020 Medicare Advantage Part B Step Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2019 Aetna Pharmacy Drug Guide Aetna Premier Plus Plan
Plan for your best health 2019 Aetna Pharmacy Drug Guide Aetna Premier Plus Plan aetna.com 05.02.414.1 O (12/19) Aetna is the brand name used for products and services provided by one or more of the Aetna group of subsidiary companies, including Aetna Life Insurance Company and its affiliates (Aetna). Aetna Pharmacy Management refers to an internal business unit of Aetna Health Management, LLC. Aetna Pharmacy Management administers, but does not offer, insure or otherwise underwrite the prescription drug benefits portion of your health plan and has no financial responsibility therefor. 2019 Aetna Commercial Plan (Premier Plus) Table of Contents INFORMATIONAL SECTION..................................................................................................................7 *5-HT4 RECEPTOR AGONISTS*** - DRUGS FOR THE STOMACH................................................ 18 *ADHD/ANTI-NARCOLEPSY/ANTI-OBESITY/ANOREXIANTS* - DRUGS FOR THE NERVOUS SYSTEM.................................................................................................................................18 *AGENTS FOR NARCOTIC WITHDRAWAL*** - DRUGS FOR ADDICTION............................... 22 *AGENTS FOR OPIOID WITHDRAWAL*** - DRUGS FOR ADDICTION......................................22 *AMEBICIDES* - DRUGS FOR INFECTIONS.....................................................................................22 *AMINO ACIDS*** - DRUGS FOR NUTRITION................................................................................ 22 *AMINOGLYCOSIDES* - DRUGS FOR -

Ophthalmologic Policy: Vascular Endothelial Growth Factor (VEGF) Inhibitors
UnitedHealthcare® Community Plan Medical Benefit Drug Policy Ophthalmologic Policy: Vascular Endothelial Growth Factor (VEGF) Inhibitors Policy Number: CS2021D0042S Effective Date: March 1, 2021 Instructions for Use Table of Contents Page Related Community Plan Policies Application.......................................................................................... 1 • Macular Degeneration Treatment Procedures Coverage Rationale ........................................................................... 1 • Maximum Dosage and Frequency Definitions ........................................................................................... 3 • Oncology Medication Clinical Coverage Applicable Codes .............................................................................. 3 Background ........................................................................................ 3 Commercial Policy Clinical Evidence .............................................................................23 • Ophthalmologic Policy: Vascular Endothelial Growth U.S. Food and Drug Administration ..............................................34 Factor (VEGF) Inhibitors Centers for Medicare and Medicaid Services .............................35 References .......................................................................................35 Policy History/Revision Information..............................................39 Instructions for Use .........................................................................39 Application This Medical Benefit -

Imaging Tumor Angiogenesis
Imaging tumor angiogenesis Kristy Red-Horse, Napoleone Ferrara J Clin Invest. 2006;116(10):2585-2587. https://doi.org/10.1172/JCI30058. Commentary Since the discovery of vascular-specific growth factors with angiogenic activity, there has been a significant effort to develop cancer drugs that restrict tumorigenesis by targeting the blood supply. In this issue of the JCI, Mancuso et al. use mouse models to better understand the plasticity of the tumor vasculature in the face of antiangiogenic therapy (see the related article beginning on page 2610). They describe a rapid regrowth of the tumor vasculature following withdrawal of VEGFR inhibitors, emphasizing the importance of fully understanding the function of these and similar treatments used in the clinic at the cellular and molecular level. Find the latest version: https://jci.me/30058/pdf commentaries Imaging tumor angiogenesis Kristy Red-Horse and Napoleone Ferrara Genentech Inc., South San Francisco, California, USA. Since the discovery of vascular-specific growth factors with angiogenic activ- in 1 week (Figure 1). In accordance with ity, there has been a significant effort to develop cancer drugs that restrict previous findings (4, 6), posttreatment tumorigenesis by targeting the blood supply. In this issue of the JCI, Mancuso angiogenic growth correlated with the et al. use mouse models to better understand the plasticity of the tumor vas- disappearance of empty basement mem- culature in the face of antiangiogenic therapy (see the related article begin- brane sleeves, suggesting that regrowth ning on page 2610). They describe a rapid regrowth of the tumor vasculature occurred along these structures (Figure 1). -

Med Pharm PA List to Build Pdfs.Xlsx
The following medications, typically administered in a provider's office or ambulatory/outpatient infusion center, require authorization prior to utilization. Authorization requests can be submitted via the Portal. Additionally, you are welcome to call our member services line to initiate the Prior Authorization process. This list is updated quaterly. Effective date: 1/1/2021 Therapeutic category Brand Name Generic Name HCPCS Immunologic agent Orencia, IV infusion abatacept J0129 Botulinum toxins Dysport abobotulinumtoxin B J0586 HER-2 receptor drug Kadcyla ado-trastuzumab emtansine J9354 Ophthalmic injectable Eylea afilbercept J0178 Enzyme replacement drug Fabrazyme agalsidase beta J0180 Multiple sclerosis drug Lemtrada alemtuzumab J0202 Enzyme replacement drug Lumizyme alglucosidase alfa J0221 Enzyme replacement drug Strensiq asfotase alfa J3590 (non-specific) PD1-PDL1 drug Tecentriq atezolizumab J9022 PD1-PDL1 drug Bavencio avelumab J9023 CAR-T Therapy Yescarta axicabtageneciloleucel inpatient admin Systemic lupus erythematosus (SLE) drug Benlysta belimumab J0490 Antineoplastic agent Beleodaq belinostat J9032 Antineoplastic Belrapzo bendamustine HCl J9036 Antineoplastic Bendeka bendamustine HCl J9034 Antineoplastic agent Treanda bendamustine HCl J9033 Respiratory injectable Fasenra benralizumab J0517 J9035/J3590 (ophthalmology Antineoplastic Avastin bevacizumab uses this non-specific code) Antineoplastic agent Mvasi bevacizumab-awwb Q5107 Antineoplastic agent Zirabev bevacizumab-bvzr Q5118 Antineoplastic agent Blincyto blinatumomab -

Pegaptanib (Macugen) Reference Number: CP.PHAR.185 Effective Date: 03/16 Coding Implications Last Review Date: 03/17 Revision Log
Clinical Policy: Pegaptanib (Macugen) Reference Number: CP.PHAR.185 Effective Date: 03/16 Coding Implications Last Review Date: 03/17 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description The intent of the criteria is to ensure that patients follow selection elements established by Centene® clinical policy for pegaptanib (Macugen®). Policy/Criteria It is the policy of health plans affiliated with Centene Corporation® that Macugen is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Macular Degeneration (must meet all): 1. Diagnosis of neovascular (wet) age-related macular degeneration (AMD); 2. Prescribed dose of Macugen does not exceed 0.3 mg (1 syringe) every six weeks; 3. Macugen will not be used concomitantly with other anti-vascular endothelial growth factor (VEGF) medications; 4. At the time of request, member has no ocular or periocular infections. Approval duration: 6 months B. Other diagnoses/indications: Refer to CP.PHAR.57 - Global Biopharm Policy. II. Continued Approval A. Macular Degeneration (must meet all): 1. Previously received medication via Centene benefit or member has previously met all initial approval criteria; 2. Documentation of positive response to therapy (e.g., detained neovascularization, improvement/stabilization of visual acuity, supportive findings on optical coherence tomography or fluorescein angiography); 3. Prescribed dose does not exceed 0.3 mg (1 syringe) every six weeks; 4. Macugen is not being used concomitantly with other anti-VEGF medications. Approval duration: 6 months B. Other diagnoses/indications (must meet 1 or 2): 1. Currently receiving medication via Centene benefit and documentation supports positive response to therapy; or 2. -
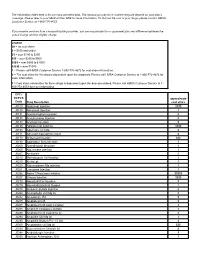
CPT / HCPCS Code Drug Description Approximate Cost Share
The information listed here is for our most prevalent plan. The amount you pay for a covered drug will depend on your plan’s coverage. Please refer to your Medical Plan GTB for more information. To find out the cost of your drugs, please contact HMSA Customer Service at 1-800-776-4672. If you receive services from a nonparticipating provider, you are responsible for a copayment plus any difference between the actual charge and the eligible charge. Legend $0 = no cost share $ = $100 and under $$ = over $100 to $250 $$$ = over $250 to $500 $$$$ = over $500 to $1000 $$$$$ = over $1000 1 = Please call HMSA Customer Service 1-800-776-4672 for cost share information. 2 = The cost share for this drug is dependent upon the diagnosis. Please call HMSA Customer Service at 1-800-772-4672 for more information. 3 = Cost share information for these drugs is dependent upon the dose prescribed. Please call HMSA Customer Service at 1- 800-772-4672 for more information. CPT / HCPCS approximate Code Drug Description cost share J0129 Abatacept Injection $$$$ J0130 Abciximab Injection 3 J0131 Acetaminophen Injection $ J0132 Acetylcysteine Injection $ J0133 Acyclovir Injection $ J0135 Adalimumab Injection $$$$ J0153 Adenosine Inj 1Mg $ J0171 Adrenalin Epinephrine Inject $ J0178 Aflibercept Injection $$$ J0180 Agalsidase Beta Injection 3 J0200 Alatrofloxacin Mesylate 3 J0205 Alglucerase Injection 3 J0207 Amifostine 3 J0210 Methyldopate Hcl Injection 3 J0215 Alefacept 3 J0220 Alglucosidase Alfa Injection 3 J0221 Lumizyme Injection 3 J0256 Alpha 1 Proteinase Inhibitor -
343 Intravitreal Angiogenesis Inhibitors for Choroidal Vascular
Medical Policy Intravitreal Angiogenesis Inhibitors for Choroidal Vascular Conditions Table of Contents • Policy: Commercial • Coding Information • Information Pertaining to All Policies • Policy: Medicare • Description • References • Authorization Information • Policy History Policy Number: 343 BCBSA Reference Number: 9.03.24A NCD/LCD: N/A Related Policies • Epiretinal Radiation Therapy for Age-Related Macular Degeneration, #610 • Photodynamic Therapy for Choroidal Neovascularization, #599 • Transpupillary Thermotherapy for Treatment of Choroidal Neovascularization, #600 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Medicare HMO BlueSM and Medicare PPO BlueSM Members Anti-vascular endothelial growth factor therapies (anti-VEGF), ie., pegaptanib (Macugen®*), ranibizumab (Lucentis™*), bevacizumab (Avastin™), and aflibercept (Eylea™*) for the treatment of neovascular (wet) age-related macular degeneration may be MEDICALLY NECESSARY. Anti-vascular endothelial growth factor therapies (anti-VEGF) are MEDICALLY NECESSARY for Choroidal neovascularization due to the following conditions: • Angioid streaks, • Central serous chorioretinopathy, • Choroidal rupture or trauma, • Idiopathic choroidal neovascularization, • Multifocal choroiditis, • Pathologic myopia, • Presumed ocular histoplasmosis syndrome, and • Uveitis. Anti-vascular endothelial growth factor therapies (anti-VEGF) are INVESTIGATIONAL for the treatment of chorioretinal scars. *FDA-approved indication 1 Prior Authorization Information Pre-service approval -

Pdf 111.82 K
INTERNATIONAL JOURNAL OF Int J Med Rev 2016;3(4):523-524 MEDICAL doi 10.15171/ijmr.2016.14 REVIEWS Letter to Editor The History and Efficacy of Intravitreal Injection of Pegaptanib in Patients With Macular Edema Secondary to Branch Retinal Vein Occlusion; The Need for Special Attention Roohollah Ahmadian1, Shahriar Najafizadeh-Sari1,2* 1Student Research Committee, Baqiyatallah University of Medical Science, Tehran, Iran 2Trauma Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran Corresponding Author: Shahriar Najafizadeh-Sari, MD, Student Research Committee, Baqiyatallah University of Medical Science, Tehran, Iran. Tel: +98-9126441288, Fax: +98-2188620826, Email: [email protected] Received December 2, 2016; Accepted December 20, 2016; Online Published December 24, 2016 e have read a recent article about intravitreal year.5 pharmacotherapy for the treatment of macular Pegaptanib is not FDA approved for BRVO yet. Anti-VEGF edema secondary to branch retinal vein drugs revolutionized the treatment of eyes suffering macular Wocclusion (BRVO) with great interest. You have mentioned edema secondary to BRVO, and this result necessitates the that few studies have evaluated the efficacy of pegaptanib further study of pegaptanib monotherapy or in combination in ocular diseases; thus, discussing this the Food and Drug with other effective agents. Administration (FDA)-approved drug is necessary. It would be useful to study more intensely RNA silencing Anti-VEGF therapy is a critical and potent approach for the (siRNA) with -

Picture As Pdfoctober 2020: Reminder Specific Medications
OCTOBER 2020: REMINDER SPECIFIC MEDICATIONS REQUIRE PRIOR AUTHORIZATION As a part of our continuous efforts to improve the quality of care for our members, Highmark Health Options wanted to send a reminder about the prior authorization process for the following medications. Failure to obtain authorization will result in a claim denial. The prior authorization process applies to all Highmark Health Options Members. Medical necessity criteria for each of the medications listed below are outlined in the specific medication policies available online. To access Highmark Health Options’ medical policies, please paste the following link in your internet browser: https://www.highmarkhealthoptions.com/providers/medication-information.html. PROCEDURE CODES REQUIRING AUTHORIZATION DRUG NAME CODE DESCRIPTION HCPCS DE Medicaid Injection, abatacept, 10 mg (code may be used for Medicare when drug administered under J0129 11/4/2019 the direct supervision of a physician, not for abatacept (Orencia) use when drug is self administered aflibercept (Eylea) Injection, aflibercept, 1 mg J0178 10/1/2018 agalsidase beta (Fabrazyme) Injection, agalsidase beta, 1 mg J0180 6/3/2019 alemtuzumab (Lemtrada) Injection, alemtuzumab, 1 mg J0202 11/4/2019 alglucosidase alfa (Lumizyme) Injection, alglucosidase alfa, (lumizyme), 10 mg J0221 10/1/2018 aprepitant (Cinvanti) Injection, aprepitant, 1 mg J0185 11/4/2019 asparaginase (Erwinaze) Injection, asparaginase (erwinaze), 1,000 iu J9019 11/4/2019 atezolizumab (Tecentriq) Injection, atezolizumab, 10 mg J9022 11/4/2019 Axicabtagene -

Age-Related Macular Degeneration (Amd)
EUnetHTA Joint Action 3 WP4 Relative effectiveness assessment of pharmaceutical technologies BROLUCIZUMAB FOR THE TREATMENT OF ADULTS WITH NEOVASCULAR (WET) AGE-RELATED MACULAR DEGENERATION (AMD) Project ID: PTJA09 Version 1.0, 12/03/2020 Dec2015 ©EUnetHTA, 2015. Reproduction is authorised provided EUnetHTA is explicitly acknowledged 1 PTJA09 - Brolucizumab for patients with neovascular (wet) AMD DOCUMENT HISTORY AND CONTRIBUTORS Version Date Description V0.1 28/01/2020 First draft V0.2 24/2/2020 Input from dedicated reviewers has been processed V0.3 10/03/2020 Input from medical editor and manufacturer(s) has been processed V1.0 12/03/2020 Final assessment report Disclaimer This Joint Assessment is part of the project / joint action ‘724130 / EUnetHTA JA3’ which has received funding from the European Union’s Health Programme (2014-2020). The content of this Assessment Report represents a consolidated view based on the consensus within the Authoring Team; it cannot be considered to reflect the views of the European Network for Health Technology Assessment (EUnetHTA), EUnetHTA’s participating institutions, the European Commission and/or the Consumers, Health, Agriculture and Food Executive Agency or any other body of the European Union. The European Commission and the Agency do not accept any responsibility for use that may be made of the information it contains. Assessment team Author(s) Finnish Medicines Agency (Fimea), Finland Co-Author(s) Spanish Agency of Medicine and Sanitary Products (AEMPS), Spain Andalusian Unit for Health Technology Assessment (AETSA), Spain Dedicated French National Authority for Health (HAS), France Reviewer(s) Agency for Health Technology Assessment and Tariff System (AOTMiT), Poland Regione Emilia-Romagna (RER), Italy Association of Austrian Social Insurance Institutions (DVSV), Austria Observer HTA Department/EC Ukraine, Ukraine March 2020 EUnetHTA Joint Action 3 WP4 1 PTJA09 - Brolucizumab for patients with neovascular (wet) AMD Further contributors External experts Prof. -

DRUG COVERAGE GUIDELINES Policy Number: PHARMACY 098.175 T0 Effective Date: June 1, 2018
UnitedHealthcare® Oxford Clinical Policy DRUG COVERAGE GUIDELINES Policy Number: PHARMACY 098.175 T0 Effective Date: June 1, 2018 Table of Contents Page Related Policies INSTRUCTIONS FOR USE ......................................................................... 1 Refer to Payment Guidelines below CONDITIONS OF COVERAGE ..................................................................... 1 DESCRIPTION OF SERVICES ..................................................................... 2 DEFINITIONS ......................................................................................... 3 PAYMENT GUIDELINES ............................................................................. 3 POLICY HISTORY/REVISION INFORMATION ............................................ 161 INSTRUCTIONS FOR USE This Clinical Policy provides assistance in interpreting Oxford benefit plans. Unless otherwise stated, Oxford policies do not apply to Medicare Advantage members. Oxford reserves the right, in its sole discretion, to modify its policies as necessary. This Clinical Policy is provided for informational purposes. It does not constitute medical advice. The term Oxford includes Oxford Health Plans, LLC and all of its subsidiaries as appropriate for these policies. When deciding coverage, the member specific benefit plan document must be referenced. The terms of the member specific benefit plan document [e.g., Certificate of Coverage (COC), Schedule of Benefits (SOB), and/or Summary Plan Description (SPD)] may differ greatly from the standard benefit plan -

Treatment of Intractable Diabetic Macular Edema with Pegaptanib Versus Bevacizumab, Both in Combination with Dexamethasone Diana M
Kansas Journal of Medicine 2012 Intractable Diabetic Macular Edema Treatment of Intractable Diabetic Macular Edema with Pegaptanib Versus Bevacizumab, Both in Combination with Dexamethasone Diana M. Leitner, M.D.1, David M. Chacko, M.D., Ph.D.1,2, Philip Twumasi-Ankrah, Ph.D.3, Elizabeth Ablah, Ph.D., M.P.H.3 1University of Kansas School of Medicine-Wichita Department of Internal Medicine 2Grene Vision Group, Wichita, KS 3 University of Kansas School of Medicine-Wichita Department of Preventive Medicine and Public Health Abstract Background . Diabetic macular edema is a significant cause of vision loss, and some patients do not respond optimally to existing treatments. This study compared the response of intractable diabetic macular edema to intravitreal injection of two anti-VEGF drugs, bevacizumab and pegaptanib, both in combination with dexamethasone. Methods . A retrospective chart review was conducted to examine patients from an ophthalmology practice in one year with diabetic macular edema (DME), recurrent or persistent, after focal laser or intravitreal bevacizumab. Patients received bevacizumab/dexamethasone or pegaptanib/dexamethasone. Outcome measures were improvement in best corrected visual activity (converted to LogMAR) and central macular thickness (CRT). Data on adverse effects also were collected. Results. The bevacizumab/dexamethasone group included 25 eyes which had pre-treatment LogMAR = 0.69 ± 0.49 (mean ± SD) and CRT = 419 ± 131. Post-treatment LogMAR was 0.70 ± 0.48 and CRT = 377 ± 107. The pegaptanib/dexamethasone group included 14 eyes; pre- treatment LogMAR = 0.80 ± 0.55 and CRT = 520 ± 108. Post-treatment LogMAR was 0.77 ± 0.49 and CRT = 46 4 ± 106.