDHWA ROAD GOKUL NAGAR, PUNE, -411046 SRNO-381 HNO-2835 NR CHAITRABAN, BALAJI 8 MH12PV7178 BHARTI .V. 41 19,100 KOMAL RAM BHISE NAGAR SATARA ROAD, DHANKAWADI PUNE, Pune- 411043 FL NO.12,RAJIV GANDHI NAGAR,, NR.SHANI MANDIR,, 9 MH12NC7692 BHARTI .V. 40 17,200 SHANKAR DHAWARE PUNE, -411043 SR NO 37/15/263/957 GAONTHAN , SARAS SOC 10 MH12NY9419 BHARTI .V. 40 12,800 TEJASVI DURGE DHANKAWDI, PUNE, Pune-411043 LANE NO 17 SAI NAGAR , (GAYATRI VASTU), NEAR 11 MH12NZ4821 BHARTI .V. 38 18,300 PRAFULATA JASABHATI SALVE GARDEN, Pune-411048 SR NO 63 SAI NAGAR GALLI NO 2, NEAR DAS GIRANI 12 MH12PW6063 bharti v. -

Development of Inflectional Morphology and Its Effect on Reading Comprehension in Marathi Speaking Children – a Preliminary Study
================================================================= Language in India www.languageinindia.com ISSN 1930-2940 Vol. 15:4 April 2015 ================================================================= Development of Inflectional Morphology and Its Effect on Reading Comprehension in Marathi Speaking Children – A Preliminary Study Mrs. Madhavi Tambay B.Sc. (AST) Ms. Neha Nellangara Ms. Kajol Mutha ============================================================= Abstract The purpose of the study was three fold: one, to investigate the developmental trend of inflectional morphemes, second, to study the relation between morphological awareness and reading comprehension and lastly, to compare the development of inflection between genders. Marathi is an inflected and an agglutinative language; where affixes are attached to the root morpheme altering the person, number gender and tense. Marathi has poly-morphemic words and free word order. Hence knowledge of inflection is highly critical for comprehension of Marathi sentences. Sixty participants, thirty males and thirty females, from Grade III and Grade IV, were assessed on morphological awareness by a judgment task. Reading comprehension was assessed by answering questions on a reading passage. Results indicated significant developmental trend in inflectional morphemes from Grade III to Grade IV. Case marker was significant predictor of reading comprehension in grade III. No significant difference was observed between genders. We conclude that awareness of morphological skills improves reading comprehension and children start to read with meaning. The findings of this study and previous research suggest inclusion of assessment of morphological knowledge in early reading evaluation and intervention. It may also contribute to the assessment and intervention of children with learning disabilities. Keywords: Inflectional morphemes, Marathi, Morphological awareness, Reading comprehension. Language in India www.languageinindia.com ISSN 1930-2940 15:4 April 2015 Mrs. -

List of Approved Schools
List of approved Schools - PMC (As per RTE 25% Reservation) Capacity/Total Medium Board 25% RTE Sr.No UDISE Code School Name Address School Type School Entry Level Area Name Intake for 1st Name Name Seats Standard DR SHAMRAO KALMADI HIGH S.N.153, D.P. ROAD PARIHAR CHOWK 1 27251400106 English SSC Co-Education Nursery / Playgroup PMC 50 13 SCHOOL AUNDH PUNE 411007 2 27251400108 English D A V PUBLIC SCHOOL D.P.ROAD AUNDH PUNE 411007 CBSE Co-Education Nursery / Playgroup PMC 150 38 ARJAN WATUMULL SINDHU VIDHYA ARJAN WATUMULL SINDHU VIDHYA 3 27251400109 English BHAVAN,SIND CO-OPERATIVE SSC Co-Education Nursery / Playgroup PMC 90 23 BHAVAN,PUNE-411007 SOCIETY,AUNDH,PUNE-411007 SHRI KHANDERAI PRATISTHANCHE 4 27251400205 Marathi KHANDERAI PRATISHTAN PRI. PRATHMIK VIDYALAY , S/N. 4/2 , POST NIA, SSC Co-Education 1st Standard PMC 82 21 BALEWADI, PUNE 411 045. MITCON ROAD,IN FRONT OF MAMTA BHARATI VIDHYAPITH ENG MED 5 27251400208 English DINING HALL,BALEWADI,TAL-HAVELI,DIST- CBSE Co-Education Nursery / Playgroup PMC 80 20 SCHOOL,BALEWADI,PUNE - 45 PUNE SR.NO.80/1/2/1,BANER MAHALUNGE Junior Kg (LKG) / Mini KG / 6 27251400209 English THE ORCHID SCHOOL CBSE Co-Education PMC 105 26 ROAD,BANER,PUNE-411045 Balwadi (Chota Group) VINDYANCHAL S.NO.258,BALAJI PARK,BEHIND SEASONS Junior Kg (LKG) / Mini KG / 7 27251400210 English SSC Co-Education PMC 80 20 SCHOOL,AUNDH,BANER,PUNE-07 HOTEL AUNDH,BANER,PUNE-07 Balwadi (Chota Group) LATE.MADHAVRAO BHUSARI PATH Junior Kg (LKG) / Mini KG / 8 27251400307 English NEW INDIA ENG MEDIUM PRI RT:BHUSARI COLONY,PAUD SSC -

City Development Plan 2006-2012
Jawaharlal Nehru National Urban Renewal Mission PUNE City Development Plan 2006-2012 Volume I April 2006 Technical Assistance by FIRE (D) Project City Development Plan Pune Municipal Corporation CONTENTS EXECUTIVE SUMMARY .................................................................................................................................. 1 1.1. THE OPPORTUNITY IN THE FORM OF JNNURM................................................................................2 1.2. THE CITY DEVELOPMENT PLAN – A CORPORATION’S CORPORATE STRATEGY ................................2 1.3. ASSESSMENT OF INFRASTRUCTURE: STATUS AND KEY ISSUES ........................................................3 1.4. STRATEGIES FOR GROWTH ...............................................................................................................9 1.5. INVESTMENT REQUIREMENTS ........................................................................................................10 1.6. PMC’S INVESTMENT CAPACITY.....................................................................................................11 1.7. REFORM STRATEGY .......................................................................................................................12 2. PROJECT BACKGROUND.................................................................................................................. 14 2.1. BACKGROUND................................................................................................................................14 2.2. OBJECTIVES OF A CITY DEVELOPMENT -

Sr No Vehicle Number DIV NAME Unpaid Challan Count Unpaid
TOP 500 UNPAID CHALLAN OFFENDER LIST DATE 14-03-2020 Sr Vehicle Unpaid Unpaid DIV NAME Vahan owner Name Vahan Permant Address no Number Challan Amount Count DAGDU GANPATI MANDIR, WADULEBK, TAL- SHEVGAON, 1 MH14DC9134 A.NAGAR 44 8800 DAMAL SHIVAJI VINAYAK Ahmadnagar-414502 PLOT NO 16 SHIVAM SIDDHESHWAR, OPP AMBEDKAR KRIDA 2 MH12NS2489 BANDGARDAN 37 15900 MAYURI PANDIT SANKUL PADA , PUNE, -411009 3 MH12MY0472 BANDGARDAN 35 17300 SATISH DAYARAM JAGTAP 13 TADIWALA RD, PUNE, PUNE 9762145368, -411001 1482/13 , BHIMPURA LANE NR BABASAHE, AMBEDKAR 4 34 9100 MH12JS5072 BANDGARDAN GAUTAM KAMBLE BHAVAN , CAMP, PUNE, -411001 SR NO 63 SAI NAGAR GALLI NO 2, NEAR DAS GIRANI BHARATI.V 35 16500 5 MH12PW6063 NAVNATH RATHOD SANTOSH NAGAR, , Pune-411046 S NO 10 (OLD 8) SLUM REHABILITATION, AUTHORITY BLDG C 6 BHARATI.V MH12NN7312 34 14,200 RAHUL BHAGWAT TUPARE WING C2 F NO 206, PUNE, -411037 H.NO 190 VIDHYA NGR, S.NO 20/1 KATRAJ - KONDHWA 7 BHARATI.V MH12KD9312 32 15800 RAJPUT DATTA SIDRAM ROAD, PUNE, -411046 S NO 18/2/7/3 FLAT NO10 SUMAN VIHAR, SUKHASAGAR BHARATI.V 8 MH12MJ5477 32 13300 LEENA THOPTE KATRAJ, PUNE, -411046 S NO 36 SWAMI SAMARTH NAGAR, KATRAJ KONDHWA ROAD 9 BHARATI.V MH12NM3144 32 14200 BHISE NEETA GOKUL NAGAR, PUNE, -411046 SRNO-381 HNO-2835 NR CHAITRABAN, BALAJI NAGAR 10 BHARATI.V MH12PV7178 41 19,100 KOMAL RAM BHISE SATARA ROAD, DHANKAWADI PUNE, Pune-411043 11 MH12QN0564 BHARATI.V 41 17,500 LATA KUMBHAR 135 KUMBHARWADA KATRAJ, PUNE, , Pune-411046 FL NO.12,RAJIV GANDHI NAGAR,, NR.SHANI MANDIR,, PUNE, - 12 BHARATI.V MH12NC7692 40 17,200 SHANKAR -
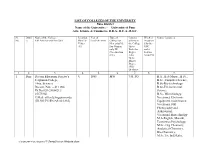
LIST of COLLEGES of the UNIVERSITY Pune District Name of the University: - University of Pune Arts, Science & Commerce, B.B.A., B.C.A., B.S.C
LIST OF COLLEGES OF THE UNIVERSITY Pune District Name of the University: - University of Pune Arts, Science & Commerce, B.B.A., B.C.A., B.S.C. Sr. Distri Name of the College, Location Year of Type of Courses Whether Course Conduced No. ct Full Address with Pin Code Rural ® Establish-ment College for offered in recognize Urban Men only(M) the College d by the (U) For Women Up to UGC only(W) Bachelor under Co-education Degree Section (CE) (UG) 2(f)&12B Up to Master Degree (PG) Or above 1. 2. 3. 4. 5. 6. 7. 8. 9. 1 Pune Deccan Education Society’s U 1885 MW UG, PG B.A., B.A-Music., B.Sc., Fergusson College, B.Sc.-Computer Science, (Arts, Science) B.Sc-Bio-technology Deccan, Pune – 411 004. B.Sc-Environmental Ph.No.020-25654212/ Science, 25675960 B.Sc- Microbiology, E.Mail: [email protected] Vocational Electronic (ID.NO.PU/PN/AS/02/1885) Equipment maintenance, Vocational Still Photography and Audiovisual, Vocational Biotechnolgy M.A-English, Marathi, Economics,Psychology, M.Sc- Org Chemistry, Analytical Chemistry, Bio-Chemistry, M.Sc.Tec.Ind.Maths, C:\DOCUME~1\PC1\LOCALS~1\Temp\List on Website.docx Microbiology, Physics, Petrolium Technology, Electronics Science, Environmental science, Geology, Bio-tech, Botany, Zoology M.Sc- Computer Science MCA-(Science), 2 Pune Shikshan Prasarak Mandal’s U 1916 MW UG, PG B.A., B.Com.,B.B.A., Sir Parashurambhau College B.Sc.-Computer Science, (Arts,Science and Commerce), MA.- Economics, Politics, Tilak Road, Pune-411030. Geography, Psychology, Ph. No. 020- 24331978, Philosophy, Logic Fax No. -

The Pune District Central Co-Operative Bank Ltd
THE PUNE DISTRICT CENTRAL CO-OPERATIVE BANK LTD. INFORMATION TECHNOLOGY DEPARTMENT HEAD OFFICE: Pune District Central Co-op. Bank Ltd., B 4, B. J. Road, Pune. Pin – 411001 REQUEST FOR PROPOSAL (RFP) FOR Appointment of Network Management Service Provider and Branch Network Equipment Provider REF NO. : PDCC/IT-Tender/2018-19/002 RELEASE DATE: 03-09-2018 PARTICULARS DEADLINE Last Date of Submission of RFP related pre bid query 10/09/2018, 16:00 hours Pre-bid Meeting 11/09/2018, 13:00 hours Last date of submission of the Technical and Commercial bid 25/09/2018, 15:00 hours Date of opening of the Technical bid 25/09/2018, 16:00 hours Bank email id for RFP related communication [email protected] 1 TABLE OF CONTENT 1. OBJECTIVE ................................................................................................................................................................................. 4 2. PROJECT STRUCTURE ........................................................................................................................................................... 4 3. IMPLEMENTATION SCHEDULE ........................................................................................................................................ 4 4. ELEGIBILITY CRITERIA ........................................................................................................................................................ 5 5. SCOPE OF WORK .................................................................................................................................................................... -

Sr No Retailer Name Retailer Address Area Mobile City State Pincode
Sr No Retailer Name Retailer Address Area Mobile City State Pincode SR NO 44ROOM NO 237 ADHARSH 1 MAULI PAN SHOP (36180) Adarsh Nagar - Pune Maharashtra 411061 NAGAR PUNE MAHARASHTRA 411061- SURVEY NO 230B121 NEW AIRPORT 2 NIRMALA VISHNU RAUT Airport Road 7798543178 Pune Maharashtra 411032 ROADMADINA MAJID SANJAY PARK PUNE house no 860 ghundare ali chavdi chouk 3 VISHVARAJ ENTERPRISES (34779) vadgoan rd alandi alandi alandi alandi Alandi - Pune Maharashtra 412105 pune MAHARASHTRA 4121- 570 SAIBABA MANDEERAMBEDKAR 4 MO ANWAR RAIS AHMAD ANSARI Ambedkar Nagar 9921272116 Pune Maharashtra 411037 NAGAR Shravan Kumar Triyogi Singh (Pune)- FLAT NO 1 B GANESH APARTMENT 5 Ambegaon 9175698807 Pune Maharashtra 411037 IBP AMBEGAON PA- SHANKAR PARVATI APPT BHUYARI MARG 6 GANRAJ MOBILE SHOPPE (35430) JAVAL DATTANAGAR AMBEGOAN PUNE Ambegoan - Pune Maharashtra 411060 MAHARASTRA- FLAT NO 9 KUDALE PATIL TOWERS 7 BHUMKAR ROHAN DILIP SINHGROAD NR FUN TIME TALKIES Anand Nagar 8421539599 Pune Maharashtra 411051 ANAND NAGAR CHANDRAMA RESIDENCEY A WING FLAT 8 GANDHI GANESH SHANTILAL NOSUN CITY ROAD ANANDNAGAR Anand Nagar 9850549597 Pune Maharashtra 411051 SINHGAD RO PLOT NO 19, SAISHREE MAHALXMI SICIETY LANE NO 3, SINHAGAD ROAD, 9 SAIKRUPA ENTERPRISES (38075) Anand Nagar - Pune Maharashtra 411051 OPP SANTOSH HALL, ANAND NAGAR PUNE- SHOP NO 27 S NO 20 21 AJANTAPALACE 10 LAXMIKANT JIVRAJ VORA Balaji Nagar 9890170750 Pune Maharashtra 411043 BEHIND ELLORA PALACE BALAJI NAGAR OPP KK MARKET PUNE 11 KMK MOBILE (37436) Balaji Nagar - Pune Maharashtra 411043 MAHARASHTRA