Affordability & Value of Health Care Focus of MAHP 2017-2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protect Your Collective Bargaining Rights!
PROTECT YOUR COLLECTIVE BARGAINING RIGHTS! On April 26th, a majority of the members of the Massachusetts of House Representatives voted to dramatically restrict the rights of municipal employees to collectively bargain over the issue of health insurance. It is critically important that you let your Representative know how you feel about their vote. These Representatives voted IN FAVOR of your collective bargaining rights: Democrats: Geraldo Alicea Denise Andrews Bruce Ayers Michael Brady Paul Brodeur Thomas Calter Christine Canavan James Cantwell Tackey Chan Nicholas Collins Edward Coppinger Geraldine Creedon Mark Cusack Marcos Devers James Dwyer Lori Ehrlich Christopher Fallon Robert Fennell John Fresolo Denise Garlick Coleen Garry John Mahoney Paul Mark James Miceli Kevin Murphy Rhonda Nyman James O’Day Thomas Petrolati Denise Provost Kathi-Anne Reinstein Carl Sciortino Joyce Spiliotis Thomas Stanley David Sullivan Walter Timilty Timothy Toomey Cleon Turner Marty Walsh Steven Walsh Alice Wolf Republicans: Bradford Hill Daniel Winslow If your state representative stood up for you, it is important that you call them and thank them for their support. You can say something like this: My name is ____________________ and I live in __________________. I work for the city/town of ___________ as a _____________. I am calling because Rep. ____________ voted in favor of maintaining collective bargaining rights for municipal workers like me. I wanted to thank Rep. ______________ for standing up for my union rights. These Representatives voted AGAINST -

An Act to Provide Identification to Homeless Youth and Families
________________________________________________________________________________________________ Everyone Needs ID: An Act to Provide Identification to Homeless Youth and Families Senate Bill 2043 and House Bill 3066 Sponsored by Senator Harriette Chandler and Representative Kay Khan Lead Sponsors: Senator Harriette Chandler and Representative Kay Khan Senate Cosponsors: Senators Will Brownsberger, Jo Comerford, Julian Cyr, Sal DiDomenico, Jamie Eldridge, Cindy Friedman, Pat Jehlen, Jason Lewis, Mike Moore, and Becca Rausch House Cosponsors: Representatives Ruth Balser, Natalie Blais, Daniel Carey, Mike Connolly, Dan Donahue, Marjorie Decker, Mindy Domb, Carolyn Dykema, Nika Elugardo, Tricia Farley-Bouvier, Sean Garballey, Carmine Gentile, Carlos González, Tami Gouveia, James Hawkins, Kevin Honan, Mary Keefe, David LeBoeuf, Jack Patrick Lewis, David Linsky, Adrian Madaro, Liz Malia, Paul Mark, Paul McMurtry, Liz Miranda, Jim O’Day, Elizabeth Poirier, Denise Provost, Dave Rogers, Lindsay Sabadosa, Jon Santiago, Tom Stanley, José Tosado, Steve Ultino, Aaron Vega, and Bud Williams Bill History: Both Senate Bill 2043 and House Bill 3066 were refiled in January 2019, and were reported out favorably by the Joint Committee on Transportation in November 2019. S. 2043 was sent to the Senate Committee on Ways and Means, and may come up for a vote by the full Senate soon. H. 3066 was sent to the Joint Committee on Health Care Financing, and is awaiting action. Last session, the bill (Senate Bill 2568) passed the Senate unanimously. Importance of -
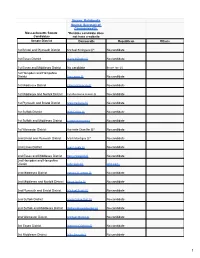
MA CCAN 2020 Program FINAL
Source: Ballotpedia Source: Secretary of Commonwealth Massachusetts Senate *Denotes candidate does Candidates not have a website Senate District Democratic Republican Others 1st Bristol and Plymouth District Michael Rodrigues (i)* No candidate 1st Essex District Diana DiZoglio (i) No candidate 1st Essex and Middlesex District No candidate Bruce Tarr (i) 1st Hampden and Hampshire District Eric Lesser (i) No candidate 1st Middlesex District Edward Kennedy (i) No candidate 1st Middlesex and Norfolk District Cynthia Stone Creem (i) No candidate 1st Plymouth and Bristol District Marc Pacheco (i) No candidate 1st Suffolk District Nick Collins (i) No candidate 1st Suffolk and Middlesex District Joseph Boncore (i) No candidate 1st Worcester District Harriette Chandler (i)* No candidate 2nd Bristol and Plymouth District Mark Montigny (i)* No candidate 2nd Essex District Joan Lovely (i) No candidate 2nd Essex and Middlesex District Barry Finegold (i) No candidate 2nd Hampden and Hampshire District John Velis (i) John Cain 2nd Middlesex District Patricia D. Jehlen (i) No candidate 2nd Middlesex and Norfolk District Karen Spilka (i) No candidate 2nd Plymouth and Bristol District Michael Brady (i) No candidate 2nd Suffolk District Sonia Chang-Diaz (i) No candidate 2nd Suffolk and Middlesex District William Brownsberger (i) No candidate 2nd Worcester District Michael Moore (i) No candidate 3rd Essex District Brendan Crighton (i) No candidate 3rd Middlesex District Mike Barrett (i) No candidate 1 Source: Ballotpedia Source: Secretary of Commonwealth -

March 25, 2020 the Honorable Charles Baker State House, Rm
March 25, 2020 The Honorable Charles Baker State House, Rm 360 Boston, MA 02133 Secretary MaryLou Sudders Executive Office of Health and Human Services 1 Ashburton Place, 11th Floor Boston, MA 02108 Dear Governor Baker and Madam Secretary, We write to channel the urgency that members spoke of on the Legislature’s call with you yesterday, March 24, regarding the systemic response necessary to address the needs and rights of people who are currently without homes. You know well that for this population, the public health recommendation to “stay at home” is not possible, nor will it be possible for an entire shelter population to self-quarantine once a guest is discovered to be COVID-19 positive or for that individual to self-isolate. As you also know very well, this is a very vulnerable community and the sector responsible for serving this community is tireless, though entirely under resourced. We want to underscore that our municipalities are also not capable of adding one more acute need to their long list of concerns. Respectfully, we join together to urge the Commonwealth to immediately identify and dedicate the resources for expanded or alternative shelter structures (by county) that reduce density for this population to address its needs holistically. We are grateful for your commitment to this population and we urge you to act quickly on our shared goals: • Direct local emergency response personnel to consider this effort as part of the Emergency Order. • Identify and assess the necessary infrastructure (e.g. hotel rooms, motel rooms, college and boarding school dormitories, etc.) and/or produce new construction that may be needed (for e.g. -

Candidate Full Name Candidate City Office Sought Office Held Alex Bezanson Abington House, 7Th Plymouth N/A, No Office Alyson M
Candidate Full Name Candidate City Office Sought Office Held Alex Bezanson Abington House, 7th Plymouth N/A, No office Alyson M. Sullivan Abington House, 7th Plymouth House, 7th Plymouth Kristen Gail Arute Accord House, 3rd Plymouth N/A, No office Benjamin Elliot Bloomenthal Acton House, 14th Middlesex N/A, No office Daniel L. Factor Acton House, 14th Middlesex N/A, No office Tami L. Gouveia Acton House, 14th Middlesex House, 14th Middlesex James Eldridge Acton Senate, Middlesex & Worcester Senate, Middlesex & Worcester Susan R. Dawson Agawam Senate, Hampden N/A, No office Forrest W. Bradford Agawam House, 3rd Hampden N/A, No office William P. Sapelli Agawam Mayoral, Agawam Mayoral, Agawam Brian P. Golden Allston House, 18th Suffolk N/A, No office James M. Kelcourse Amesbury House, 1st Essex House, 1st Essex Brianna R. Sullivan Amesbury House, 1st Essex N/A, No office Thatcher W. Kezer III Amesbury Mayoral, Amesbury N/A, No office Robert W. Lavoie Amesbury House, 1st Essex N/A, No office C. Kenneth Gray Amesbury Mayoral, Amesbury Mayoral, Amesbury Anne R. Ferguson Amesbury Mayoral, Amesbury N/A, No office Alexander L. Williams Amesbury Senate, 1st Essex N/A, No office Jennifer Rocco-Runnion Amesbury House, 1st Essex N/A, No office Theodore T. Semesnyei Amesbury Mayoral, Amesbury N/A, No office James N. Thivierge Amesbury Mayoral, Amesbury N/A, No office Kassandra M. Gove Amesbury Mayoral, Amesbury N/A, No office Matthew Burton Amesbury House, 1st Essex N/A, No office David J. Murphy Amherst Senate, Hampshire, Franklin & Worcester N/A, No office Mindy Domb Amherst House, 3rd Hampshire House, 3rd Hampshire Stanley C. -

Letter-To-President-Re-International
students contribute a $41 billion economic impact that supports more than 450,000 jobs. As one of our University Presidents observed, no public good is served by these efforts to deprive international students from continuing to make valuable and necessary contributions to the prosperity of the nation and the impact on the economic interests will be negative and potentially irreversible. This policy is not only punitive to these international students, it also threatens the safety of other students and the communities surrounding college campuses. Additionally, transporting international students who may have been exposed to the coronavirus to other campuses or to airports to fly back to their home countries poses a myriad of health risks. Finally, we understand that both Harvard University and MIT filed suit seeking a preliminary injunction this morning and I am sure others will follow. This litigation will be costly, will take time, and will waste precious judicial resources at a time when we should be focusing on rebuilding our nation. Accordingly, we request that, in the best interest of our nation, you reconsider and rescind the temporary rules to help preserve our higher education system which is, indeed, the envy of the world. Most respectfully, Robert A. DeLeo Jeffrey N. Roy Speaker of the House House Chair Committee on Higher Education Anne Gobi Claire Cronin Senate Chair House Chair Committee on Higher Education Committee on Judiciary Paul McMurtry Patricia A. Haddad House Chair Speaker Pro Tempore Committee on Tourism, Arts and Cultural Development Bradley H. Jones, Jr. Alice H. Peisch House Minority Leader House Chair 20th Middlesex District Committee on Education Joanne M. -

MASC Legislative Directory 2020
2020 Massachusetts State Legislative Directory Massachusetts Constitutional Officers Governor Charlie Baker (617) 725-4005 Room 280 Lt. Governor Karyn Polito (617) 725-4005 Room 360 Treasurer Deborah Goldberg (617) 367-6900 Room 227 Atty. General Maura Healey (617) 727-2200 1 Ashburton Place, 18th Floor [email protected] Sec. of the State William Galvin (617) 727-9180 Room 340 [email protected] State Auditor Suzanne Bump (617) 727-2075 Room 230 [email protected] Massachusetts Senate (617) 722- Email (@masenate.gov) Room # (617) 722- Email (@masenate.gov) Room # Michael Barrett 1572 Mike.Barrett 109-D Patricia Jehlen 1578 Patricia.Jehlen 424 Joseph Boncore 1634 Joseph.Boncore 112 John Keenan 1494 John.Keenan 413-F Michael Brady 1200 Michael.Brady 416-A Edward Kennedy 1630 Edward.Kennedy 70 William Brownsberger 1280 William.Brownsberger 319 Eric Lesser 1291 Eric.Lesser 410 Harriette Chandler 1544 Harriette.Chandler 333 Jason Lewis 1206 Jason.Lewis 511-B Sonia Chang-Diaz 1673 Sonia.Chang-Diaz 111 Joan Lovely 1410 Joan.Lovely 413-A Nick Collins 1150 Nick.Collins 312-D Mark Montigny 1440 Mark.Montigny 312-C Joanne Comerford 1532 Jo.Comerford 413-C Michael Moore 1485 Michael.Moore 109-B Cynthia Creem 1639 Cynthia.Creem 312-A Patrick O'Connor 1646 Patrick.OConnor 419 Brendan Crighton 1350 Brendan.Crighton 520 Marc Pacheco 1551 Marc.Pacheco 312-B Julian Cyr 1570 Julian.Cyr 309 Rebecca Rausch 1555 Becca.Rausch 218 Sal DiDomenico 1650 Sal.DiDomenico 208 Michael Rodrigues 1114 Michael.Rodrigues 212 Diana DiZoglio 1604 Diana.DiZoglio 416-B -

S643/H2480) Lead Sponsors: Senators Lewis, Chandler & Welch, Representatives Vega & Chan
AN ACT TO PROMOTE PUBLIC HEALTH THROUGH THE PREVENTION & WELLNESS TRUST FUND (S643/H2480) Lead Sponsors: Senators Lewis, Chandler & Welch, Representatives Vega & Chan REPRESENTATIVES Dylan Fernandes Juana Matias SENATORS Brian Ashe Sean Garballey Joseph McKenna Michael Barrett Cory Atkins Denise Garlick Joan Meschino Michael Brady Bruce Ayers Carmine Gentile James Miceli William Brownsberger Ruth Balser Susan Gifford Rady Mom Harriette Chandler Christine Barber Solomon Goldstein-Rose David Muradian Sonia Chang-Diaz Jennifer Benson Carlos Gonzalez Matt Muratore Julian Cyr Donald Berthiaume Danielle Gregoire James Murphy Sal DiDomenic Antonio Cabral Stephan Hay Brian Murray James Eldridge Daniel Cahill Jonathan Hecht David Nangle Jennifer Flanagan Thomas Calter Paul Heroux Shaunna O'Connell Vinny deMacedo Kate Campanale Natalie Higgins James O'Day Linda Dorcena Forry James Cantwell Kate Hogan Sarah Peake Anne Gobi Gailanne Cariddi Russell Holmes Smitty Pignatelli Adam Hinds Evandro Carvalho Kevin Honan Denise Provost Donald Humason Gerard Cassidy Daniel Hunt Angelo Puppolo John Keenan Tackey Chan Hannah Kane David Rogers Eric Lesser Nick Collins Louis Kafka Byron Rushing Jason Lewis Mike Connolly Mary Keefe Daniel Ryan Barbara L'Italien Brendan Crighton Kay Khan Paul Schmid Joan Lovely Will Crocker Peter Kocot Frank Smizik Thomas McGee Claire Cronin Robert Koczera Todd Smola Michael Moore Daniel Cullinane Stephen Kulik William Straus Patrick O'Connor Mark Cusack John Lawn Jose Tosado James Welch Josh Cutler Jack Lewis Steven Ultrino Marjorie Decker David Linsky Aaron Vega REPRESENTATIVES = 93 David DeCoste Jay Livingstone David Vieira SENATORS = 23 Daniel Donahue Adrian Madaro Joseph Wagner TOTAL = 116 Michelle Dubois John Mahoney Chris Walsh Carolyn Dykema Elizabeth Malia Bud Williams Lori Ehrlich Paul Mark Tricia Farley-Bouvier Christopher Markey 1. -

Senate House Massachusetts House of Representatives
Senate House Massachusetts House of Representatives Representative Dylan Fernandes, (Barnstable, Dukes & Nantucket) Phone: (617) 722-2013 Email: [email protected] Cities: Nantucket, Falmouth, Chilmark, Aquinnah, Gosnold, Oak Bluffs, Tisbury, West Tisbury Representative Timothy Whelan, (1st Barnstable) Phone: (617) 722-2488 Email: [email protected] Cities: Dennis, Brewster, Yarmouth Representative Kip Diggs, (2nd Barnstable) Phone: (617) 722-2800 Email: [email protected] Cities: Barnstable, Yarmouth Representative David Vieira, (3rd Barnstable) Phone: (617) 722-2230 Email: [email protected] Cities: Teaticket (Falmouth), Bourne, Mashpee Representative Sarah Peake, (4th Barnstable) Phone: (617) 722-2040 Email:[email protected] Cities Provincetown, Chatham, Eastham, Harwich, Orleans, Truro, Wellfleet Representative Steven Xiarhos, (5th Barnstable) Phone: (617) 722-2800 Email: [email protected] Cities Sandwich, Barnstable, Bourne, Plymouth Representative John Barrett, (1st Berkshire) Phone: (617) 722-2305 Email: [email protected] North Adams, Adams, Clarksburg, Florida, Williamstown, Chesire, Hancock, Lanesborough, New Ashford Representative Paul Mark, (2nd Berkshire) Phone: (617) 722-2304 Email: [email protected] Bernardston, Colrain, Dalton, Hinsdale, Leyden, Northfield, Peru, Pittsfield, Savoy, Windsor, Greenfield, Charlemont, Hawley, Heath, Monroe, Rowe Representative Tricia Farley-Bouvier, (3rd Berkshire) -

Msp Membership Meeting
MSP MEMBERSHIP MEETING April 8, 2021 AGENDA • Welcome and ground rules – Marc – 12:00 – 12:05 • UMass financial situation – Marc – 12:05 – 12:25 • MSP bargaining platform – Asha – 12:25 – 12:35 • What can we do? – Eve – 12:35 – 12:40 • MTA updates – Max – 12:40 – 12:45 • Q&A – MSP Executive Committee – 12:45 – 1:00 • Post-meeting – MSP bargaining team and members – 1:00 – 1:30 GROUND RULES • This meeting is for MSP members only. • Please do not record or photograph the meeting in any way. • Please stay on mute so that everyone can hear. • Please type questions or comments into the Chat box – be patient because we have a lot of information to share and we’ll get to your questions. • This PowerPoint will be posted on the MSP website: umassmsp.org • If you have questions about your individual situation, please email them directly to [email protected]. All queries to the union are confidential. WHERE’S THE MONEY? MSP BARGAINING PRINCIPLES: COVID-RELATED ISSUES • Make SRTI optional (administration unilaterally decided to require SRTI this semester) • Automatic extensions of TDY delays with retroactive pay – with the option to revert to one’s original TDY • Workload adjustment for faculty and librarians whose work increased due to Covid-19 health and safety protocols to accommodate in-person student instruction and services • Accommodations for faculty and librarians with Covid-related health concerns in the fall MSP BARGAINING PRINCIPLES: RACE AND GENDER EQUITY • Recruit faculty and librarians from underrepresented groups through multiple pathway hires; • Equitable workload processes for departments, libraries, and clinical; • Holistic evaluations of teaching rather than relying on SRTI scores; • Reduce gender and race inequities at the time of hiring by having candidates meet with MSP both pre-hire and upon separation. -
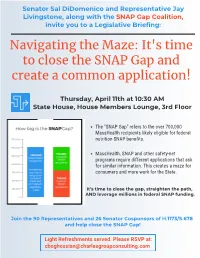
It's Time to Close the SNAP Gap and Create a Common Application!
Senator Sal DiDomenico and Representative Jay Livingstone, along ith the SNAP Gap Coalition, invite you to a Legislative Briefing: Navigating the Maze: It's time to close the SNAP Gap and create a common application! Thursday, April th at : AM State House, House Members Lounge, rd Floor The "SNAP Gap" refers to the over 700,000 MassHealth recipients likely eligible for federal nutrition SNAP benefits. MassHealth, SNAP and other safety-net programs require different applications that ask for similar information. This creates a maze for consumers and more work for the State. It’s time to close the gap, straighten the path, AND leverage millions in federal SNAP funding. Join the Representatives and Senator Cosponsors of H./S. and help close the SNAP Gap! Light Refreshments served. Please RSVP at: [email protected] SNAP Gap Cosponsors H./S. Representatives & Senators* Senator Michael Barrett Representative Gerard Cassidy Representative David Linsky Senator Joseph Boncore Representative Michelle Ciccolo Representative Adrian Madaro Senator William Brownsberger Representative Mike Connolly Representative John Mahoney Senator Harriette Chandler Representative Edward Coppinger Representative Elizabeth Malia Senator Sonia Chang-Diaz Representative Daniel Cullinane Representative Paul Mark Senator Jo Comerford Representative Michael Day Representative Joseph McGonagle Senator Nick Collins Representative Marjorie Decker Representative Paul McMurtry Senator Brendan Crighton Representative David DeCoste Representative Christina -

Day on the Hill 2014 “Advocacy: Beacon Hill and Beyond”
Day on the Hill 2014 “Advocacy: Beacon Hill and Beyond” March 26, 2014 Massachusetts State House, Boston 9:30 am – noon "The League of Women Voters is the gold standard in advocacy. I tell my staff that when they see the League's name among the supporters of something, pay attention." --Nancy Pelosi, former Speaker, now minority leader, U.S. House of Representatives Representative Pelosi commented on the significance of League advocacy when she met LWVMA board member Marlene O’Brien at the Radcliffe Institute’s celebration of the 50th anniversary of the first report on the Presidential Commission on the Status of Women. Table of Contents Co-Presidents’ Message .............................................................................................................................. 1 Day on Hill Speakers .................................................................................................................................... 2 Legislative Action Committee ..................................................................................................................... 3 Why Lobby on March 26 at Day on the Hill ................................................................................................ 4 Tips on How to Lobby Your Legislators ....................................................................................................... 5 Talking Points for Featured Bills ................................................................................................................ 6 Education ............................................................................................................................................