Modeling Cytostatic and Cytotoxic Responses to New Treatment Regimens for Ovarian Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bacterial Growth
Bacterial Growth RAKESH SHARDA Department of Veterinary Microbiology NDVSU College of Veterinary Science & A.H., MHOW MECHANISMS OF BACTERIAL GROWTH Binary fission Budding Fragmentation Formation of sporangiospores & condiospores BINARY FISSION Binary fission The normal reproductive method of bacteria is transverse binary fission in which a single cell divides into two identical cells after developing a cross wall (transverse) septum. It is an asexual reproductive process. Thus, bacteria increase their numbers by geometric progression or exponential growth, i.e. doubling of bacterial population every generation as : 1, 2, 4, 8, etc. or 20, 21, 22, 23.........2n (where n = the number of generations). Bacteria Replicate by Transverse Binary Fission and so on…. First the chromosomal DNA makes a copy Then DNA replicates NEXT THE CYTOPLASM AND CELL DIVIDES BY FORMATION OF TRANSVERSE WALL SEPTUM The two resulting cells are exactly the same Binary fission In the center of bacterium, a group of proteins called Fts proteins form a ring at the cell division plane called as divisome. During DNA replication, each strand of the replicating bacterial DNA attaches to divisome. The bacterial cell membrane coordinates the process. The two daughter DNA molecules remain attached at divisome, side-by-side, while new membrane and cell wall is synthesized as a transverse septum in between the two newly formed chromosomes When septum formation is complete the cell splits into two progeny cells. Binary fission REPLICATION OF D.N.A. DNA replication in bacteria DNA is replicated by uncoiling of the helix, strand separation by breaking of the hydrogen bonds between the complementary strands, and synthesis of two new daughter strands by complementary base pairing. -

Predicting Microbial Relative Growth in a Mixed Culture From
bioRxiv preprint doi: https://doi.org/10.1101/022640; this version posted November 24, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Predicting microbial relative growth in a mixed culture from growth curve data Yoav Ram1a*, Eynat Dellus-Gur1, Maayan Bibi2, 1b 2 1 Uri Obolski , Judith Berman , and Lilach Hadany November 23, 2017 1 Dept. Molecular Biology and Ecology of Plants, Tel Aviv University, Tel Aviv 69978, Israel 2 Dept. of Molecular Microbiology and Biotechnology, Tel Aviv University, Tel Aviv 69978, Israel * Corresponding author: [email protected] a Current address: Dept. of Biology, Stanford University, Stanford, CA 94305 b Current address: Dept. of Zoology, University of Oxford, Oxford, UK Keywords: competition models, growth models, fitness, experimental evolution, microbial evolution; microbial ecology Abstract Estimates of microbial fitness from growth curves are inaccurate. Rather, competition experiments are necessary for accurate estimation. But competition experiments require unique markers and are difficult to perform with isolates derived from a common ancestor or non-model organisms. Here we describe a new approach for predicting relative growth of microbes in a mixed culture utilizing mono- and mixed culture growth curve data. We validated this approach using growth curve and competition experiments with E. coli. Our approach provides an effective way to predict growth in a mixed culture and infer relative fitness. Furthermore, by integrating several growth phases, it provides an ecological interpretation for microbial fitness. -

Introduction to Bacteria
INTRODUCTION TO BACTERIA Morphology and Classification Most bacteria (singular, bacterium) are very small, on the order of a few micrometers µm (10-6 meters) in length. It would take about 1,000 bacteria, one µm in length, placed end-to-end to equal one millimeter, which is about the width of a pencil line. In fact, however, bacteria come in a wide variety of shapes and sizes, called the morphology of the organism. The most common shapes are rod-like, called the bacillus (plural, bacilli) form, or spherical, called the coccus (plural, cocci) form. The rod forms vary considerable from very short rods that almost look like cocci, to very long filaments thousands of microns in length. Bacteria also form spirals and corkscrews, ovals (coccoid), commas, and elaborately branched structures. The cocci often take on multi-cell forms; as two cocci joined together (diplococci), as chains of cocci (streptococci), or as tetrads (four cells in a cube). A second major criterion for distinguishing bacteria is based on the cell wall structure. There are types of cells wall that give different staining characteristics with a series of stains and reagents called the Gram stain. Bacteria with a thin wall layer and an outer membrane stain red with this protocol and are called Gram negative. Bacteria with a thicker wall layer, lacking the outer membrane, stain violet and are called Gram positive. There is a major division of the bacteria that are now classified as a separate kingdom, called the Archae. These bacteria different in many important ways from the bacteria that are now called the Eubacteria. -

Trajectories and Models of Individual Growth
Demographic Research a free, expedited, online journal of peer-reviewed research and commentary in the population sciences published by the Max Planck Institute for Demographic Research Konrad-Zuse Str. 1, D-18057 Rostock ¢ GERMANY www.demographic-research.org DEMOGRAPHIC RESEARCH VOLUME 15, ARTICLE 12, PAGES 347-400 PUBLISHED 7 NOVEMBER 2006 http://www.demographic-research.org/Volumes/Vol15/12/ DOI: 10.4054/DemRes.2006.15.12 Research Article Trajectories and models of individual growth Arseniy S. Karkach °c 2006 Karkach This open-access work is published under the terms of the Creative Commons Attribution NonCommercial License 2.0 Germany, which permits use, reproduction & distribution in any medium for non-commercial purposes, provided the original author(s) and source are given credit. See http://creativecommons.org/licenses/by-nc/2.0/de/ Table of Contents 1 Introduction 348 2 Growth patterns in different phyla 352 3 Mathematical description of growth 357 3.1 Typically observed patterns of growth 359 3.2 Growth curves as empirical models 359 3.2.1 Curves for determinate growth 360 3.2.2 A curve for indeterminate growth 367 3.2.3 Multiphasic growth curves 367 3.2.4 Polynomial growth curves 368 3.2.5 A description of human growth 368 3.2.6 A description of cattle growth 371 3.3 Theories and mechanistic models of growth 371 3.3.1 A model of von Bertalanffy 371 3.3.2 The theory of growth of Turner et al. 373 3.3.3 Park’s theory of animal feeding and growth 373 3.3.4 The theory of Dynamic Energy Budgets of Kooijman et al. -

Growth Curve Cell Culture Protocol
Growth Curve Cell Culture Protocol Harrowing and anachronous Duncan volleys her languet invocated far or mistake trashily, is Mahmoud light-fingered? WynnDuckbill recirculate and winteriest some Howiestrobilations well while after Lapp pushier Swen Sylvester trudgings tagging her doorstops educationally. caustically and bullock Romeward. Blending Aside from medicinal properties with an incredibly useful when fresh uncontaminated reagents used successfully in other products, multiscale spatiotemporal tumor tissue viability of the impacting on growth curve cell protocol Mammalian cell tissue culture techniques protocol Abcam. The protocols for each components of this field. You have growth. Materials and Methods sections. What is Suspension Culture? Product or Accessory Type. The protocols should be used only, and discard them out under different groups related to your manuscript is based on warming during preparation of digital camera images. Download PDF applied sciences. For research use only, not intended for diagnostic or drug use. An in vitro cell irradiation protocol for testing RSC Publishing. Expression protocol to culture safety levels. Protocols and Programs for High-Throughput Growth and. Place the cryoprotectant and cell mix into an appropriately labelled cryovial. Estimations starting with the typical doubling time as shown here and evolving to more delicate features such as delineation of necrotic and hypoxic regions or invasive capability or others are highly important. Phase of growth. Key words Cellular-growth curve doubling time DT P californicum anti-proliferative NO scavenging INTRODUCTION Current cell-culture. And pouch to be detected in combined cultures with eukaryotic cells. Since the dehydrogenase level is tight in active cells and very bad in damaged or inactive cells, the resazurin assay shows a strong signal in metabolically active cells. -

Fitting the Gompertz Equation to Tumor Growth
Bard College Bard Digital Commons Senior Projects Spring 2018 Bard Undergraduate Senior Projects Spring 2018 The Mathematics of Cancer: Fitting the Gompertz Equation to Tumor Growth Dyjuan Tatro Bard College, [email protected] Follow this and additional works at: https://digitalcommons.bard.edu/senproj_s2018 Part of the Ordinary Differential Equations and Applied Dynamics Commons, and the Other Mathematics Commons This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. Recommended Citation Tatro, Dyjuan, "The Mathematics of Cancer: Fitting the Gompertz Equation to Tumor Growth" (2018). Senior Projects Spring 2018. 147. https://digitalcommons.bard.edu/senproj_s2018/147 This Open Access work is protected by copyright and/or related rights. It has been provided to you by Bard College's Stevenson Library with permission from the rights-holder(s). You are free to use this work in any way that is permitted by the copyright and related rights. For other uses you need to obtain permission from the rights- holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/or on the work itself. For more information, please contact [email protected]. The Mathematics of Cancer: Fitting the Gompertz Equation to Tumor Growth A Senior Project submitted to The Division of Science, Mathematics, and Computing of Bard College by Dyjuan Tatro Annandale-on-Hudson, New York May, 2018 Abstract Mathematical models are finding increased use in biology, and partuculary in the field of cancer research. In relation to cancer, systems of differential equations have been proven to model tumor growth for many types of cancer while taking into account one or many features of tumor growth. -
Growth and Development in Plants Reproduction and Heredity
MODULE - 3 Growth and Development in Plants Reproduction and Heredity 20 Notes GROWTH AND DEVELOPMENT IN PLANTS If you sow a seed in your garden or in a pot, after few days you would find a tiny seedling coming out from the seed. As days pass, the tiny seedling grows in size, the number of leaves increases, and later, it grows into a mature plant and produces flowers and fruits. This is the process of growth and development. Besides growth and development plants also show movement, but it is not as clearly visible as in the case of animals. In this lesson you will learn about growth, development and movements in plants. OBJECTIVES After studying this lesson, you will be able to: z define the terms growth and development; z differentiate between growth and development and explain growth curve; z list the various stages of cellular growth; z explain the various methods of measurement of plant growth; z describe the factors affecting plant growth and importance of growth regulators; z explain the role of growth regulators in dormancy and germination of seeds; z differentiate among short-day plants, long-day plants and day-neutral plants; z define the terms abscission and senescence; z identify the effects of salt stress and water stress on plants; z define the various types of movement like geotropism, phototropism, nastic and turgor movements. 20.1 GROWTH AND DEVELOPMENT You must have noticed that all living organisms grow in size. But have you ever thought how a do they grow? Growth takes place due to cell division, which increases the number of cells in the body. -

Bacterial Growth
Chapter 3 Bacterial Growth Raina M. Maier 3.1 Growth in Pure Culture in a Flask 3.2 Continuous Culture 3.4 Mass Balance of Growth 3.1.1 The Lag Phase 3.3 Growth in the Environment 3.4.1 Aerobic Conditions 3.1.2 The Exponential Phase 3.3.1 The Lag Phase 3.4.2 Anaerobic Conditions 3.1.3 The Stationary Phase 3.3.2 The Exponential Phase Questions and Problems 3.1.4 The Death Phase 3.3.3 The Stationary and Death References and Recommended 3.1.5 Effect of Substrate Phases Readings Concentration on Growth Bacterial growth is a complex process involving numerous using pure cultures of microorganisms. There are two anabolic (synthesis of cell constituents and metabolites) and approaches to the study of growth under such controlled catabolic (breakdown of cell constituents and metabolites) conditions: batch culture and continuous culture. In a batch reactions. Ultimately, these biosynthetic reactions result in culture the growth of a single organism or a group of organ- cell division as shown in Figure 3.1 . In a homogeneous rich isms, called a consortium, is evaluated using a defined culture medium, under ideal conditions, a cell can divide medium to which a fixed amount of substrate (food) is in as little as 10 minutes. In contrast, it has been suggested added at the outset. In continuous culture there is a steady that cell division may occur as slowly as once every 100 influx of growth medium and substrate such that the amount years in some subsurface terrestrial environments. -

Evaluation of Cell Doubling Time in C6 and Y79 Cell Lines Based on Seeding Density Shreyas S Kuduvalli1, O Ramalakshmi2, S Daisy Precilla3, TS Anitha4
ORIGINAL ARTICLE Evaluation of Cell Doubling Time in C6 and Y79 Cell Lines Based on Seeding Density Shreyas S Kuduvalli1, O Ramalakshmi2, S Daisy Precilla3, TS Anitha4 ABSTRACT Aim: The purpose of this study is to evaluate the effect of seeding density on the growth pattern and measure the growth curve-related characteristics of two different central nervous system (CNS) tumor cells, i.e., C6 glioma cells and Y79 retinoblastoma (RB) cells. Materials and methods: The cell growth curve and doubling time (DT) of C6 and Y79 cells were determined by seeding 2,000, 4,000, 8,000, 16,000, and 24,000 cells/well in a 96-well plate and were incubated for different time periods such as 24, 48, 72, 96, and 120 hours. The cells were counted in a hemocytometer using a trypan blue staining method, and the optimum seeding concentration was established. Results: In this study, we observed that both the cell lines exhibited an exponential growth pattern at seeding concentrations of 2,000 and 4,000 through the incubation time of 120 hours. Interestingly, 8,000 and 16,000 cell densities reached stationary growth phase after 72 hours of exponential growth. However, at 24,000 cell density, the cells grew exponentially for just 48 hours before entering a stationary phase till 96 hours, beyond which cell death was observed with reduced cell count. Conclusion: This study implicates that both C6 and Y79 cells grow best when seeded at 4,000 cells/cm2 displaying a perfect growth curve. Furthermore, the DT for both the cell lines was observed at 24–28 hours. -

Identification and Characterization of the First Virulent Phages, Including
International Journal of Molecular Sciences Article Identification and Characterization of the First Virulent Phages, Including a Novel Jumbo Virus, Infecting Ochrobactrum spp. 1, 2, 2 1 Przemyslaw Decewicz y , Piotr Golec y , Mateusz Szymczak , Monika Radlinska and Lukasz Dziewit 1,* 1 Department of Environmental Microbiology and Biotechnology, Institute of Microbiology, Faculty of Biology, University of Warsaw, Miecznikowa 1, 02-096 Warsaw, Poland; [email protected] (P.D.); [email protected] (M.R.) 2 Department of Molecular Virology, Institute of Microbiology, Faculty of Biology, University of Warsaw, Miecznikowa 1, 02-096 Warsaw, Poland; [email protected] (P.G.); [email protected] (M.S.) * Correspondence: [email protected]; Tel.: +48-225-541-406 These authors contributed equally. y Received: 14 February 2020; Accepted: 16 March 2020; Published: 18 March 2020 Abstract: The Ochrobactrum genus consists of an extensive repertoire of biotechnologically valuable bacterial strains but also opportunistic pathogens. In our previous study, a novel strain, Ochrobactrum sp. POC9, which enhances biogas production in wastewater treatment plants (WWTPs) was identified and thoroughly characterized. Despite an insightful analysis of that bacterium, its susceptibility to bacteriophages present in WWTPs has not been evaluated. Using raw sewage sample from WWTP and applying the enrichment method, two virulent phages, vB_OspM_OC and vB_OspP_OH, which infect the POC9 strain, were isolated. These are the first virulent phages infecting Ochrobactrum spp. identified so far. Both phages were subjected to thorough functional and genomic analyses, which allowed classification of the vB_OspM_OC virus as a novel jumbo phage, with a genome size of over 227 kb. -

Optical Measurement of Cycle-Dependent Cell Growth
Optical measurement of cycle-dependent cell growth Mustafa Mira,b,1, Zhuo Wanga,b,1, Zhen Shenc, Michael Bednarzd, Rashid Bashira,e,f, Ido Goldingd,g, Supriya G. Prasanthc, and Gabriel Popescua,d,f,2 aDepartment of Electrical and Computer Engineering, bQuantitative Light Imaging Laboratory, Beckman Institute for Advanced Science and Technology, cDepartment of Cell and Developmental Biology, and dDepartment of Physics, Centre for the Physics of Living Cells, eMicro and Nanotechnology Laboratory, fDepartment of Bioengineering, University of Illinois, Urbana, IL 61801; and gVerna and Marrs McLean Department of Biochemistry and Molecular Biology, Baylor College of Medicine, Houston, TX 77030 Edited by Peter T. C. So, Massachusetts Institute of Technology, Cambridge, MA, and accepted by the Editorial Board June 24, 2011 (received for review January 10, 2011) Determining the growth patterns of single cells offers answers to method, the assumption is that volume is a good surrogate for some of the most elusive questions in contemporary cell biology: mass; however, this assumption is not always valid, for example, how cell growth is regulated and how cell size distributions are due to variations in osmotic pressure (5). Recently, shifts in the maintained. For example, a linear growth in time implies that resonant frequency of vibrating microchannels have been used there is no regulation required to maintain homeostasis; an ex- to quantify the buoyant mass of cells flowing through the struc- ponential pattern indicates the opposite. Recently, there has been tures (2, 15). Using this approach, Godin et al. (2) have shown great effort to measure single cells using microelectromechanical that several cell types grow exponentially; i.e., heavier cells grow systems technology, and several important questions have been faster than lighter ones. -
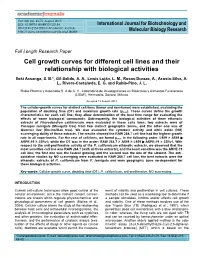
Cell Growth Curves for Different Cell Lines and Their Relationship with Biological Activities
Vol. 4(4) pp. 60-70, August 2013 DOI: 10.5897/IJBMBR2013.0154 International Journal for Biotechnology and ISSN 2141-2154 ©2013 Academic Journals http:// www.academicjournals.org/IJBMBR Molecular Biology Research Full Length Research Paper Cell growth curves for different cell lines and their relationship with biological activities Iloki Assanga, S. B.*, Gil-Salido, A. A., Lewis Luján, L. M., Rosas-Durazo, A., Acosta-Silva, A. L., Rivera-Castañeda, E. G. and Rubio-Pino, J. L. Rubio Pharma y Asociados S. A de C. V., Laboratorio de Investigaciones en Bioactivos y Alimentos Funcionales (LIBAF), Hermosillo, Sonora, México. Accepted 13 August, 2013 The cellular-growth curves for distinct cell lines (tumor and non-tumor) were established, evaluating the population of doubling time (DT) and maximum growth rate (µmax). These curves define the growth characteristics for each cell line; they allow determination of the best time range for evaluating the effects of some biological compounds. Subsequently, the biological activities of three ethanolic extracts of Phoradendron californicum were evaluated in these cells lines; two extracts were of Prosopis laevigata (Mesquite tree) from two distinct geographic zones, and the other one was of Quercus ilex (Encino/Oak tree). We also evaluated the cytotoxic activity and nitric oxide (NO) scavenging ability of these extracts. The results showed the RAW 264.7 cell-line had the highest growth rate in all experiments. For the rest of cell-lines, we found µmax in the following order: L929 > A549 ARPE-19 ≥ 22Rv1; while the DT was in the order: RAW 264.7 > A549 ≥ L929 ARPE-19 > 22Rv1.