California Statewide Trauma System Triage and Transfer Resource Guide 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Access+ HMO 2021Network
Access+ HMO 2021Network Our Access+ HMO plan provides both comprehensive coverage and access to a high-quality network of more than 10,000 primary care physicians (PCPs), 270 hospitals, and 34,000 specialists. You have zero or low copayments for most covered services, plus no deductible for hospitalization or preventive care and virtually no claims forms. Participating Physician Groups Hospitals Butte County Butte County BSC Admin Enloe Medical Center Cohasset Glenn County BSC Admin Enloe Medical Center Esplanade Enloe Rehabilitation Center Orchard Hospital Oroville Hospital Colusa County Butte County BSC Admin Colusa Medical Center El Dorado County Hill Physicians Sacramento CalPERS Mercy General Hospital Mercy Medical Group CalPERS Methodist Hospital of Sacramento Mercy Hospital of Folsom Mercy San Juan Medical Center Fresno County Central Valley Medical Medical Providers Inc. Adventist Medical Center Reedley Sante Community Physicians Inc. Sante Health Systems Clovis Community Hospital Fresno Community Hospital Fresno Heart and Surgical Hospital A Community RMCC Fresno Surgical Hospital San Joaquin Valley Rehabilitation Hospital Selma Community Hospital St. Agnes Medical Center Glenn County Butte County BSC Admin Glenn Medical Center Glenn County BSC Admin Humboldt County Humboldt Del Norte IPA Mad River Community Hospital Redwood Memorial Hospital St. Joseph Hospital - Eureka Imperial County Imperial County Physicians Medical Group El Centro Regional Medical Center Pioneers Memorial Hospital Kern County Bakersfield Family Medical -

Hospital Organ Donation Campaign Recognition for Outreach
Hospital Organ Donation Campaign Recognition for Outreach The hospitals listed below reached gold, silver, and bronze recognition levels for their organ, eye, and tissue donation and registration efforts between August 1, 2014, and April 30, 2015. The hospitals worked closely with their organ procurement organizations and Donate Life America affiliates to educate and register new donors. In many states, the participation of state hospital associations was pivotal to the hospitals’ efforts. DLA and hospital association participation is indicated in the title line for each state. OPO participation is listed in the OPO recogni- tion list at the end of the document. SEARCH BY STATE: A B C D E F G H I J K L M N O P Q R S T U V W X Y Z OPO RECOGNITION ALABAMA • Donate Life Alabama 1 0 0 East Alabama Medical Center Y ARIZONA • Donate Life Arizona 3 11 28 • Arizona Hospital and Healthcare Association Abrazo Arizona Heart Hospital Y Abrazo Central Campus Y Abrazo Scottsdale Campus Y Abrazo West Campus Y American Liver Foundation Y Banner Boswell Medical Center Y Banner Casa Grande Regional Medical Center Y Banner Del E. Webb Medical Center Y Banner Desert Medical Center and Cardon Children’s Medical Center Y Banner Estrella Medical Center Y Banner Gateway Medical Center and Banner MD Anderson Cancer Center Y Banner Goldfield Medical Center Y Banner Ironwood Medical Center Y Banner Thunderbird Medical Center Y Banner University Medical Center—Tucson and South Campus* Y Barnet Dulaney Perkins Eye Center Y Carondelet St. Mary’s Hospital Y Chandler Regional Medical Center Y Cobre Valley Regional Medical Center Y Flagstaff Medical Center Y * denotes transplant centers 1 HonorHealth Deer Valley Medical Center Y HonorHealth John C. -
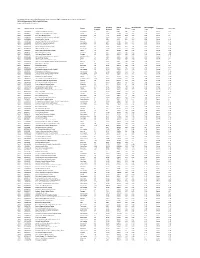
Appendix S3 C Diff Rates
Clostridium Difficile Infection (CDI) Standardized Infection Ratios (SIRs) in California General Acute Care Hospitals California Department of Public Health 2016 Data Lower is better, goal is 1.0 or less Infections Infections Patient SIR CI 95 Lower SIR CI 95 Upper Year CDPH Facility ID Facility Name County SIR Score Comparison SIR in 2015 Reported Predicted Days Limit Limit 2016 930000060 Glendora Community Hospital Los Angeles 8 2.81 5849 2.85 1.32 5.41 Worse 0.95 2016 60000007 Children's Hospital of Orange County Orange 58 21.96 47689 2.64 2.02 3.39 Worse 1.5 2016 930000035 Silver Lake Medical Center Los Angeles 20 7.74 16124 2.58 1.62 3.92 Worse 1.5 2016 250000344 Southwest Healthcare System, Wildomar Riverside 47 18.35 33228 2.56 1.9 3.38 Worse 2.3 2016 110000056 Sonoma Valley Hospital Sonoma 7 2.85 4759 2.45 1.07 4.85 Worse 1.79 2016 250000507 Southwest Healthcare System, Murrieta Riverside 27 11.26 24726 2.4 1.61 3.44 Worse 1.51 2016 930000082 Community Hospital Long Beach Los Angeles 20 8.96 15786 2.23 1.4 3.39 Worse 1.25 2016 930000108 Monterey Park Hospital Los Angeles 13 5.89 20399 2.21 1.23 3.68 Worse 2.29 2016 250000101 San Gorgonio Memorial Hospital Riverside 34 15.52 12601 2.19 1.54 3.03 Worse 1.63 2016 930000105 Olympia Medical Center Los Angeles 59 27.59 27338 2.14 1.64 2.74 Worse 1.89 2016 40001397 Fresno Heart and Surgical Hospital Fresno 13 6.44 11680 2.02 1.12 3.37 Worse 2.11 2016 30000123 Memorial Medical Center Stanislaus 85 43.6 77513 1.95 1.57 2.4 Worse 2.01 2016 60000015 Huntington Beach Hospital Orange 13 6.88 -

Hospital/Medi-Cal Paid Amounts
OSHPD Claim Medi-Cal Paid HOSPITAL NAME NUMBER DOS Year Type Amount Mandatory Enrollment of SPDs ALAMEDA CO MED CTR - HIGHLAND CAMPUS 106010846 10846 2009 Outpatient $ 5,204,390 0 $ - ALHAMBRA HOSPITAL 106190017 190017 2009 Outpatient $ 202,292 1 $ 202,292.16 ALTA BATES SUMMIT MED CTR-SUMMIT CAMPUS-HAWTHORN106010937 10937 2009 Outpatient $ 1,222,974 1 $ 1,222,974.37 ALVARADO HOSPITAL 106370652 370652 2009 Outpatient $ 559,136 1 $ 559,136.30 ANAHEIM GENERAL HOSPITAL 106301097 301097 2009 Outpatient $ 5,376 0 $ - ANAHEIM MEMORIAL MEDICAL CENTER 106301098 301098 2009 Outpatient $ 41,992 0 $ - ARROYO GRANDE COMMUNITY HOSPITAL 106400466 400466 2009 Outpatient $ 9,505 0 $ - BAKERSFIELD HEART HOSPITAL 106154101 154101 2009 Outpatient $ 129,951 1 $ 129,950.70 BAKERSFIELD MEMORIAL HOSPITAL- 34TH STREET 106150722 150722 2009 Outpatient $ 628,606 1 $ 628,606.08 BARSTOW COMMUNITY HOSPITAL 106361105 361105 2009 Outpatient $ 327,464 1 $ 327,463.59 BARTON MEMORIAL HOSPITAL 106090793 90793 2009 Outpatient $ 259,833 0 $ - BEAR VALLEY COMMUNITY HOSPITAL 106361110 361110 2009 Outpatient $ 77,871 0 $ - BEVERLY HOSPITAL 106190081 190081 2009 Outpatient $ 524,570 1 $ 524,570.03 BIGGS GRIDLEY MEMORIAL HOSPITAL 106040802 40802 2009 Outpatient $ 300,660 0 $ - BROTMAN MEDICAL CENTER 106190110 190110 2009 Outpatient $ 271,558 1 $ 271,558.23 CALIFORNIA PACIFIC MED CTR-DAVIES CAMPUS 106380933 380933 2009 Outpatient $ 594,435 0 $ - CALIFORNIA PACIFIC MED CTR-PACIFIC CAMPUS 106380929 380929 2009 Outpatient $ 1,372,565 1 $ 1,372,565.43 CASA COLINA HOSPITAL FOR REHAB -

Table 3: 1960 - 2017 Historic Hospital List by CODE
Table 3: 1960 - 2017 Historic Hospital List by CODE County Code Hospital Name Address City Zip 1 001 ALAMEDA HOSPITAL 2070 CLINTON AVE ALAMEDA 94501 1 002 ALTA BATES HOSPITAL AT ALBANY 1247 MARIN AVENUE ALBANY 94706 1 003 ALTA BATES MEDICAL CENTER 2450 ASHBY AVENUE BERKELEY 94705 1 004 BOOTH MEMORIAL HOSPITAL 2794 GARDEN STREET OAKLAND 94701 1 005 CHILDREN'S HOSPITAL 51ST & GROVE STREETS OAKLAND 94609 1 006 CIVIC CENTER HOSPITAL FOUNDATION 390 40TH STREET OAKLAND 94609 1 007 SAN LEANDRO HOSPITAL 13855 E 14TH STREET SAN LEANDRO 94578 1 008 EDEN MEDICAL CENTER 20103 LAKE CHABOT RD CASTRO VALLEY 94546 1 009 ESKATON DOCTORS HOSPITAL OAKLAND 4600 E FAIRFAX AVENUE OAKLAND 94601 1 010 FAIRMONT HOSPITAL 15400 FOOTHILL BOULEVARD SAN LEANDRO 94578 1 011 HAYWARD HOSPITAL 770 'A' STREET HAYWARD 94541 1 012 HERRICK MEMORIAL HOSPITAL 2001 DWIGHT WAY BERKELEY 94704 1 013 ACMC-HIGHLAND CAMPUS 1411 E. 31ST ST OAKLAND 94602 1 014 KAISER HOSPITAL: SAN LEANDRO 2500 MERCED STREET SAN LEANDRO 94577 1 015 KAISER HOSPITAL: OAKLAND 275 W. MACARTHUR BLVD OAKLAND 94611 1 016 SUMMIT MEDICAL CENTER - HAWTHORNE 350 HAWTHORNE AVENUE OAKLAND 94609 1 017 NAVAL HOSPITAL: OAKLAND 8750 MOUNTAIN BOULEVARD OAKLAND 94627 1 018 OAKLAND HOSPITAL CORPORATION 2648 EAST 14TH STREET OAKLAND 94601 1 019 OGORMAN INFANT 2587 - 35TH AVENUE OAKLAND 94601 1 020 PERALTA HOSPITAL 450 - 30TH STREET OAKLAND 94609 1 021 SUMMIT MEDICAL CENTER 3100 SUMMIT STREET OAKLAND 94623 1 022 ST. ROSE HOSPITAL 27200 CALAROGA AVE HAYWARD 94540 1 023 ST. PAUL'S HOSPITAL 813 J STREET LIVERMORE 94550 1 024 VALLEYCARE MEDICAL CENTER 5555 W. -

Physicians in Post-Graduate Training
Physicians in Post-Graduate Training - Affiliation Agreements Contract Effective Contractor Name Number Date Original Requesting Facility Barlow Respiratory Hospital H-201544 07/01/92 LAC+USC Medical Center Beth Israel Medical Center H-705478 10/24/12 Harbor-UCLA Medical Center Beverly Community Hospital Association dba Beverly Hospital H-702810 06/19/07 Harbor-UCLA Medical Center Bi-County Community Hospital H-202765 09/07/93 MLK California Hospital Medical Center H-208617 09/30/97 with Amendment #1 Camarillo State Hospital and Development Center H-204212 12/13/94 Olive View-UCLC Medical Center Cancer Institute Medical Group, Inc. H-700511 08/01/04 LAC+USC Medical Center Catholic Healthcare West (Amendment No. 1 = 8/01/06, for St. Mary MC only) H-700853-1 01/18/05 REPLACED WITH DIGNITY HEALTH Cedars-Sinai Medical Center H-701019-1 05/25/05 CFHS Holdings, Inc. H-700916-1 03/28/05 Children's Hospital Los Angeles H-703521 10/01/08 Children's Hospital of Orange County H-204570 05/18/95 LAC+USC Medical Center Children's Institute, INC. H-705950 12/24/13 Harbor-UCLA Medical Center Christina Care H-703771 05/01/09 City of Hope H-201659 10/01/92 Emergency Medical Services City of Hope National Medical Center H-204228 01/30/95 MLK CPC Alhambra Hospital H-205070 07/01/95 LAC+USC Medical Center Crenshaw Expo Medical Center H-702977 10/16/07 Harbor-UCLA Medical Center DCH Foundation Hospitals H-205915 06/26/96 LAC+USC Medical Center Dept. of Veterans Affairs - VA Greater Los Angeles Healthcare System H-702820 06/19/07 Dept. -
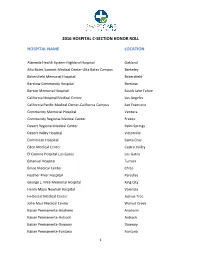
2016 Hospital C-Section Honor Roll List
2016 HOSPITAL C-SECTION HONOR ROLL HOSPITAL NAME LOCATION Alameda Health System-Highland Hospital Oakland Alta Bates Summit Medical Center-Alta Bates Campus Berkeley Bakersfield Memorial Hospital Bakersfield Barstow Community Hospital Barstow Barton Memorial Hospital South Lake Tahoe California Hospital Medical Center Los Angeles California Pacific Medical Center-California Campus San Francisco Community Memorial Hospital Ventura Community Regional Medical Center Fresno Desert Regional Medical Center Palm Springs Desert Valley Hospital Victorville Dominican Hospital Santa Cruz Eden Medical Center Castro Valley El Camino Hospital-Los Gatos Los Gatos Emanuel Hospital Turlock Enloe Medical Center Chico Feather River Hospital Paradise George L. Mee Memorial Hospital King City Henry Mayo Newhall Hospital Valencia Hi-Desert Medical Center Joshua Tree John Muir Medical Center Walnut Creek Kaiser Permanente-Anaheim Anaheim Kaiser Permanente-Antioch Antioch Kaiser Permanente-Downey Downey Kaiser Permanente-Fontana Fontana 1 2016 HOSPITAL C-SECTION HONOR ROLL Kaiser Permanente-Fresno Fresno Kaiser Permanente-Modesto Modesto Kaiser Permanente-Oakland Oakland Kaiser Permanente-Panorama City Panorama City Kaiser Permanente-Redwood City Redwood City Kaiser Permanente-Riverside Riverside Kaiser Permanente-Roseville Roseville Kaiser Permanente-San Francisco San Francisco Kaiser Permanente-San Jose San Jose Kaiser Permanente-San Leandro San Leandro Kaiser Permanente-Santa Rosa Santa Rosa Kaiser Permanente-South Sacramento Sacramento Kaiser Permanente-Vacaville -
Supplemental Information
ARTICLE Supplemental Information SUPPLEMENTAL TABLE 5 Participating Hospitals Hospital City State or Province Abington Memorial Hospital Abington Pennsylvania Adventist Hinsdale Hospital Hinsdale Illinois Advocate Good Samaritan Hospital Downers Grove Illinois Advocate Lutheran General Hospital Park Ridge Illinois Affinity NICU at St Elizabeth Hospital Appleton Wisconsin Akron Children’s Hospital Akron Ohio Akron Children’s SCN at St Elizabeth Youngstown Ohio Akron Children’s Special Care Nursery at Summa Akron Ohio Albany Medical Center Albany New York Albert Einstein Medical Center Philadelphia Pennsylvania Alegent Health Bergen Mercy Medical Center Omaha Nebraska All Children’s at Sarasota Memorial Sarasota Florida All Saints Episcopal Hospital Fort Worth Texas Allegheny General Hospital Pittsburgh Pennsylvania Allentown’s Neonatal Intensive Care Allentown Pennsylvania Alta Bates Summit Medical Center Berkeley California Anaheim Regional Medical Center Anaheim California Anderson Regional Medical Center Meridian Mississippi Anne Arundel Medical Center Annapolis Maryland Antelope Valley Hospital Lancaster California Arkansas Children’s Hospital Little Rock Arkansas Arnot Ogden Medical Center Elmira New York Arrowhead Regional Medical Center Colton California Aspirus Wausau Hospital Wausau Wisconsin Athens Regional Medical Center Athens Georgia Aultman Hospital Canton Ohio Aurora Baycare Medical Center Green Bay Wisconsin Aurora Sinai Medical Center Milwaukee Wisconsin Aurora Women’s Pavilion West Allis Wisconsin Avera McKennan Sioux -
Chamcn063009
Enrollment Company Name County Month Year Alameda County Medical Center Highland Campus Alameda 6 2009 Alhambra Hospital Medical Center Los Angeles 6 2009 Alta Bates Summit Medical Center ‐ Summit Campus‐Hawthorne Alameda 6 2009 Alvarado Hospital San Diego 5 2009 Anaheim General Hospital Orange 1 2009 Arroyo Grande Community Hospital San Luis Obispo 3 2009 Bakersfield Heart Hospital Kern 1 2009 Banner Lassen Medical Center Lassen 6 2009 Barlow Respiratory Hospital Los Angeles 6 2009 Bellflower Medical Center Los Angeles 6 2009 Beverly Hospital Los Angeles 3 2009 BHC Alhambra Hospital Inc Los Angeles 6 2009 Biggs‐Gridley Memorial Hospital Butte 12 2008 California Department of Veterans Affairs Napa 12 2008 California Pacific Medical Center San Francisco 6 2009 Casa Colina Hospital Los Angeles 6 2009 Catalina Island Medical Center Los Angeles 6 2009 Cedars‐Sinai Medical Center Los Angeles 6 2009 Central Valley General Hospital Kings 3 2009 Chapman Medical Center Orange 6 2009 Childrens Hospital of Los Angeles Los Angeles 6 2009 Childrens Hospital of Orange County Orange 1 2009 Childrens Hospital/Research Ctr Oakland Alameda 6 2009 Chino Valley Medical Center San Bernardino 1 2009 CHW ‐ Mercy San Juan Medical Center Sacramento 6 2009 City of Alameda Health Care District Alameda 2 2009 City of Hope Los Angeles 3 2009 College Hospital Costa Mesa Orange 3 2009 Colusa Regional Medical Center Colusa 6 2009 Community Behavioral Health Center Fresno 2 2009 Community Hospital Monterey Peninsula Monterey 1 2009 Community Hospital of Long Beach Los -

OSHPD FACILITY CODES -‐-‐-‐ Sorted by Hospital (JAN 2018)
OSHPD FACILITY CODES --- Sorted by Hospital (JAN 2018) CPQCC Centers Indicated in Bold Italics OSHPD # HOSPITAL NAME CITY COUNTY 700564 30TH MEDICAL GROUP HOSPITAL 700597 60TH MEDICAL GROUP HOSPITAL 700431 722ND MEDICAL GROUP 700103 95TH MEDICAL GROUP - EDWARDS AIR FORCE BASE 150808 ADVENTIST HEALTH MEDICAL CENTER TEHACHAPI VALLEY TEHACHAPI KERN 164029 ADVENTIST MEDICAL CENTER HANFORD KINGS 100797 ADVENTIST MEDICAL CENTER - REEDLEY REEDLEY FRESNO 100793 ADVENTIST MEDICAL CENTER-SELMA SELMA FRESNO 010735 ALAMEDA HOSPITAL ALAMEDA ALAMEDA 010989 ALAMEDA HOSPITAL AT WATERS EDGE ALAMEDA ALAMEDA 190017 ALHAMBRA HOSPITAL MEDICAL CENTER ALHAMBRA LOS ANGELES 010844 ALTA BATES SUMMIT MED CTR-HERRICK CAMPUS BERKELEY ALAMEDA 010937 ALTA BATES SUMMIT MED CTR-SUMMIT CAMPUS-HAWTHORNE OAKLAND ALAMEDA 013626 ALTA BATES SUMMIT MED CTR-SUMMIT CAMPUS-SUMMIT OAKLAND ALAMEDA 010739 ALTA BATES SUMMIT MEDICAL CENTER BERKELEY ALAMEDA 370652 ALVARADO HOSPITAL MEDICAL CENTER SAN DIEGO SAN DIEGO 301097 ANAHEIM GENERAL HOSPITAL ANAHEIM ORANGE 301098 ANAHEIM REGIONAL MEDICAL CENTER ANAHEIM ORANGE 341051 ANDERSON LUCCHETTI WOMEN'S AND CHILDREN'S CENTER SACRAMENTO SACRAMENTO 190034 ANTELOPE VALLEY HOSPITAL LANCASTER LOS ANGELES 364231 ARROWHEAD REGIONAL MEDICAL CENTER COLTON SAN BERNARDINO 154101 BAKERSFIELD HEART HOSPITAL BAKERSFIELD KERN 150722 BAKERSFIELD MEMORIAL HOSPITAL BAKERSFIELD KERN 184008 BANNER LASSEN MEDICAL CENTER SUSANVILLE LASSEN 190052 BARLOW RESPIRATORY HOSPITAL LOS ANGELES LOS ANGELES 364430 BARSTOW COMMUNITY HOSPITAL 090793 BARTON MEMORIAL HOSPITAL -

California Children Services Approved Hospital Report
California Children Services Approved Hospital Report NPI Legal Name Business Name Facility Type StartDt EndDt County Address Phone 1770587107 Asante Rogue Valley Medical Center Standard 05/12/1980 2825 E Barnett Road (541) 789-4728 Medford OR 97504-8332 1124098421 Renown Regional Med Ctr Renown Regional Med Ctr Standard 01/01/1979 1155 Mill Street (775) 982-4100 Reno NV 89502-1474 1659340370 Sky Lakes Medical Center Sky Lakes Medical Center Limited 01/01/1995 2865 Daggett Avenue (541) 274-6221 Klamath Falls OR 97601-1106 1265421887 St Marys Hospital St Marys Hospital Standard 01/01/1979 235 W 6th Street Reno NV 89503-4548 General Community (over 14 without 1396764353 Alameda Health System Highland General Hospital pediatric license) 12/27/2005 Alameda 1411 E 31st Street (510) 437-4800 Oakland CA 94602-1018 1003961251 Childrens Hospital Medical Childrens Hospital And Resea Tertiary 11/01/1984 Alameda 747 52nd Street (510) 428-3000 Oakland CA 94609 1942298153 Hayward Sisters Hospital St Rose Hosp Limited 03/01/1974 Alameda 27200 Calaroga Avenue (510) 264-4000 Hayward CA 94545-4383 1427123132 Kaiser Foundation Hosp Kaiser Foundation Hosp Tertiary 04/06/2009 Alameda 275 W Macarthur Boulevard (415) 653-6121 Oakland CA 94611-5641 General Community (over 14 without 1649605403 Kaiser Foundation Hospital Kaiser Foundation Hospital pediatric license) 08/25/2014 Alameda 2500 Merced Street (510) 454-1000 San Leandro CA 94577-4201 9/18/21 6:25 PM Page 1 of 20 NPI Legal Name Business Name Facility Type StartDt EndDt County Address Phone 1639523004 -

Dignity Health – Alternate Hospital List
Dignity Health – Alternate Hospital List Terminating Hospital Street Address City State Zip Code County Name BAKERSFIELD MEMORIAL HOSPITAL 420 34TH ST BAKERSFIELD CA 93301 KERN Alternate Hospitals Street Address City State Zip Code County Name ADVENTIST HEALTH BAKERSFIELD 2615 CHESTER AVE BAKERSFIELD CA 93301 KERN BAKERSFIELD HEART HOSPITAL 3001 SILLECT AVE BAKERSFIELD CA 93308 KERN GOOD SAMARITAN HOSPITAL 901 OLIVE DR BAKERSFIELD CA 93308 KERN KERN MEDICAL CENTER 1700 MOUNT VERNON AVE BAKERSFIELD CA 93306 KERN Terminating Hospital Street Address City State Zip Code County Name CALIFORNIA HOSPITAL MEDICAL CENTER 1401 S GRAND AVE LOS ANGELES CA 90015 LOS ANGELES Alternate Hospitals Street Address City State Zip Code County Name ADVENTIST HEALTH WHITE MEMORIAL HOSPITAL 1720 E CESAR E CHAVEZ AVE LOS ANGELES CA 90033 LOS ANGELES AHMC MONTEREY PARK HOSPITAL 900 S ATLANTIC BLVD MONTEREY PARK CA 91754 LOS ANGELES ALTA LOS ANGELES HOSPITALS INC. 4081 E OLYMPIC BLVD LOS ANGELES CA 90023 LOS ANGELES BARLOW RESPIRATORY HOSPITAL 2000 STADIUM WAY LOS ANGELES CA 90026 LOS ANGELES CHILDRENS HOSPITAL LOS ANGELES 4650 W SUNSET BLVD LOS ANGELES CA 90027 LOS ANGELES COMMUNITY HOSPITAL OF HUNTINGTON PARK 2623 E SLAUSON AVE HUNTINGTON PARK CA 90255 LOS ANGELES DOCS SURGICAL HOSPITAL LLC 6000 SAN VICENTE BLVD LOS ANGELES CA 90036 LOS ANGELES EAST LOS ANGELES DOCTORS HOSPITAL 4060 WHITTIER BLVD LOS ANGELES CA 90023 LOS ANGELES GOOD SAMARITAN HOSPITAL 1225 WILSHIRE BLVD LOS ANGELES CA 90017 LOS ANGELES HOLLYWOOD PRESBYTERIAN MEDICAL CENTER 1300 N VERMONT AVE