Reducing Allergic Airway Inflammation with High-Density Microprojection Array Skin Patches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Courier Gazette
T he Courier-G r ie. ROCKLAND GAZETTE ESTABLISHED 1S4O.) ROCKLAND COCKIER EHTAIII.ISHEI) 1S74.| O n |1rcss is % ^rtlftmchcan $cber that Iftobcs Ijjc &?lorlb at £too Dollars a ilcar l TWO DOLLARS A YEAR IN ADYANCBi 1 MINGLE COPIES PRICE FIVE CKNT8, V o l. 8 , — N ew S e r ie s . ROCKLAND, MAINE, TUESDAY, APRILS, 1889. N umber 13. ? p p ? W here cnt» I invest my s h t in g s Hint, th e y H.GALI.ERT’S may lie safe nnil yet yield me n good rate of Interest? T I I 13 OFFERINC House Furnishing Co. (O F M A IN E) OF •AYR IT S ST O CK H O LDERDERR 10 PER LADIES’ SPRINC CENT ’cr A nnum DIVIDENDS JANUARY ANU JULY. For full particnlars call on or write JACKETS! DAV1I) W. SEARS, 17 Milk SI. S-20 ROOM f», BOSTON. Or the Treasurer of the Company, Portland, Me JACKETS ! = HOTEL ST. CTEKB5Sfi?HBW3iWH Fifth Ave. and 39th St., N. Y. JACKETS! Zfcu American Plan $4 OD per day; Bath and Parlors extra. European Plan $1.50 per day and upwards, Among the many New Goods we are LON NUTTER, : Proprietor. J now daily receiving for our Spring Fornv-rly op Bangor Steamship Line. j Trade, we call especial attention to ROCKLAND TOW BOAT our COMPAMY. NEW STYLES OF id B ritannia. This Company has Two Good Boats, one large for outside work, and the other smaller for inside Ladies’ Jersey and Cloth work, and are prepared to receive orders for any towing job that may come up, either Inside or Outside, Anywhere Along J a c k e ts ! the Coast of Maine. -

Annual General Meeting Season 2008 - 2009
Annual General Meeting Season 2008 - 2009 AGENDA FOR ANNUAL GENERAL MEETING, 26 MAY 2009 1. Attendance & Apologies 2. Confirmation of Minutes of AGM held 21st May 2008 3. Business arising from 21st May 2008 meeting 4. Reports 5. Affiliation Fees for 2008/2009 Season 6. Election of Board Members 7. Confirmation of Sub-Committee Chairpersons for 2008/2009 8. Confirmation of Yachting Australia Delegates 9. Confirmation of Auditor 10. Close of Meeting 2008/09 Yachting SA Roll of Honour The Board of Yachting SA congratulates the following South Australian sailors on their outstanding achievements. YSA Awards for Season 2007/2008 Sailor of the Year ~ jointly awarded to Craig McPhee & Gillian Berry Junior Sailor of the Year ~ awarded jointly to Lauren Thredgold & Megan Soulsby Volunteer of the Year ~ awarded jointly to Gary Day & Greg Hampton President’s Award ~ jointly awarded to Les Harper & David Tillett 2008/2009 National Champions Australian Sharpie Malcolm Higgins Sam Sanderson Andrew Chisolm National Champion Brighton & Seacliff YC Brighton & Seacliff YC Brighton & Seacliff YC International Fireball Robins Inns Joel Coultas National Champion Adelaide SC Adelaide SC International 505 Alexander Higgins Jordan Spencer National Champion Brighton & Seacliff YC Brighton & Seacliff YC Laser Sean Homan Grand Master Adelaide SC National Champion Mosquito Mk II Cat. Warwick Kemp Emily Fink National Champion Adelaide SC Adelaide SC Yvonne 20 Paul Hawkins Graham Lovell National Champion Victor Harbor YC Victor Harbor YC Yachting SA Annual Report 2008/2009 May 2009 ITEM 1 Attendance & Apologies Attendance Register and Voting Rights All attendees are required to sign the attendance register before the meeting commences or upon arrival. -

APRIL 2018 Ost Club Members Know That I Am an They Say “Any Fool Can Steer a Ship, It’S Old-School Navigation Geek
Opening Day APRIL 2018 ost Club members know that I am an They say “any fool can steer a ship, it’s old-school navigation geek. Paper From the knowing where to go that’s the trick.” It’s Mcharts, parallel rules, dividers, tables, kind of fun knowing that you can find your chronometers, the works. As a young man I Commodore position anywhere on the earth without the 24 was privileged to have had the opportunity to special billion-dollar satellites. learn celestial navigation from some of the Most everyone knows that in the late best teachers in the country, and in the 1970s I 1600s, when celestial navigation was just put that knowledge to use as navigator aboard beginning to become a reliable tool to find various freighters. I used it aboard yachts as one’s way on the globe, the British Navy felt well back in the ’70s and ’80s, and continue that having an accurate timepiece aboard ships today to practice the art in spite of having all was essential to safe celestial navigation, and sorts of modern electronic navigation tools, promised a fortune to the first citizen who simply because I think it’s good for the soul could solve the problem of keeping proper to know that, without any of it, and with only time at sea. Much has been written about the very basic equipment, you can find your way “search for longitude,” which has everything anywhere on the Blue Marble. to do with knowing the precise time. Josh By the time you read this, you will have Slocum, the wise, highly experienced, crusty heard about an event at the Club that was Commodore Mike Blecher old sea captain who solo-circumnavigated for conceived by Junior Commodore Ryan Janov. -

BSYC LOG BOOK - ADVERTISING RATES Much Looking Forward to Resuming Full Page More Actual On-The-Water Activity
LOG BOOK MAY 2020 www.bsyc.com.au RLA 152339 at Brighton JR Manufacturing Jeweller James Ramsey Mobile 0451 470 463 254 Brighton Road Somerton Park SA 5044 Next to Tradelink [email protected] Find us on Facebook Opening Hours Tuesday to Friday, 10.00am - 5.00pm $10 FREE $20 Watch Battery Clean, Polish and Rhodium Plate Per Item Safety Check Per Item DIARY DATES EDITOR’S CORNER Covid 19 restrictions Amazingly the coronavirus has not Stay tune for updates dampened the issue of Log Book content with so many articles, many of them of historical interest as well as the intrigues of on-line sailing. Of course we are all very BSYC LOG BOOK - ADVERTISING RATES much looking forward to resuming Full Page more actual on-the-water activity. Black & White $665 12 months Fortunately many of our junior Colour $760 fleet, whilst obeying the isolation Half Page code-of conduct, have been able to Black & White $400 12 months continue to hone their sailing skills. Colour $470 It also does appear that we might Business Card be on the verge of re-establishment Black & White $270 12 months of our BSYC social skills…here’s to (Prices are GST inclusive) it!! Editor: Nancy Higgins Nancy Higgins FLAG OFFICERS & MANAGEMENT COMMITTEE 2019/2020 SEASON COMMODORE: Lisa Brock VICE COMMODORE: Peter Woolman REAR COMMODORE: Phil Scapens TREASURER: Martin Pike RETIRING COMMODORE: Rob Turton On a sad note we say farewell to COMMITTEE: Andrew Dallisson two old BSYC members who have Darren Witty Jim Lelliott recently passed away, Chris Todd Vale Bill Corbett and Erica West Doug Nairn Tim Lelliott Rebecca Office Note: Please note that the log books Wigglesworth will be sent out via email only. -

Yachting Western Australia – Yearbook 2013 – 2014 | Page 1 YACHTING WESTERN AUSTRALIA (INC)
YEAR BOOK 2013-2014 SHACKS HOLDEN SUPPORTING YOU ON WATER & LAND. SHACKS HOLDEN SUPPORTING YOU ON WATER & LAND. 9432 9432 SHACKS 64 QUEEN VICTORIA ST FREMANTLE www.shacksholden.com.au HOLDEN 9432 9432 SHACKS 64 QUEEN VICTORIA ST FREMANTLE [email protected] HOLDEN [email protected] DL3711 INDEX YWA Office Bearers 2 INFORMATION YWA Past Presidents 2 Sailing Pathways 12 YWA Life Members 2 Swan River Racing Committee 13 What Does Yachting WA Do For You 3 Definitions of Coastal Yacht Racing Areas 13 Club Census 18 REPORTS Recreational Skippers Ticket 19 President 5 Affiliated Yacht Clubs 21 General Manager 6 Yacht Club Information 22 Coastal Committee 7 Swan River Yacht Racing Course Marks 26 Offshore Racing Committee 7 Affiliated Class Associations 31 Racing Rules Committee 7 Class Association Information 32 Race Management Committee 8 SPECIAL EVENTS REVIEW Recreational Skippers Ticket 8 Cock of the Swan 2013 41 Safety Committee 8 Fremantle to Bali 42 Swan River Racing Committee 9 Honorary Service 43 Development & participation 9 Ron Tough Yachting Foundation 44 Cruising & Power Yacht Committee 10 WA Yachting Awards 45 Yachting WA Cruising and Power Yacht Committee 11 Front Cover: Tackers Programme at Mandurah Offshore Fishing and Sailing Club YACHTING WA BOARD OF MANAGEMENT 2013-2014 President Vice President Treasurer Board Member Board Member DENYS PEARCE MARK FITZHARDINGE JOHN HEYDON MARK DONATI ALAN JOHNS Board Member since 2010 aBoard Member since Elected August 2009. Elected August 2010 Elected August 2004 -
Service and War Notes
aTmqe ^otcs. Tiie number of casualties among officers reported in the fourteen days, 1st to 14th July inclusive, was 636, of which 320 occurred in the Dardanelles, 305 in Flanders, and eleven in other seats of war, as follows :? ?S % 1 ?2 T3 3 ? ? rf v o 'I.2 ?" -2 * 3 ? S ? ? Dardanelles. Naval officers ?? ??? 4 1 16 21 ??? ??? ... British officers 6'- ... _ 113 38 213 ... British officers, Indian troops 6 ... 16 22 ... ??? officers 4 ... Indian 8 ... ... 12 ... ??? H ... Australians 21 1 ... J-3 ... ... Zealanders 2 ... New 16 1 ... 19 Flanders. British officers ... ... 80 2 ISO 13 4 279 ... British officers, Indian troops 4 ... 2 v fj Indian officers ... 1 10 11 Canadians . ... ... 2 ... 5 ... 2 9 Persian Gulf. British ... ... officers 6 6 Indian ... officers 1 1 Aden ... ... ... 3 3 Cameroons ... .. 1 1 Total ... 175 5 397 - 53 (i 636 356 THE INDIAN MEDICAL GAZETTE. [Sept., 1915. Four of the cases shown as wounded in Flanders were Liverpool, before the war broke out, when he took a suffering from gas poisoning. The chief feature of the week's temporary commission as Lieutenant in the It. A. M. C. from casualties was the great loss incurred by three Scottish 17th September 1914. territorial battalions in the Dardanelles. The 4th Royal Lieutenant-Colonel William Bridgett Pritchard, Scots lost 21 ten seven and four officers, killed, wounded, r.a.m.c. (T. P.), died of wounds in the Dardanelles, was missing ; while the 7th and 8tli Cameronians, or Scottish Ritles, educated at Owen's College, Manchester, and took the lost 37, three killed, fifteen wounded, and nineteen missing. -

D. Enrique Corominas Presidente Del Real Club Náutico De Barcelona
EDITORIAL ha procedido a la instalación de un pantalán para la escuela, a la señalización de la zona del varadero y a la optimización de espacios en los sótanos. El Club tiene además una vertiente social importante. El restaurante ha mejorado notablemente, gracias a la excelente labor del equipo ejecutivo de esta sección. Aprovecho para agradecer a Felipe Klein su excelente labor como delegado de la Junta quien, por haber cambiado de residencia, pre- sentó su renuncia. Para remplazarle la Junta ha nombrado a Marcos Palomar para tal menester y creo seguirá la buena senda que su antecesor le marcó. Las instalaciones del comedor se están renovando, se ha cambiado la climatización del edificio social, se ha sustituido la moqueta etc., etc., -siempre de acuerdo con nuestras posi- bilidades-, y espero que en pocos meses podamos ya presen- tar unas instalaciones dignas de nuestro Club. Todo ello sin alterar el equilibrio económico que deben siempre presentar nuestras finanzas. En ello, la Junta será siempre muy cautelosa. No temáis. D. Enrique Corominas He escrito al empezar que también desearía hablar del fu- Presidente del Real Club Náutico turo. de Barcelona El Club está limitado geográficamente, y nos es muy difícil crecer. Estamos a tope de amarres. Podríamos admitir algu- nos socios más pero, claro, sin más amarres no hay nuevos socios. Estamos dándole vueltas al tema, pero teniendo claro “Este número de nuestra revista social coincidirá con las pri- que, de la localización actual, inmejorable, no nos movere- meras fechas del nuevo año. Considero oportuno hacer un mos. La ampliación de nuestras palancas pasaría por el “Moll breve resumen de lo que fue el pasado ejercicio y apuntar de la Fusta”, y en ello estamos, si bien no se nos escapa la algunas ideas sobre nuestra actividad en el año que recién problemática que ello podría acarrear en cuanto a seguridad, comenzamos. -
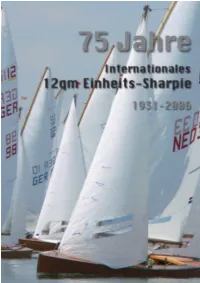
Buch 75Jahre Sharpie
75 Jahre Internationales 12qm Einheits Sharpie 1931-2006 Layout und Text: U.Peters Redaktion: S.Wussow, U.Peters Übersetzungen: G. Daubenmerkel 2 .......wenn die Renaissance in dieser Bootsklasse weiter anhält, wird es nicht die letz- te Geschichte über das 12qm Sharpie bleiben.Sie kann nicht lückenlos sein - denn selbst bei dem Aufbau dieser Chronik gab es im Verlauf der Arbeiten immer wieder Neuheiten, die wir natürlich auch einarbeiten wollten. Leider gibt es aus den 60er und siebziger Jahren noch nicht soviel Bildmaterial wie aus dem letzten Jahrzehnt. Erfreulich bei der Klassenentwicklung und des Klassenlebens ist die Tatsache, dass auch viele junge Segler das Boot für sich entdeckt haben - in Holland ist es der Förderung durch die Klassenvereinigung mit dem Promotie-Boot - einem restaurier- ten Boot, dass sich im Besitz der Klassenvereinigung befindet und gegen eine Gebühr und Pflegeeinsatz jungen Mannschaften zur Verfügung gestellt wird - auch wesentlich zu verdanken. In Deutschland können wir nur hoffen, dass wir den Bestand wieder etwas erhöhen. Das eine oder andere Boot ist ja schon wieder dazu gekommen. Mit einem Stand auf der “Boatfit” im letzten Jahr ist eine intensivere Werbung für das Boot begonnen worden und wird sich sicher auch fortsetzen lassen. Die beste Werbung für das Boot ist natürlich die rege Beteilung an Regatten im In- und Ausland. Da reicht die Palette der Veranstaltungen von der Holzboot-Regatta über die nationalen offenen Meisterschaften bis hin zur Europameisterschaft auf ständig wechselnden Revieren in Portugal, England, Holland und Deutschland. Wenn es auf den EM’s der 60er und 70er Jahre Meldezahlen von 25-30 Booten gab so sind es in den letzten Jahren schon bis zu 65 Sharpies. -

2007 Texas Reading Club Manual Sail Away with Books!
Sail Away With Books! 1 2007 Texas Reading Club Manual 2007 Texas Reading Club Manual Sail Away With Books! Written By: Barrie Alguire, Miranda Bauer, Linda Befeld, Sara Bracht, Debbie Brightwell Brown, Lucina Carpenter, Paola Ferate-Soto, WyLaina Hildreth, Shelly Lane, and Christine McNew Clip Art By: Diane Stanley and Shawn Clements Theme Songs By: Lucas Miller and Sally Meyers Craft Patterns and Illustrations By: Shawn Clements Edited By: Jeanette Larson and Christine McNew Published By: The Library Development Division of the Texas State Library and Archives Commission, Austin, Texas 2007 2 Sail Away With Books! Table Of Contents Preface 4 Something About the Artist 5 Acceptable Use of Artwork 6 Something About the Authors and Songwriters 8 Introduction 11 Theme Songs 34 Reader's Theater Scripts 38 Puppet Plays 47 Stories 57 Celebrations Programs Chapter 60 Family Program 76 Bilingual Programs Chapter 85 Toddler Programs Chapter 146 Preschool Programs Chapter 206 Elementary Programs Chapter 278 Young Adult Programs Chapter 320 Bibliography 364 3 2007 Texas Reading Club Manual Preface This manual is created for the 2007 Texas Reading Club, a program of the Library Development Division of the Texas State Library and Archives Commission. The theme is “Sail Away with Books!” in English and “¡Navega lejos con libros!” in Spanish. The programs invite children to explore oceans, lakes, boats, voyages, water sports, pirates, and many related topics. The 2007 Texas Reading Club manual is available on CD-ROM and online at the Texas State Library web site, www.tsl.state.tx.us/ld/projects/trc/2007/index.html. Children’s book illustrator, Diane Stanley, created the artwork for the 2007 Texas Reading Club. -
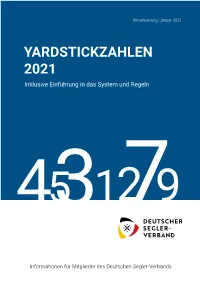
YARDSTICKZAHLEN 2021 Inklusive Einführung in Das System Und Regeln
Aktualisierung: Januar 2021 YARDSTICKZAHLEN 2021 Inklusive Einführung in das System und Regeln 4531279 Informationen für Mitglieder des Deutschen Segler-Verbands Aktualisierung: Januar 2021 YARDSTICKZAHLEN 2021 Inklusive Einführung in das System und Regeln HIGH GLOSS — DURABLE & REPAIRABLE — TRUE COLOR NEXT GENERATION TOPCOAT 45 1279 awlgrip.com 3 facebook.com/awlgripfinishes twitter.com/awlgrip instagram.com/awlgripfinishes All trademarks mentioned are owned by, or licensed to, the AkzoNobel group of companies. Informationen für Mitglieder des Deutschen Segler-Verbands © AkzoNobel 2021. 9861/0121 IPL0121879480-001_Awlgrip_HDT_IT_105x148.indd 1 22/01/2021 10:46 Yardstick Deutschland Yachten desselben Serientyps, für die eine YS-Zahl gilt, müssen Von Dietrich Kralemann also dieselben Konstruktionsmerkmale des Rumpfes (Tiefgang, Motorausrüstung, Verdrängung, Kielgewicht, Kielform und -mate- Motto: Fair segeln, mit fairen Mitteln gewinnen! rial u. ä.) und denselben Ausrüstungsstandard von Rigg und Segeln aufweisen. 1. Allgemeine Zielsetzungen Bei den vom DSV anerkannten Klassen und Werftklassen gibt es in Der DSV beabsichtigt mit dem von ihm propagierten und jährlich dieser Hinsicht keine Probleme. aktualisierten Yardsticksystem, das Regattasegeln mit baugleichen Aber auch für die übrigen Serienyachten ist der Standard durch De- Serienyachten und Jollentypen zu fördern. finition und Beschreibung im YS-Grundstandard verbindlich festge- Dabei sollen zeitlicher und finanzieller Vermessungsaufwand für legt. Für den Rumpf sind Kielform, ggf. -

Highlights from the Inverloch Classic Wooden Dinghy Regatta
The Inverloch Classic Wooden Dinghy Regatta The Inverloch Classic Wooden Dinghy Regatta is about displaying classic wooden sailing dinghies both on and off the water, many of which were once common but are now becoming rare. By focusing on the beauty of the wood crafting, rigging and history of these boats it is hoped people will appreciate them more fully and participate in their restoration and conservation. Over the Australia Day Weekend the Regatta also highlights aspects of Inverloch’s unique seaside history. Highlights from the Inverloch Classic Wooden Dinghy Regatta 26, 27 and 28 January 2017 March 2017 Newsletter South Gippsland Yacht Club Commodore What a fantastic weekend! Of course we were blessed with perfect weather conditions for a sailing event but to my mind it was the participants that made the regatta such a success. We had the most entrants of any year so far with forty seven boats lined up along the beach and looking out over Anderson Inlet at the start of the race on Friday, it was truly a spectacular sight. Many of the boats on view were here for the first time, among them the fleet of Sailfish whose owners proved to be a competitive bunch who really contributed to the atmosphere. It was an added bonus to have co-designer Jack Carroll in attendance and freely giving his time to anyone who wanted to talk about boats. With so many beautiful boats on display, the judging panel had some difficult decisions to make. It was a fitting reward and popular choice when Andrew Chapman was presented with the Best Boat award for his restoration of the Gwen 12 “Flyaway II”. -

Notice of Race
Australian Sharpie Sailing Association 78th Australian Championship 29 Dec 2020 – 4 Jan 2021 NOTICE OF RACE Organising Authority YMCA Sailing Club in conjunction with Australian Sharpie Sailing Association (NSW Division) Venue: Lake Burley Griffin, ACT The notation ‘[DP]’ in a rule in the NoR means that the penalty for a breach of that rule may, at the discretion of the protest committee, be less than disqualification. 1. Rules 1.1 The regatta will be governed by the rules as defined in The Racing Rules of Sailing (RRS) 2017- 2020. 1.2 Australian Sailing Prescriptions and Special Regulations Part 2-Off the Beach Boats will apply. It will be the responsibility of all competitors to ensure that personal flotation devices comply with a standard equivalent to those listed in Special Regulations 5.01 Personal Flotation Devices. 1.3 RRS 30.4 is changed by replacing “sail number” with “bow number”. The supplied bow number stickers are to be affixed to each side of the bow of each competing boat as prescribed in the sailing instructions. 1.4 (a) RRS 42.3(c) is changed in accordance with the Class Association By-Laws, Part B, Clause 20(1) to allow “On a free leg of the course when surfing (rapidly accelerating down the leeward side of a wave) or planning is possible, the Yacht’s crew may, in order to initiate surfing or planing, pump the sheet, boom or guy, controlling any sail a maximum of three (3) times for each wave or gust of wind.” b) Devices which indicate remotely or transmit or correlate data about wind direction, wind speed, boat speed or location shall be prohibited in accordance with the Class Association By-Laws, Part B, Clause 20(2).