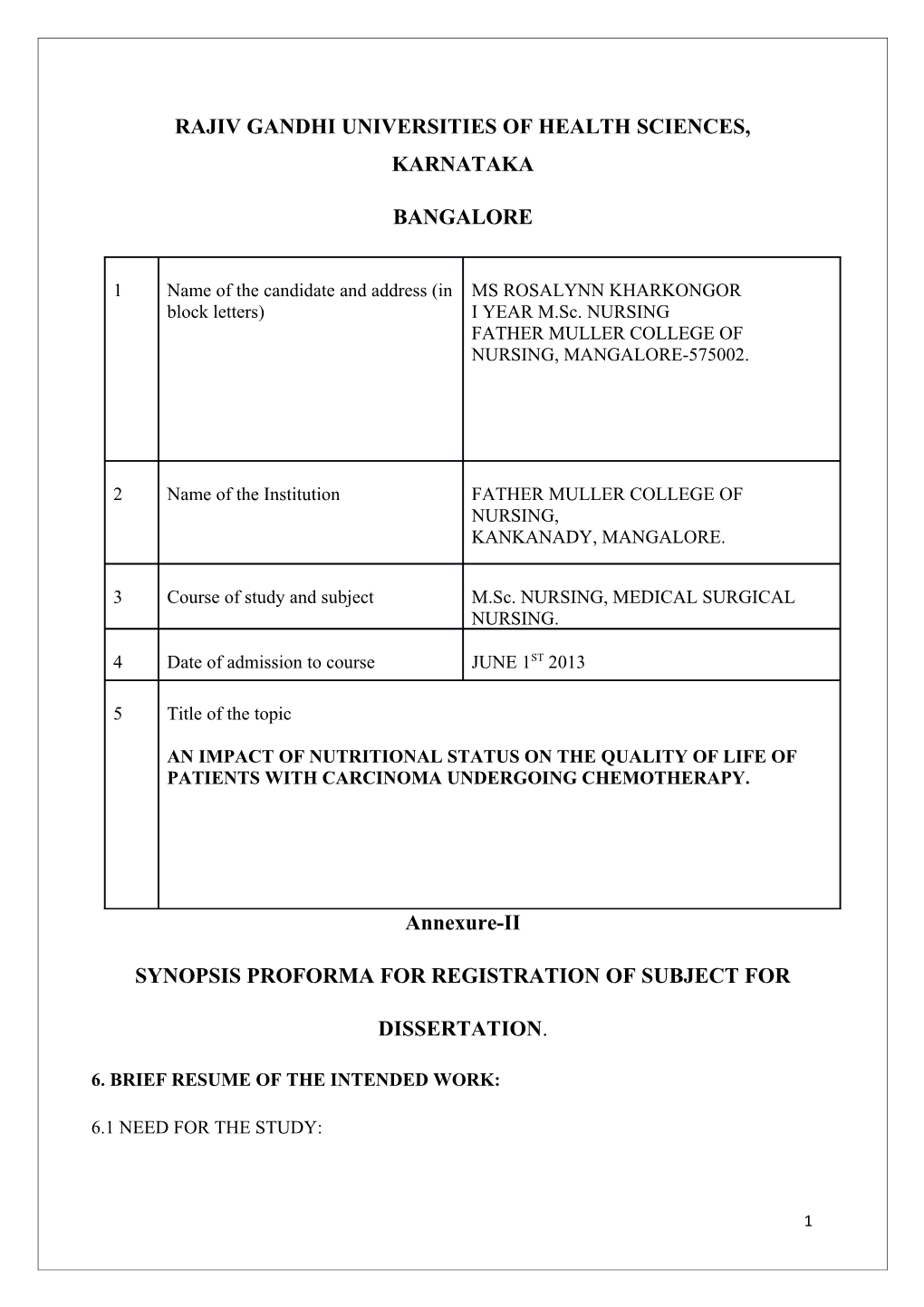
RAJIV GANDHI UNIVERSITIES OF HEALTH SCIENCES, KARNATAKA
BANGALORE
1 Name of the candidate and address (in MS ROSALYNN KHARKONGOR block letters) I YEAR M.Sc. NURSING FATHER MULLER COLLEGE OF NURSING, MANGALORE-575002.
2 Name of the Institution FATHER MULLER COLLEGE OF NURSING, KANKANADY, MANGALORE.
3 Course of study and subject M.Sc. NURSING, MEDICAL SURGICAL NURSING.
4 Date of admission to course JUNE 1ST 2013
5 Title of the topic
AN IMPACT OF NUTRITIONAL STATUS ON THE QUALITY OF LIFE OF PATIENTS WITH CARCINOMA UNDERGOING CHEMOTHERAPY.
Annexure-II
SYNOPSIS PROFORMA FOR REGISTRATION OF SUBJECT FOR
DISSERTATION.
6. BRIEF RESUME OF THE INTENDED WORK:
6.1 NEED FOR THE STUDY:
1 Cancer is a major public health problem worldwide. It is projected that by the year 2020, cancer incidence will be double worldwide. Nutrition and diet plays a major role in cancer. Dietary factors are an important component of the identifiable risk of cancer, malnutrition is a cause of some of the significant clinical signs and symptoms that are observed in patients with cancer and nutrition status is an important prognostic factor in patients with cancer. Malnutrition and weight loss often contribute to the deaths of patients with cancer.1
Malnutrition is a possible complication in patients with cancer and can be the first symptomsto reveal the presence of the disease. Even before starting anti-cancer treatment, patients can experience profound metabolic and physiological alterations with increased needs of macro- and micronutrients.2Malnutrition among cancer patients is very common; with an estimated incidence of approximately 40 to 80%.Local incidence of malnutrition is estimated to be around 47.7%. Cancer patients undergo metabolic alterations, which render them to have protein energy malnutrition throughout all stages of the disease. Malnutrition globally impacts all cancer patients by increasing the risk of infection, delaying wound healing and increasing treatment toxicity, prolonging hospital stay and increasing health related costs.3 Malnutrition is also associated with poor response to therapy, increased susceptibility to treatment-related adverse events, as well as poor outcome and quality of life.4Malnutrition impairs the immune status and reduces the body’s defence against infectious diseases. In addition, malnutrition is an independent risk factor for quality of life.2 In light of these possible complications; malnutrition represents a poor prognostic factor and should be prevented or detected as early as possible.5
According to the National Cancer Institute, an astounding 20% to 40% of cancerpatients die from causes related to malnutrition, not from the cancer itself, and 80% of cancer patients develop some form of clinical malnutrition.6 Another article in the NBCNEWS headlines “Push to Fight Malnutrition in Cancer patients” remarks that the statistic shown is shocking: Severe malnutrition and weight loss play a role in at least one in five cancer deaths.7 The various complications caused by cancer can affect patients’ quality of life in many domains: physical (pain, sleep disturbances, loss of appetite, fatigue, activities of daily living), social, psychological (depression, anxiety), and work-related.8,9 Nutritional related symptoms, such as anorexia and weight loss, reflect impaired nutritional status which is often associated with reduced Quality of life.10 A study conducted on the relationship between nutritional status and quality of life in patients with cancer shows that a significant association with weight was observed for the main dimensions of the quality of life: physical, functional, cognitive, social, fatigue, nausea, pain, loss of appetite, constipation and diarrhoea. This strong relation between quality of life and weight loss shows the importance of dietary management in patients with cancer.11
Presently in India, an estimated nearly one million new cancer cases are being detected annually in the country. For patients and their family, a diagnosis of cancer brings challenges to many aspects of daily life, with a major concern being maintaining the highest quality of life possible during and after the experience.12
Therefore the proposed study is pertinent to the needs of the patient. Early intervention with nutritional supplementation has been shown to halt malnutrition, and may improve outcome in some patients. As a matter of fact, cancer patients prefer to trade off months of survival if this is associated with a better quality of life.
6.2 REVIEW OF LITERATURE:
3 A prospective study was done in Australia to assess the nutritional status and quality of life of ambulatory patients receiving radiation therapy to the head, neck, rectal or abdominal. The results showed 65.0% of subjects were well-nourished, 28.3% moderately or suspected of being malnourished and 6.7% severely malnourished. There was a correlation between change in nutritional status (PG-SGA score) and change in QoL after 4 weeks of radiotherapy (r=-0.55, P<0.001). Regression analysis determined that 26% of the variation of change in QoL was explained by change in PG-SGA (P=0.001).13
Another study conducted at AIIMS, New Delhi, India on the effect of change in symptoms, respiratory status, nutritional profile and quality of life on response to treatment for advanced non-small cell lung cancer reported that overall, chemotherapy caused significant decline in the frequency of coughing, dyspnea, chest pain, fever, anorexia, weight loss, and improvement in haemoglobin and albumin levels. However, there was no significant improvement in pulmonary functions, nutritional status, or QOL scores after treatment. Therefore management of non-small cell lung cancer (NSCLC) must include strategies to improve various aspects of QOL, nutritional status and pulmonary reserve to achieve comprehensive benefit.14
In yet another study conducted in the medical oncology clinic of a tertiary care hospital of South India with an aim to assess the QOL of cancer patients receiving chemotherapy for different types of cancer showed that 80% of the total study population reported to have average and below average QOL.12
A descriptive study, conducted at Manipal and Mangalore, Karnataka, India on the quality of life of head, and neck cancer patients receiving cancer –specific treatments shows that quality of life was poor among 30%of thesubject and 65% had KPS scores of <85%. Physical, psychosocial and spiritual domains of quality of life and functional status were affected withhead, and neck cancer (HNC). The impact of one domain area of well -being, significantly affects the other domains of quality of life and there is a relationship between the performance status and the quality of life.15
Across-sectional study was conducted among cancer patients admitted for chemotherapy at the National Kidney and Transplant Institute-Cancer Unit, Oman from January to May 2011. According to the Subjective Global Assessment, there were 58 patients with SGA A, classified to have adequate nutrition and 39 patients (40.21%) were considered malnourished. Among these 39 patients, 32 were classified SGA-B (moderately malnourished) and 7 were classified SGA C (severely malnourished) mean global quality of life was 68.73 ± 19.05.Whenstatistically analysed, the results revealed that patients were statistically different across the Subjective Global Assessment groups according to global quality of life.3
Another study was done in wards in hospitals in Clermont-Ferrand and Saint Etienne, Belgium to describe the global quality of life and its various dimensions in patients with cancer, as a function of the nutritional status. The mean global quality of life score was 48.8 for patients who had a weight loss of more than 10% since the beginning of their illness, compared with 62.8 for the other patients. A significant association with weight was observed for the main dimensions of the quality of life: physical, functional, cognitive, social, fatigue, nausea, pain, loss of appetite, constipation and diarrhoea. This strong relation between quality of life and weight loss shows the importance of dietary management in patients with cancer.11
In a study to assess the prevalence of malnutrition and its grade among patients admitted in a mixed intensive care unit (ICU) of a tertiary care hospital in South India, 39.6% patients were malnourished, including one patient qualifying as severely malnourished. Hypertension, diabetes, and cancer were the three most commonly encountered co- morbidities among the malnourished. A total of 86% of all cancer patients admitted were malnourished against only 12% of trauma patients. Around 77% male cancer patients were moderately malnourished and 21% female cancer patients were moderately malnourished, while equal numbers of male and female patients (50%) were well nourished. Among the co- morbidities, malnutrition risk was highest among cancer patients, followed by CKD, CLD, and hypothyroidism.16
6.3 STATEMENT OF THE PROBLEM:
A study to assess the Impact of Nutritional status on the Quality of life among patients with Carcinoma undergoing Chemotherapy in a selected hospital atMangalore in a view to develop an information booklet.
6.4 OBJECTIVES OF THE STUDY: 1) To assess the nutritional status of patients with carcinoma undergoing chemotherapy.
5 2) To assess the quality of life of the patients with carcinoma undergoing chemotherapy
3) To determine the relationship between the nutritional status and the quality of life among patients with carcinoma undergoing chemotherapy.
4) To determine the association between nutritional status, quality of life and selected baseline variable.
6.5 OPERATIONAL DEFINITION:
Impact
The powerful effect that something has on something or somebody.17
In this study, impact refers to the effect of nutritional status on the quality of life among the patients with carcinoma undergoing chemotherapy as measured by nutritional status assessment scale and quality of life scale.
Nutritional status
The state of the body in relation to the consumption and utilisation of nutrients.18
In this study, it refers to the state of the body in relation to the consumption and utilisation of nutrients among the patients with carcinoma undergoing chemotherapy as measured by nutritional status scale.
Quality of life
Quality of life is the subjective evaluation of the good and satisfactory character of life as a whole.19
In the study, quality of life is the patient’s perspective on their ability to live useful, meaningful, fulfilling lives even when burden with disease as measured with quality of life scale.
Patients with carcinoma
Carcinoma is a type of cancer (an uncontrolled division of abnormal cells in a part of the body) originating from ectoderm.20 In this study, it refers to the patient diagnosed with carcinoma undergoing chemotherapy.
Information booklet
A booklet where information is printed and illustrated in a simple way.
In this study, Information booklet is a booklet where information is given about the diet that the patient can have according to their nutritional status.
6.6 ASSUMPTION:
1. Patients with carcinoma undergoing chemotherapy will have poor nutritional status.
2. The nutritional status has an impact on the quality of life.
3. Information on nutritious diet helps in improving nutritional status.
6.7 DELIMITATIONS:
1. Patients admitted at Father Muller Medical College Hospital, Mangalore.
2. Patients with carcinoma receiving chemotherapy.
6.8 HYPOTHESES:
H1: There will bea significant relationship between the nutritional status and the quality of life of the patients with carcinoma undergoing chemotherapy.
H2: There will be significant association between the nutritional status and the selected baseline variable.
H3: There will be significant association between the quality of life and the selected baseline variable.
7. MATERIALS AND METHOD:
7.1 SOURCE OF DATA:
7.1.1 Research design: A descriptive correlational research design.
7 7.1.2 Setting: The data will be collected from the various Wards of Father Muller Medical College Hospital, Mangalore.
7.1.3 Population: The population includes the patients with carcinoma undergoing chemotherapy.
7.2 METHOD OF COLLECTION OF DATA:
7.2.1 Sampling procedure: the sampling procedure will be Purposive sampling.
7.2.2 Sample size: 75 patientswith carcinoma undergoing chemotherapy and who fulfils the sampling criteria.
7.2.3 Inclusion criteria:
i. Patients with Stage I to Stage IIIcarcinoma undergoing chemotherapy.
ii. Patients who can read and write Kannada or English.
7.2.4 Exclusion criteria:
i. Patients who are non-ambulatory.
ii. Patients who are critically ill during the time of study.
iii. Patients with oral, oesophagus and Gastro-Intestinal Tract carcinoma.
7.2.5 Instrument intended to be used:
Part I- A demographic profile proforma.
Part II- A weighing machine and a measuring tape.
Part III- A nutritional status assessment scale.
Part IV- A quality of life assessment scale.
7.2.6. Data collection method: Data will be collected from subjects fulfilling the inclusion criteria. Written consent will be obtained from each subject before the study. Weight and height of these patients will be measured. A nutritional status assessment scale and the quality of life scale for assessing the nutritional status and the quality of life will be given.
7.2.7. Data analysis plan:
Descriptive statistics:
Baseline data, nutritional status and quality of life would be analysed in terms of frequency, percentage, mean and standard deviation and would be presented in the form of tables and diagrams.
Inferential statistics:
Chi –Square test will be used to determine the association between nutritional status, quality of life and the demographic variable.
Pearson’s correlation will be used to establish the correlation between the nutritional status, quality of life and the demographic variable.
7.3 DOES THE STUDY REQUIRE ANY INVESTIGATION OR interventions to be
conducted on patients or other human or animals? If so, please describe briefly.
Yes, investigations will done on the patient.Weight and height of the patients will be measured to calculate the BMI. A nutritional status assessment scale and the quality of life scale for assessing the nutritionalstatus and the quality of life will be given to these patients.
7.4 HAS ETHICAL CLEARANCE BEEN FROM YOUR INSTITUTE IN CASE OF 7.3?
Yes.
9 8. REFERENCES:
1. Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR(editors). Modern nutrition in health and diseases. 11thed. Philadelphia:Lippincott Williams and Wilkins,a Wolters and Kluwerbusiness; 2014.
2. Alexandre J, Goupil MG, Falssard B, et al. Evaluation of the nutritional and inflammatory status in cancer patients for the risk assessment of severe haematological toxicity following chemotherapy. Ann Oncol [serial online] 2003 [cited 2013 Oct 26]:14:36-41.
Available from: URL:http://www.ncbi.nlm.nih.gov/pubmed/12488290.
3. Vergara N, Montoya JE, Luna HG, Amparo JR, and Luna GC. Quality of life and nutritional status among cancer patients on chemotherapy. Oman Med J [serial online] 2013 July [cited 2013 Oct 26];28(4):270–274.
Available from: URL:http://www.ncbi.nlm.nih.gov/pmc/articles/pmc 3725251.
4. Argiles GM.Cancer-associated malnutrition. Eur J Oncol Nurs [serial online] 2005 [cited 2013 Oct 15];9Suppl 2:S39-50. Available from: URL:http://www.ncbi.nlm.nih.gov/pubmed
5. Andreyev HJ. Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies? Eur J Cancer [serial online] 1998 [cited on 2013 Oct 27];34:503–509.
Available from: URL:http://www.ncbi.nlm.nih.gov/pubmed/9713300.
6. Fighting malnutrition among cancer patients;19 July 2007-1:00 PDT
Available from:URL:http://www.ABCnews.com/PubMed/18467087
7. Push to fight malnutrition in cancer patients; updated Oct 16, 2013.
Available from: URL:http://www.nbcnews.com/id/34696916/?q=cancer%20patient.
8. Campbell KL, Ash S, Davies PS, Bauer JD. Randomized controlled trial of nutritional counseling on body composition and dietary intake in severe CKD. Am J Kidney Dis [serial online] 2008 [cited 2013 Oct 27];51(5):748–758.
Available from: URL;http://www.ncbi.nlm.nih.gov/pubmed/18436085.
9. Das P, Cantor SB, Parker CL, Zampieri JB, Baschnagel A, Eng C, et al. Long-term quality of life after radiotherapy for the treatment of anal cancer. Cancer [serial online] 2010 Feb 15 [cited 2013 Oct 27];16(4):822–829.
Available from: URL:http://www.ncbi.nlm.nih.gov/pubmed/20041481.
10. Caro MMM, Laviano A, Pichard C. Impact of nutrition on quality of life during cancer. CurrOpinClinNutrMetab Care 2007;10:480-87.Lippincott Williams and Wilkins.
11. Nourissat A, Vasson MP, Merrouche Y, Bouteloup C, Goutte M, Mille D, etal. Relationship between nutritional status and quality of life in patients with cancer. Eur J Cancer[serial online] 2008 Jun [cited 2013 Oct 20];44(9):1238- 42.
Available from: URL:http://www.ncbi.nlm.nih.gov/pubmed/18467087.
12. Kannan G, Rani V, Ananthanarayanan RM, Palani T, Nigam N, Janardhan V, Reddy UM. Assessment of quality of life of cancer patients in a tertiary care
11 hospital of South India. J Can Res Ther [serial online] 2011[cited 2013 Oct 26];7: 275-9.
Available from: URL: http://www.cancerjournal.net/text.asp?2011/7/3/275/87013.
13. Isenring E, Bauer J, Capra S. The scored Patient-generated Subjective Global Assessment (PG-SGA) and its association with quality of life in ambulatory patients receiving radiotherapy.Eur J ClinNutr[serial online] 2003 Feb [cited on 2013 Oct 15];57(2):305-9.
Available from: URL:http://www.ncbi.nlm.nih.gov/pubmed/1257664.
14. Mohan A, Singh P, Kumar S, Mohan C, Pathak AK, Pandey RM, Guleria R.
Effect of change in symptoms, respiratory status, nutritional profile and quality of life on response to treatment for advanced non-small cell lung cancer.Asian Pac J Cancer Prev [serial online] 2008 Oct-Dec [cited 2013 Oct 26];9(4):557-62.
Available from: URL: http:// www.ncbi.nlm.nih.gov/p ubmed/19256738
15. DSouza PJJ, Chakrabarty J, Sulochana B, Gonsalves J. Quality of life of head and
neck cancer patients receiving cancer specific treatments. JKIMSU [serial online] 2013 Jan-June [cited 2013 Oct 26];2(1):112-5.
16. Chakravarty C, HazarikaB,GoswamiL and RamasubbanS. Prevalence of malnutrition in tertiary care hospital in India. Indian J.Crit.Care.Med[serial online] 2013 May-Jun [cited 2013 Oct 26];17(3):170-73.
Available from: URL:http://www.ncbi.nlm.nih.gov/pmc/articles/pmc 3777371/.
17. Hornby AS. New Oxford Advanced Learner’s Dictionary.7th ed. UK:Oxford
University Press; 2005.
18. Encyclopedia of medical terms: nutritional status. Available from: URL:http://reference.md/files/D009/mD009752.html. (Accessed on 2013 Nov 8).
19. Vankrippenberg FC, Dehaes JC. Measuring the quality of life of cancer patients:psychometric properties of instruments. J ClinEpidemiol[serial online] 1988 [cited 2013 Oct 27];41:1043-1053.
Available from: URL:http://www.ncbi.nlm.nih.gov/pubmed/3060569.
20. Chintamani, editor. Lewis’s: medical surgical nursing-assessment and management of clinical problems.7th ed. New Delhi:Elsevier; 2011.
13 9. SIGNATURE OF THE CANDIDATE:
10. REMARKS OF THE GUIDE:
11. NAME AND DESIGNATION OF:
11.1 GUIDE MRS PREETHI FERNANDES, ASSISTANT PROFESSOR MEDICAL SURGICAL NURSING.
11.2 SIGNATURE
11.3HEAD OF THE DEPARTMENT. MRS VICTORIA D’ALMEIDA, HEAD OF DEPARTMENT MEDICAL SURGICAL NURSING.
11.4 SIGNATURE:
12.1 REMARKS OF THE CHAIRMAN / PRINCIPAL 12.2 SIGNATURE
15