Research Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pdf/DM13/DM13.Pdf
FOREWORD n both the past and present, and in virtually every allow a better understanding of the sector and thus pave I world region, widely varied religious actors play the way for an exploration of priorities and for crucial roles in health care. Nowhere is this more meaningful action. significant than in Sub-Saharan Africa. Today, in most African countries, faith institutions and groups run Frankly, the report found more solid information than clinics, hospitals, and facilities that support families, expected. However, much is in silos, inaccessible or orphans, handicapped people, the mentally ill, and older unknown to key actors. And it is patchy with notable people. In communities, leaders and individuals gaps. It also confirmed our rising appreciation for communicate vital messages about health and provide remarkably wide differences country to country and sustained, hands-on care for the sick. The devastating faith tradition to faith tradition. Thus, a key element is a HIV and AIDS pandemic has placed a powerful series of short, preliminary case studies of faith health spotlight on these networks and their impact. With care in five countries— Gabon, Ghana, Mozambique, ambitious contemporary global health goals—notably South Sudan, and Tanzania—that illustrate this combatting malaria, tuberculosis, and maternal deaths, diversity. but also making decent care for all a meaningful human The report’s principle author was Lynn Aylward, who right—faith leaders and communities can be vital allies. led a team of contributors comprised of Molly Brady Yet many international health institutions and some and Kari Nelson. The case studies were written by Lynn governments have paid scant attention to faith-inspired Aylward, Katherine Marshall, and Claudia Zambra, organizations (FIOs) and their potential impact has not with research and writing assistance by Elizabeth Bliss been tapped in any systematic fashion. -

Histoire, Societe, Poesie
ANNALES DE L’UNIVERSITE OMAR BONGO, N° 19 1 HISTOIRE, SOCIETE, POESIE DES DESEQUILIBRES AUX EQUILIBRES Annales de l’U.O.B., n° 19 ; Décembre 2014 ISSN : 2-912603-18-8 ; ISBN : 978-2-912603-52-4 ; EAN : 978-2-912603-52-4 © Presses Universitaires du Gabon ANNALES DE L’UNIVERSITE OMAR BONGO, N° 19 DECEMBRE 2014 DIRECTEUR DE PUBLICATION : MARC LOUIS ROPIVIA, RECTEUR DE L'UOB DIRECTEUR SCIENTIFIQUE : PATRICK DAOUDA MOUGUIAMA COMITE SCIENTIFIQUE : COMITES DE LECTURE : SCIENCES HUMAINES : JEAN-AIME BOUSSOUGOU LETTRES ET LANGUES : GUY SERGE BIGNOUMBA ALEXANDRE BARRO CHAMBRIER JEAN-AIME BOUSSOUGOU DANIEL AKENDENGUE JEAN-JACQUES EKOMIE JULES DJEKI BERNARD EKOME OSSOUMA 2 JEROME KWENZI-MIKALA THIERRY EKOGHA FREDERIC MAMBENGA YLAGOU RAYMOND MAYER MANON LEVESQUE EP. KOMBILA BLANDINE MOUENDOU CHARLES MBA OWONO THEODORE KOUMBA NICOLAS NGOU MVE JEAN-EMILE MBOT MICHEL LOKO STEEVE ROBERT RENOMBO NICOLAS METEGUE N'NAH ROGER MICKALA PIERRE TCHALOU JOHN JOSEPH NAMBO BERNARDIN MINKO MVE ANDRE TOLOFON HERVÉ NDOUME ESSINGONE PLACIDE MOWANGUE PIERRE NDOMBI JEAN BERNARD MOMBO FIDELE PIERRE NZE NGUEMA JEAN-FRANÇOIS OWAYE NOËL MESMIN SOUMAHO JOSEPH TONDA GILBERT ZUE NGUEMA ISSN : 2-912603-18-8 ISBN : 978-2-912603-52-4 EAN : 9782912603524 © Presses Universitaires du Gabon B.P. 13.131, Libreville Gabon www.pug-uob.org Annales de l’U.O.B., n° 19 ; Décembre 2014 ISSN : 2-912603-18-8 ; ISBN : 978-2-912603-52-4 ; EAN : 978-2-912603-52-4 © Presses Universitaires du Gabon HISTOIRE, SOCIETE, POESIE DES DESEQUILIBRES AUX EQUILIBRES SOMMAIRE SAVOIRS ET SOCIETE HISTOIRE GRANDE-BRETAGNE/AFRIQUE -

Acp-Eu Joint Parliamentary Assembly
ACP-EU JOINT PARLIAMENTARY ASSEMBLY NOTICE TO MEMBERS Members will find attached the follow-up given by the Commission to the resolutions adopted by the ACP-EU Joint Parliamentary Assembly during its 4th session of 18 - 21 March 2002 in Cape Town (South Africa). The Co-secretariat DV\493765EN.doc APP/3499 EN EUROPEAN COMMISSION ACP-EU JOINT PARLIAMENTARY ASSEMBLY BRAZZAVILLE (Republic of the Congo) 31 March – 3 April 2003 Members of the ACP-EU Joint Parliamentary Assembly will find attached progress reports on the follow-up action the Commission has taken or planned in response to the main points and certain specific requests contained in the resolutions adopted by the ACP-EU Joint Parliamentary Assembly during its session held in Cape Town (South Africa) from 18–21 March 2002. The Commission is at the disposal of the parliamentarians for any further information they may require. DV\493765EN.doc2 APP/3499 FOLLOW UP OF THE EUROPEAN COMMISSION TO THE RESOLUTIONS OF THE ACP-EU JOINT PARLIAMENTARY ASSEMBLY ADOPTED IN CAPE TOWN (SOUTH AFRICA) ON 21 MARCH 2002 Page - on the situation in West Africa (ACP-EU 3383/02/fin.) 4 - on the situation in Central Africa and the African Great Lakes region 6 (ACP-EU 3384/02/fin.) - on the situation in Southern Africa (ACP-EU 3385/02/fin.) 7 - on the situation in Madagascar (ACP-EU 3386/02/fin.) 10 - on the situation in Zimbabwe (ACP-EU 3396/02/fin.) 11 - on the situation in East Africa (ACP-EU 3387/02/fin.) 13 - on the Caribbean region (ACP-EU 3388/02/fin.) 14 - on the situation in Cuba (ACP-EU 3389/02/fin.) -
A THEORETICAL MODEL for a YIPUNU-ENGLISH-FRENCH EXPLANATORY DICTIONARY of MEDICAL TERMS Guy-Roger MIHINDOU: Doctoral Dissertation
A THEORETICAL MODEL FOR A YIPUNU-ENGLISH-FRENCH EXPLANATORY DICTIONARY OF MEDICAL TERMS Guy-Roger MIHINDOU Dissertation presented for the Degree of Doctor of Literature (Lexicography) at the University of Stellenbosch Promoter: Prof. R.H. GOUWS April 2006 DECLARATION I, the undersigned, hereby declare that the work contained in this dissertation is my own original work and had not previously in its entirety or in part been submitted at any other university for a degree. ............................................................ .................................................... Signature Date A THEORETICAL MODEL FOR A YIPUNU-ENGLISH-FRENCH EXPLANATORY DICTIONARY OF MEDICAL TERMS Guy-Roger MIHINDOU: Doctoral dissertation DEDICATION Tata Kondi- Mihindou, Yilumbu I ma rugha Diweru di matola mu vhegha yirondu na yisungu ombu fumu MUGHURI, dub du kiri. Ghirighanu, Kala asa mafu na mbagha, mutu tsinga asa mafu na mitanguni. I dedicate this work to my late father KONDI-MIHIDOU DANIEL (MUGHURI), as I say Diboti di neni tata, mu malongi motsu, la yiraa! mwana yaloolu. This Dedication is also for you MWA DIGHABI-DI- MUNDUNGA, my grand mother. For you taught me that duya mulong tsambi omulong, uvhiol mutsi mulund mutsi. vii ACKNOWLEDGEMENT I would like to express my deepest gratitude to my promoter Prof. R.H. Gouws for his diligent guidance, gentleness, his ability to encourage for excellence. From him I got the conviction that accuracy and completion pave the way to excellence. To my wife, Piekielele “Piks” Mihindou, my sincerest appreciation, for the unshakable faith in the completion of this work, the unreserved support, the help and encouragements I received from her, when facing the utmost uncertainties. I whish to thank my mother, Kondi Augustine, my uncle Nzigou Ditengou Dan, as well as my brothers, Ndzia-Saji, Fabrice, Jordan, and my sister Soulejka “Copine”, for their emotional support and prayers. -

Brief on Public Health and Social Measure Implementation in Africa
Brief on Public Health and Social Measure Implementation in Africa 14-27 July 2020 Note: This report includes information on how COVID-19 has affected health care workers across Africa and how public mistrust of governments and international agencies is affecting PHSM adherence and fueling vaccine hesitancy. Table of Contents I. Africa COVID-19 Situation • Metrics • Key Trends • Disease Dynamics • PHSM Implementation & Adherence • PHSM Burden II. Spotlight • Health Care Worker Burden • Vaccine Hesitancy III. Regional Analysis • Central Africa • Eastern Africa • Northern Africa • Southern Africa • Western Africa IV. Annex • Aims and Approach • Methods and Limitations • Epidemiological Indicators • Data Sources • Reporting Rates • Resources Africa COVID-19 Situation: Metrics 7-day moving average of mobility No. of health care workers Total cases/ Total deaths/ Countries with positive test Region change between 15 Feb - 27 July2 tested positive/ Trend 13-27 July Trend 13-27 July rate1 >10% > +10% or < -10% % of total cases3 Central African Rep (15%) Central Chad (13%) 45,504 896 Congo (15%) Gabon (-16%) 1,050 (2.6%) Africa DRC (20%) Sao Tome & Principe (30%) Comoros (22%) Kenya (-20%) Madagascar (25%) Eastern Mauritius (-16%) Somalia (17%) 67,718 1,555 Rwanda (-14%) 712 (1.6%) Africa S. Sudan (19%) Uganda (-29%) Sudan (34%) Algeria (29%) Northern Morocco (-12%) Egypt (21%) 149,264 6,330 Egypt (-24%) 2,826 (1.9%) Africa Mauritania (10%) Angola (-24%) Southern South Africa (16%) Mozambique(-13%) 463,999 7,146 5,386 (1.4%) Africa Malawi (13%) South Africa (-31%) Zimbabwe (-18%) Cameroon (12%) Cote d’Ivoire (18%) Burkina Faso (+12%) Western Equatorial Guinea (12%) Cabo Verde (-38%) 120,594 1,849 Gabon (10%) Nigeria (-17%) 4,687 (4.3%) Africa Guinea (14%) Senegal (-14%) Guinea Bissau (19%) Togo (-14%) Nigeria (15%) 1. -

World Bank Document
Public Disclosure Authorized GABON ASSESSMENT OF THE IMPACT OF Public Disclosure Authorized TOBACCO EXCISE TAX INCREASES ON PRICE, CONSUMPTION AND TAX REVENUE OVER 2018-2021 Public Disclosure Authorized D [Document subtitle] WORLD BANK GROUP April 25, 2019 Public Disclosure Authorized Table of Contents Executive Summary ........................................................................................................................ 3 Impact Assessment of New Tobacco Taxation in Gabon ................................................................ 4 Modelling Tobacco Tax Impact Assessment for 2018-2021 in Gabon ....................................... 4 Results ......................................................................................................................................... 5 Conclusions and recommendations ............................................................................................ 8 I. Introduction ........................................................................................................................... 10 II. Modelling the fiscal revenue impact of tobacco tax increases in Gabon ........................... 11 A. Current cigarette market – Retail Price and Consumption Trends ................................. 11 B. Gabon Tobacco Taxation ............................................................................................... 13 C. Assessing tobacco tax increases impact on consumption and tax revenue in Gabon .... 17 III. Conclusion and Policy Recommendations........................................................................ -
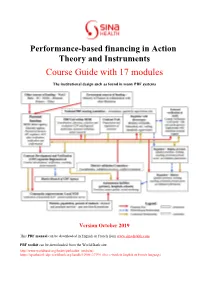
Course Guide with 17 Modules
Performance-based financing in Action Theory and Instruments Course Guide with 17 modules The institutional design such as found in many PBF systems Version October 2019 This PBF manual can be downloaded in English or French from www.sina-health.com PBF toolkit can be downloaded from the World Bank site: http://www.worldbank.org/health/pbftoolkit (website) https://openknowledge.worldbank.org/handle/10986 /17194 (free e-book in English or French language) PBF Course Manual Page 2 PBF in Action Theory and Instruments PBF Course Guide The components of the PBF black box SINA – 2019 PBF Course Manual Page 3 Ninth edition, 2019 Guide, Performance-based financing, health, health financing The contents of this publication can be reproduced if the source SINA is duly mentioned. Using this book for conducting courses is allowed when coordinated with Robert Soeters from SINA Health to assure that the latest materiel and methodologies are being used and in general to assure the quality of the course. Main Editor: Robert Soeters, PhD - SINA Health Contributors: Freddy BATUNDI, Dr. Michel BOSSUYT, Dr. Harmelle ENAME, Moussoume EKOUANGUE, Bwanga ENANDJOUM, Dr. Gyuri FRITSCHE, Christian HABINEZA, Frank van de LOOIJ Jean Baptiste HABIGUHIRWA, Sosthène HICUBURUNDI, Célestin KIMANUKA, Dr. Philémon MBESSAN, Professeur MUNYANGA, Pacifique MUSHAGULUSA, Dr Juvénal NDAYISHIMIYE, Dr Canut NKUNZIMANA, Dr Claude NTABUYANTWA, Dr Jean Paul NYARUSHATSI, Didier NTIRORANYA, Dr Peter Bob PEERENBOOM, Ernest Schoffelen, Dr Jean Pierre TSAFACK, René QUEFFELEC, Dr. Godelieve -

Preventive Measures Against the Vectors of Malaria in Akanda, Southwest Gabon: Knowledge, Attitudes, Practices, and Beliefs
ESJ Natural/Life/Medical Sciences Preventive Measures Against The Vectors Of Malaria In Akanda, Southwest Gabon: Knowledge, Attitudes, Practices, And Beliefs Richard Pamba, Silas Lendzele Sevidzem, Ecole Doctorale des Grandes Ecole de Libreville (EDGE), Libreville, Gabon Laboratoire d’Ecologie Vectorielle (LEV), Institut de Recherche en Ecologie Tropicale (IRET), Centre National de la Recherche Scientifique et Technologique, Libreville, Gabon Aubin Armel Koumba, Laboratoire d’Ecologie Vectorielle (LEV), Institut de Recherche en Ecologie Tropicale (IRET), Centre National de la Recherche Scientifique et Technologique, Libreville, Gabon Faculté des Sciences et Techniques (FAST), Université d’Abomey-Calavi, Cotonou, Bénin Christophe Roland Zinga-Koumba, Audrey Prisca Melodie Ovono, Rodrigue Mintsa-Nguema, Jacques François Mavoungou, Laboratoire d’Ecologie Vectorielle (LEV), Institut de Recherche en Ecologie Tropicale (IRET), Centre National de la Recherche Scientifique et Technologique, Libreville, Gabon Alexis Mbouloungou, Laboratoire de Géomatique, de Recherche Appliquée et de Conseil (LAGRAC), Université Omar Bongo (UOB), Faculté des Lettres et Sciences Humaines (FLSH), Libreville, Gabon Felicien M’Foubou Kassa, Institut d’Hygiène Publique et Assainissement, Ministère de la Santé, Libreville, Gabon Pyazzi Obame Ondo Kutomy, Programme National de Lutte contre le Paludisme, Ministère de la santé, Libreville, Gabon Doi:10.19044/esj.2021.v17n21p169 Submitted: 05 August 2020 Copyright 2021 Author(s) Accepted: 27 May 2021 Under Creative Commons BY-NC-ND Published: 30 June 2021 4.0 OPEN ACCESS www.eujournal.org 169 European Scientific Journal, ESJ ISSN: 1857-7881 (Print) e - ISSN 1857-7431 June 2021 edition Vol.17, No.21 Cite As: Pamba R., Sevidzem S.L., Koumba A.A., Zinga-Koumba C.R., Ovono A.P.M., Mintsa- Nguema R., Mavoungou J.F., Mbouloungou A., M’Foubou Kassa F. -

The State of Health in the Who African Region African Who the in Health of State The
THE STATE OF HEALTH IN THE WHO AFRICAN REGION THE STATE OF HEALTH in the WHO African Region An analysis of the status of health, health services and health systems in the context of the Sustainable Development Goals Where we are Where we need to go on no e b g e in h v i n a d d e e L L i n A AFRIC SUSTAINABLE DEVELOPMENT G ALS 30 30 25 6% 6% 25 20 20 8% 7% 4% 2% 15 15 4% 6% 2% 10 14% 14% 3% 2% 10 11% 3% 9% 5 8% 5 6% 0 0 Courts Police Public Public clinic/ school service hospital Once or twice A few times Often The peoples of Africa aspire to a future of good health and well-being. The health and health-related Sustainable Development Goals (SDGs) build on this hope, providing guidance to ensure that no one is left behind as the continent progresses towards sustainable and equitable health. To achieve this, a coherent and logical approach to the adaptation of the SDGs is needed, to ensure that the health dividend accrued in the coming years is enjoyed equitably and plays its role in accelerating the development of the continent. The WHO Regional Oce for Africa has set up a process to ensure that countries walk together as they march towards sustainable and equitable health. This report is a recognition of the complexity of actions needed. It aims to provide guidance on where countries need to focus as they plan their work towards attaining the SDGs. -

Underestimation of Hepatocellular Carcinoma Incidence Resulting from a Competition Between Modern and Traditional Medicine: the Case of Gabon
Moussavou-Boundzanga P, Mabika B, Itoudi Bignoumba PE, et al. Underestimation of hepatocellular carcinoma incidence resulting from a competition between modern and traditional medicine: the case of Gabon. Journal of Global Health Reports. 2020;4:e2020063. doi:10.29392/001c.13653 Viewpoint Underestimation of hepatocellular carcinoma incidence resulting from a competition between modern and traditional medicine: the case of Gabon Pamela Moussavou-Boundzanga 1 , Barthelemy Mabika 2, Patrice E Itoudi Bignoumba 3, Agnès Marchio 4, Augustin Mouinga-Ondeme 5, JP Moussavou Kombila 3, Pascal Pineau 4 1 Laboratoire de Biologie Moléculaire et Cellulaire (LABMC), Université des Sciences et Techniques de Masuku, Franceville, Gabon; Unité Infections Rétrovirales et Pathologies Associées, Centre International de Recherches Médicales de Franceville, Franceville, Gabon, 2 Département d'Anatomie Pathologique , Faculté de Médecine, Université Sciences de la Santé, Libreville, Gabon, 3 Service d'Hepato-Gastroentérologie, Centre Hospitalier Universitaire de Libreville, Gabon, 4 Unité Organisation nucléaire et oncogenèse, INSERM U993, Institut Pasteur, France, 5 Unité Infections Rétrovirales et Pathologies Associées, Centre International de Recherches Médicales de Franceville, BP769, Franceville, Gabon Keywords: epidemiology, incidence, primary liver cancer, gabon https://doi.org/10.29392/001c.13653 Journal of Global Health Reports Vol. 4, 2020 Primary liver cancer, particularly hepatocellular carcinoma (HCC), remains a major killer in sub-Saharan Africa. In this dreadful landscape, West and Central Africas are more particularly affected. However, a small country located on the equator, Gabon, is apparently not concerned by this adverse situation. Despite worrying prevalences of many bona fide risk factors of HCC, including high rates of chronic infections with hepatitis viruses and very high alcohol consumption, Gabon presents theoretically an amazingly low incidence of HCC when compared to other countries of the region. -
Effective Project Planning and Evaluation in Biomedical Research
Couv_OK Step:Step Guide cover 13.4.2007 10:03 Page 2 TRAINERS TDR/RCS/PPE/T/07.2 Effective project planning and evaluation in biomedical research STEP-BY-STEP GUIDE Special Programme for Research & Training TDR/World Health Organization 20, Avenue Appia in Tropical Diseases (TDR) sponsored by 1211 Geneva 27 UNICEF/UNDP/World Bank/WHO Switzerland Fax: (+41) 22 791-4854 [email protected] www.who.int/tdr The Special Programme for Research and Training in Tropical Diseases (TDR) is a global programme of scientific collaboration established in 1975. Its focus is research into neglected diseases of the poor, with the goal of improving existing approaches and developing new ways to prevent, diagnose, treat and control these diseases. TDR is sponsored Special Programme for Research & Training by the following organizations: in Tropical Diseases (TDR) sponsored by UNICEF/UNDP/World Bank/WHO World Bank Couv_OK Step:Step Guide cover 5.4.2007 19:13 Page 4 2pages_debut_SBS:7522_OMS_STEP_BY_STEP 5.4.2007 19:16 Page 1 TDR/RCS/PPE/T/07.2 Effective project planning and evaluation in biomedical research STEP-BY-STEP GUIDE TRAINERS Special Programme for Research & Training in Tropical Diseases (TDR) sponsored by UNICEF/UNDP/World Bank/WHO 2pages_debut_SBS:7522_OMS_STEP_BY_STEP 5.4.2007 19:16 Page 2 TDR/RCS/PPE/T/07.2 Copyright © World Health Organization on behalf of the Special Programme for Research and Training in Tropical Diseases 2007 All rights reserved. The use of content from this health information product for all non-commercial education, training and information purposes is encouraged, including translation, quotation and reproduction, in any medium, but the content must not be changed and full acknowledgement of the source must be clearly stated. -

Safety and Efficacy of the RTS,S/AS01E Candidate Malaria
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Digital Library of the Tanzania Health Community Articles Safety and effi cacy of the RTS,S/AS01E candidate malaria vaccine given with expanded-programme-on-immunisation vaccines: 19 month follow-up of a randomised, open-label, phase 2 trial Kwaku Poku Asante, Salim Abdulla, Selidji Agnandji, John Lyimo, Johan Vekemans, Solange Soulanoudjingar, Ruth Owusu, Mwanajaa Shomari, Amanda Leach, Erik Jongert, Nahya Salim, Jose F Fernandes, David Dosoo, Maria Chikawe, Saadou Issifou, Kingsley Osei-Kwakye, Marc Lievens, Maria Paricek, Tina Möller, Stephen Apanga, Grace Mwangoka, Marie-Claude Dubois, Tigani Madi, Evans Kwara, Rose Minja, Aurore B Hounkpatin, Owusu Boahen, Kingsley Kayan, George Adjei, Daniel Chandramohan, Terrell Carter, Preeti Vansadia, Marla Sillman, Barbara Savarese, Christian Loucq, Didier Lapierre, Brian Greenwood, Joe Cohen, Peter Kremsner, Seth Owusu-Agyei, Marcel Tanner, Bertrand Lell Summary Background The RTS,S/AS01E candidate malaria vaccine is being developed for immunisation of infants in Africa Lancet Infect Dis 2011; through the expanded programme on immunisation (EPI). 8 month follow-up data have been reported for safety and 11: 741–49 Published Online immunogenicity of RTS,S/AS01E when integrated into the EPI. We report extended follow-up to 19 months, including effi cacy results. July 21, 2011 DOI:10.1016/S1473- 3099(11)70100-1 Methods We did a randomised, open-label, phase 2 trial of safety and effi cacy of the RTS,S/AS01E candidate malaria This online publication vaccine given with EPI vaccines between April 30, 2007, and Oct 7, 2009, in Ghana, Tanzania, and Gabon.