Mombasa City Residents' Perception Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

County Urban Governance Tools
County Urban Governance Tools This map shows various governance and management approaches counties are using in urban areas Mandera P Turkana Marsabit P West Pokot Wajir ish Elgeyo Samburu Marakwet Busia Trans Nzoia P P Isiolo P tax Bungoma LUFs P Busia Kakamega Baringo Kakamega Uasin P Gishu LUFs Nandi Laikipia Siaya tax P P P Vihiga Meru P Kisumu ga P Nakuru P LUFs LUFs Nyandarua Tharaka Garissa Kericho LUFs Nithi LUFs Nyeri Kirinyaga LUFs Homa Bay Nyamira P Kisii P Muranga Bomet Embu Migori LUFs P Kiambu Nairobi P Narok LUFs P LUFs Kitui Machakos Kisii Tana River Nyamira Makueni Lamu Nairobi P LUFs tax P Kajiado KEY County Budget and Economic Forums (CBEFs) They are meant to serve as the primary institution for ensuring public participation in public finances in order to im- Mom- prove accountability and public participation at the county level. basa Baringo County, Bomet County, Bungoma County, Busia County,Embu County, Elgeyo/ Marakwet County, Homabay County, Kajiado County, Kakamega County, Kericho Count, Kiambu County, Kilifi County, Kirin- yaga County, Kisii County, Kisumu County, Kitui County, Kwale County, Laikipia County, Machakos Coun- LUFs ty, Makueni County, Meru County, Mombasa County, Murang’a County, Nairobi County, Nakuru County, Kilifi Nandi County, Nyandarua County, Nyeri County, Samburu County, Siaya County, TaitaTaveta County, Taita Taveta TharakaNithi County, Trans Nzoia County, Uasin Gishu County Youth Empowerment Programs in urban areas In collaboration with the national government, county governments unveiled -

Sediment Dynamics and Improvised Control Technologies in the Athi River Drainage Basin, Kenya
Sediment Dynamics in Changing Environments (Proceedings of a symposium held 485 in Christchurch, New Zealand, December 2008). IAHS Publ. 325, 2008. Sediment dynamics and improvised control technologies in the Athi River drainage basin, Kenya SHADRACK MULEI KITHIIA Postgraduate Programme in Hydrology, Department of Geography and Environmental Studies, University of Nairobi, PO Box 30197, 00100 GPO, Nairobi, Kenya [email protected] Abstract In Kenya, the changing of land-use systems from the more traditional systems of the 1960s to the present mechanized status, contributes enormous amounts of sediments due to water inundations. The Athi River drains areas that are subject to intense agricultural, industrial, commercial and population settlement activities. These activities contribute immensely to the processes of soil erosion and sediment transport, a phenomenon more pronounced in the middle and lower reaches of the river where the soils are much more fragile and the river tributaries are seasonal in nature. Total Suspended Sediments (TSS) equivalent to sediment fluxes of 13 457, 131 089 and 2 057 487 t year-1 were recorded in the headwater areas, middle and lower reaches of the river, respectively. These varying trends in sediment transport and amount are mainly due to the chemical composition of the soil coupled with the land-soil conservation measures already in practice, and which started in the 1930s and reached their peak in the early 1980s. This paper examines trends in soil erosion and sediment transport dynamics progressively downstream. The land-use activities and soil conservation, control and management technologies, which focus on minimizing the impacts of overland flow, are examined to assess the economic and environmental sustainability of these areas, communal societal benefits and the country in general. -

The Water Crisis in Kenya: Causes, Effects, and Solutions
Global Majority E-Journal, Vol. 2, No. 1 (June 2011), pp. 31-45 The Water Crisis in Kenya: Causes, Effects and Solutions Samantha Marshall Abstract Located on the eastern coast of Africa, Kenya, a generally dry country with a humid climate, is enduring a severe water crisis. Several issues such as global warming (causing recurrent and increasingly severe droughts as well as floods), the contamination of drinking water, and a lack of investment in water resources have enhanced the crisis. This article provides an overview of Kenya’s water crisis, along with a brief review of the literature and some empirical background. It reviews the main causes of the water crisis and how it affects the health of millions of Kenyans. Furthermore, the article summarizes some of the main solutions proposed to overcome the crisis. I. Introduction There are about 40 million people living in Kenya, of which about 17 million (43 percent) do not have access to clean water.1 For decades, water scarcity has been a major issue in Kenya, caused mainly by years of recurrent droughts, poor management of water supply, contamination of the available water, and a sharp increase in water demand resulting from relatively high population growth. The lack of rainfall affects also the ability to acquire food and has led to eruptions of violence in Kenya. In many areas, the shortage of water in Kenya has been amplified by the government’s lack of investment in water, especially in rural areas. Most of the urban poor Kenyans only have access to polluted water, which has caused cholera epidemics and multiple other diseases that affect health and livelihoods. -

469880Esw0whit10cities0rep
Report No. 46988 Public Disclosure Authorized &,7,(62)+23(" GOVERNANCE, ECONOMIC AND HUMAN CHALLENGES OF KENYA’S FIVE LARGEST CITIES Public Disclosure Authorized December 2008 Water and Urban Unit 1 Africa Region Public Disclosure Authorized Public Disclosure Authorized Document of the World Bank __________________________ This document has a restricted distribution and may be used by recipients only in the performance of their official duties. Its contents may not otherwise be disclosed without written authorization from the World Bank. ii PREFACE The objective of this sector work is to fill existing gaps in the knowledge of Kenya’s five largest cities, to provide data and analysis that will help inform the evolving urban agenda in Kenya, and to provide inputs into the preparation of the Kenya Municipal Program (KMP). This overview report is first report among a set of six reports comprising of the overview report and five city-specific reports for Nairobi, Mombasa, Kisumu, Nakuru and Eldoret. The study was undertaken by a team comprising of Balakrishnan Menon Parameswaran (Team Leader, World Bank); James Mutero (Consultant Team Leader), Simon Macharia, Margaret Ng’ayu, Makheti Barasa and Susan Kagondu (Consultants). Matthew Glasser, Sumila Gulyani, James Karuiru, Carolyn Winter, Zara Inga Sarzin and Judy Baker (World Bank) provided support and feedback during the entire course of work. The work was undertaken collaboratively with UN Habitat, represented by David Kithkaye and Kerstin Sommers in Nairobi. The team worked under the guidance of Colin Bruce (Country Director, Kenya) and Jamie Biderman (Sector Manager, AFTU1). The team also wishes to thank Abha Joshi-Ghani (Sector Manager, FEU-Urban), Junaid Kamal Ahmad (Sector Manager, SASDU), Mila Freire (Sr. -

Second Health Strategic and Investment Plan (Chsip Ii)
MOMBASA COUNTY of HealthDepartment Services SECOND HEALTH STRATEGIC AND INVESTMENT PLAN (CHSIP II) 2018 – 2022 A Healthy and Productive Community Abridged Version August 2018 CONTENTS CONTENTS ii ABBREVIATIONS iii LIST OF FIGURES v LIST OF TABLES 6 Foreword 7 Acknowledgment 8 Executive Summary 9 1 COUNTY INSTITUTIONAL REVIEW 1 1.1 About Mombasa County ........................................................................................................ 1 1.2 Population Demographics...................................................................................................... 3 1.3 County Health Sector............................................................................................................. 3 1.4 Purpose of the Second County Health Sector Strategic and Investment Plan (CHSIP II) 2018-2022 .............................................................................................................................. 4 1.5 County Performance Management Framework ..................................................................... 5 1.6 The Planning Process............................................................................................................. 6 1.7 Mission, Vision and Values ................................................................................................... 7 2 SITUATION ANALYSIS 8 2.1 Summary of County Health Sector Performance 2013/14 – 2017/18 ................................... 8 2.2 Situation Analysis ................................................................................................................. -
Flash Update
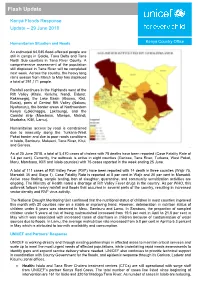
Flash Update Kenya Floods Response Update – 29 June 2018 Humanitarian Situation and Needs Kenya Country Office An estimated 64,045 flood-affected people are still in camps in Galole, Tana Delta and Tana North Sub counties in Tana River County. A comprehensive assessment of the population still displaced in Tana River will be completed next week. Across the country, the heavy long rains season from March to May has displaced a total of 291,171 people. Rainfall continues in the Highlands west of the Rift Valley (Kitale, Kericho, Nandi, Eldoret, Kakamega), the Lake Basin (Kisumu, Kisii, Busia), parts of Central Rift Valley (Nakuru, Nyahururu), the border areas of Northwestern Kenya (Lokichoggio, Lokitaung), and the Coastal strip (Mombasa, Mtwapa, Malindi, Msabaha, Kilifi, Lamu). Humanitarian access by road is constrained due to insecurity along the Turkana-West Pokot border and due to poor roads conditions in Isiolo, Samburu, Makueni, Tana River, Kitui, and Garissa. As of 25 June 2018, a total of 5,470 cases of cholera with 78 deaths have been reported (Case Fatality Rate of 1.4 per cent). Currently, the outbreak is active in eight counties (Garissa, Tana River, Turkana, West Pokot, Meru, Mombasa, Kilifi and Isiolo counties) with 75 cases reported in the week ending 25 June. A total of 111 cases of Rift Valley Fever (RVF) have been reported with 14 death in three counties (Wajir 75, Marsabit 35 and Siaya 1). Case Fatality Rate is reported at 8 per cent in Wajir and 20 per cent in Marsabit. Active case finding, sample testing, ban of slaughter, quarantine, and community sensitization activities are ongoing. -

Citizens' Perception of Leadership During COVID-19 Times in Mombasa, Kenya
Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya Fathima Azmiya Badurdeen To cite this version: Fathima Azmiya Badurdeen. Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya. 2020, https://mambo.hypotheses.org/2853. halshs-03078567 HAL Id: halshs-03078567 https://halshs.archives-ouvertes.fr/halshs-03078567 Submitted on 16 Dec 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Institut français de recherche en Afrique French Institute for Research in Africa MAMBO! XVII (4), 2020 COVID-19 Special Papers Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya Fathima AZMIYA BADURDEEN Cite: AZMIYA BADURDEEN, Fathima. 2020. Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya. Mambo! vol. XVII, no. 4. URL: https://mambo.hypotheses.org/2853 The author: Dr. Fathima Azmiya Badurdeen is a lecturer in Development Studies at the Department of Social Sciences, Technical University of Mombasa, working on issues related to youth, gender and violent extremism. The article is an outcome of the research funded by the French Institute for Research in Africa (IFRA) from April to September 2020. Email: [email protected]. -
CONFLICT SNAPSHOT Kenya December 2020 Introduction
Funded by the European Union CONFLICT SNAPSHOT Kenya December 2020 Introduction Kenya is a large culturally and ethnic diverse country, with over 40 different ethnic groups and numerous superimposed conflicts. Ethnic tensions and clashes coupled with political instability that manifests during the election period have been on the rise in the recent past. Recurrent drought that pushes herders into farmlands in search of pasture has led to violent clashes between herders and farmers in Garissa and Tana River counties. Ethnic group affiliation and highly centralised ethnopolitics are the primary identity of many Kenyans, especially during periods of turmoil. According to the Conflict Analysis of Kenya report, Kenyan Muslims have been marginalised within the Kenyan state and feel like they are treated as second-rate citizens. Data collection and analysis Data for the conflict snapshot COVID-19 series in Kenya was airoi gathered from 21-25 September in the following target zones: arissa This coincided with a period of relative calm in terms of ana iver COVID-19 caseloads and containment measures in Kenya, Kilifi as it fell in between the first and second wave of outbreaks omasa and many people believed there would soon be a return to normalcy. This perception may have influenced certain survey wale responses and we expect to see changes in this in the next round of snapshot reports. This report was prepared by the Search for Common Ground Kenya team, with support from Search’s COVID-19 Response Programming Team and Institutional Learning Team. For more information on the data collection methodology and tools used by Search for Common Ground for this research, click here. -

Mombasa County Crime and Violence Report
MOMBASA COUNTY CRIME AND VIOLENCE RAPID ASSESSMENT MOMBASA COUNTY CRIME AND VIOLENCE RAPID ASSESSMENT Cover photo credit: Andrea Albini | Creative Commons 3.0 Design and copy editing: Laura C. Johnson II Contents Foreword .................................................v Acknowledgements .........................................vi Acronyms ................................................vii 1 Introduction .............................................1 Crime and Violence Prevention in Kenya ...............................3 Crime and Violence Prevention Training ...............................4 County-Level Crime and Violence Prevention ..........................4 Framework for Analysis .............................................7 Goals of the Rapid Assessment ......................................9 Methodology . .9 2 Background: Crime and Violence Trends in Kenya ............13 Boda-Boda-Related Crime and Violence .............................14 Alcohol and Drug Abuse ...........................................14 Sexual and Gender-Based Violence ..................................16 Violence against Children ..........................................16 Radicalization and Recruitment into Violent Extremism ..................17 3 Rapid Assessment of Mombasa County .....................19 Overview of County ...............................................19 Cross-Cutting Drivers of Crime and Violence ..........................20 Dynamics of Crime and Violence ....................................23 Security Interventions .............................................40 -

(Nema)Table of Contents
ENVIR ONMENTAL AND SOCIAL IMPACT ASSESSMENT REPORT (ESIA) AND RESETLEMENT ACTION PLAN (RAP) FOR THE PROPSED MALINDI AIRPORT RUNWAY EXPANSION PROJECT TENDER NO. KAA/OT/MLD/1507/2018/2019 NOVEMBER, 2020 KENYA AIRPORTS AUTHORITY ESIA and RAP report for the proposed Extension of Malindi Airport Runway CERTIFICATION This ESIA study report has been prepared in accordance with the Environmental Management and Coordination Act (EMCA) 1999 and the Environmental (Impact Assessment and Audit) Regulations 2003 for submission to the National Environment Management Authority (NEMA). The following experts conducted the study and prepared this report on behalf of Eco-solutions Limited: FOR Eco Solutions Limited, iPlan Consult (Int’l) Limited, P.O. BOX 20492 – 00100, P.O BOX 28634-00100 NAIROBI, KENYA. NAIROBI. TEL: +254 722 273935. TEL: +254 721891005. Email: [email protected] Email: [email protected] Name Designation NEMA Date & Signature REG. NO. 1. SHADRACK K. MBUTA EIA LEAD EXPERT 6315 2. WALLACE ISABOKE EIA LEAD EXPERT 2622 3. CYNTHIA OTARA ASS. EXPERT 11450 The Proponent; Kenya Airports Authority (KAA), P.O. Box 19001-00501, Nairobi. Signature___________________________ Date_____________________________ Designation: Environment Manager Disclaimer: This ESIA Report is confidential to Kenya Airports Authority (KAA), and any use of the materials hereof should be strictly in accordance with the contractual agreement between Eco-solutions and Kenya Airports Authority (KAA). It is, however, subject to conditions spelt out in the Environmental (Impact Assessment and Audit) Regulations, 2003. Eco Solutions Ltd; iPlan Consult (Int’l) Limited November 2020 2 KENYA AIRPORTS AUTHORITY ESIA and RAP report for the proposed Extension of Malindi Airport Runway EXECUTIVE SUMMARY 1. -

Out Patient Facilities for Nhif Supa Cover Baringo County Bomet County Bungoma County Busia County
OUT PATIENT FACILITIES FOR NHIF SUPA COVER BARINGO COUNTY BRANCH No HOSPITAL NAME POSTAL ADDRESS OFFICE 1 TIONYBEI MEDICAL CLINIC 396-30400, KABARNET KABARNET 2 BARINGO DISTRICT HOSPITAL (KABARNET) 21-30400, KABARNET KABARNET 3 REALE MEDICAL CENTRE-KABARNET 4694-30100, ELDORET KABARNET 4 KERIO HOSPITAL LTD 458-30400, KABARNET KABARNET 5 RAVINE GLORY HEALTH CARE SERVICES 612-20103, ELDAMA RAVINE KABARNET 6 ELDAMA RAVINE NURSING HOME 612-20103, ELDAMA RAVINE KABARNET 7 BARNET MEMORIAL MEDICAL CENTRE 490-30400, KABARNET KABARNET BOMET COUNTY BRANCH No HOSPITAL NAME POSTAL ADDRESS OFFICE 1 CHELYMO MEDICAL CENTRE 37-20422 SILIBWET BOMET 2 KAPKOROS HEALTH CENTRE 20400 BOMET BOMET BUNGOMA COUNTY BRANCH No HOSPITAL NAME POSTAL ADDRESS OFFICE 1 CHWELE SUBCOUNTY HOSPITAL 202 - 50202 CHWELE BUNGOMA 2 LUMBOKA MEDICAL SERVICES 1883 - 50200 BUNGOMA BUNGOMA 3 WEBUYE HEALTH CENTRE 25 - WEBUYE BUNGOMA 4 ST JAMES OPTICALS 2141 50200 BUNGOMA 5 NZOIA MEDICAL CENTRE 471 - 50200 BUNGOMA BUNGOMA 6 TRINITY OPTICALS LIMITED PRIVATE BAG BUNGOMA BUNGOMA 7 KHALABA MEDICAL SERVICES 2211- 50200 BUNGOMA BUNGOMA 8 ARARAT MEDICAL CLINIC 332 KIMILILI BUNGOMA 9 SIRISIA SUBDISTRICT HOSPITAL 122 - 50208 SIRISIA BUNGOMA 10 NZOIA MEDICAL CENTRE - CHWELE 471 - 50200 BUNGOMA BUNGOMA 11 OPEN HEART MEDICAL CENTRE 388 - 50202 CHWELE BUNGOMA 12 ICFEM DREAMLAND MISSION HOSPITAL PRIVATE BAG KIMILILI BUNGOMA 13 EMMANUEL MISSION HEALTH CENTRE 53 - 50207 MISIKHU BUNGOMA 14 WEBUYE DISTRICT HOSPITAL 25 - 50205 BUNGOMA 15 ELGON VIEW MEDICAL COTTAGE 1747 - 50200 BUNGOMA BUNGOMA 16 FRIENDS -

County Name County Code Location
COUNTY NAME COUNTY CODE LOCATION MOMBASA COUNTY 001 BANDARI COLLEGE KWALE COUNTY 002 KENYA SCHOOL OF GOVERNMENT MATUGA KILIFI COUNTY 003 PWANI UNIVERSITY TANA RIVER COUNTY 004 MAU MAU MEMORIAL HIGH SCHOOL LAMU COUNTY 005 LAMU FORT HALL TAITA TAVETA 006 TAITA ACADEMY GARISSA COUNTY 007 KENYA NATIONAL LIBRARY WAJIR COUNTY 008 RED CROSS HALL MANDERA COUNTY 009 MANDERA ARIDLANDS MARSABIT COUNTY 010 ST. STEPHENS TRAINING CENTRE ISIOLO COUNTY 011 CATHOLIC MISSION HALL, ISIOLO MERU COUNTY 012 MERU SCHOOL THARAKA-NITHI 013 CHIAKARIGA GIRLS HIGH SCHOOL EMBU COUNTY 014 KANGARU GIRLS HIGH SCHOOL KITUI COUNTY 015 MULTIPURPOSE HALL KITUI MACHAKOS COUNTY 016 MACHAKOS TEACHERS TRAINING COLLEGE MAKUENI COUNTY 017 WOTE TECHNICAL TRAINING INSTITUTE NYANDARUA COUNTY 018 ACK CHURCH HALL, OL KALAU TOWN NYERI COUNTY 019 NYERI PRIMARY SCHOOL KIRINYAGA COUNTY 020 ST.MICHAEL GIRLS BOARDING MURANGA COUNTY 021 MURANG'A UNIVERSITY COLLEGE KIAMBU COUNTY 022 KIAMBU INSTITUTE OF SCIENCE & TECHNOLOGY TURKANA COUNTY 023 LODWAR YOUTH POLYTECHNIC WEST POKOT COUNTY 024 MTELO HALL KAPENGURIA SAMBURU COUNTY 025 ALLAMANO HALL PASTORAL CENTRE, MARALAL TRANSZOIA COUNTY 026 KITALE MUSEUM UASIN GISHU 027 ELDORET POLYTECHNIC ELGEYO MARAKWET 028 IEBC CONSTITUENCY OFFICE - ITEN NANDI COUNTY 029 KAPSABET BOYS HIGH SCHOOL BARINGO COUNTY 030 KENYA SCHOOL OF GOVERNMENT, KABARNET LAIKIPIA COUNTY 031 NANYUKI HIGH SCHOOL NAKURU COUNTY 032 NAKURU HIGH SCHOOL NAROK COUNTY 033 MAASAI MARA UNIVERSITY KAJIADO COUNTY 034 MASAI TECHNICAL TRAINING INSTITUTE KERICHO COUNTY 035 KERICHO TEA SEC. SCHOOL