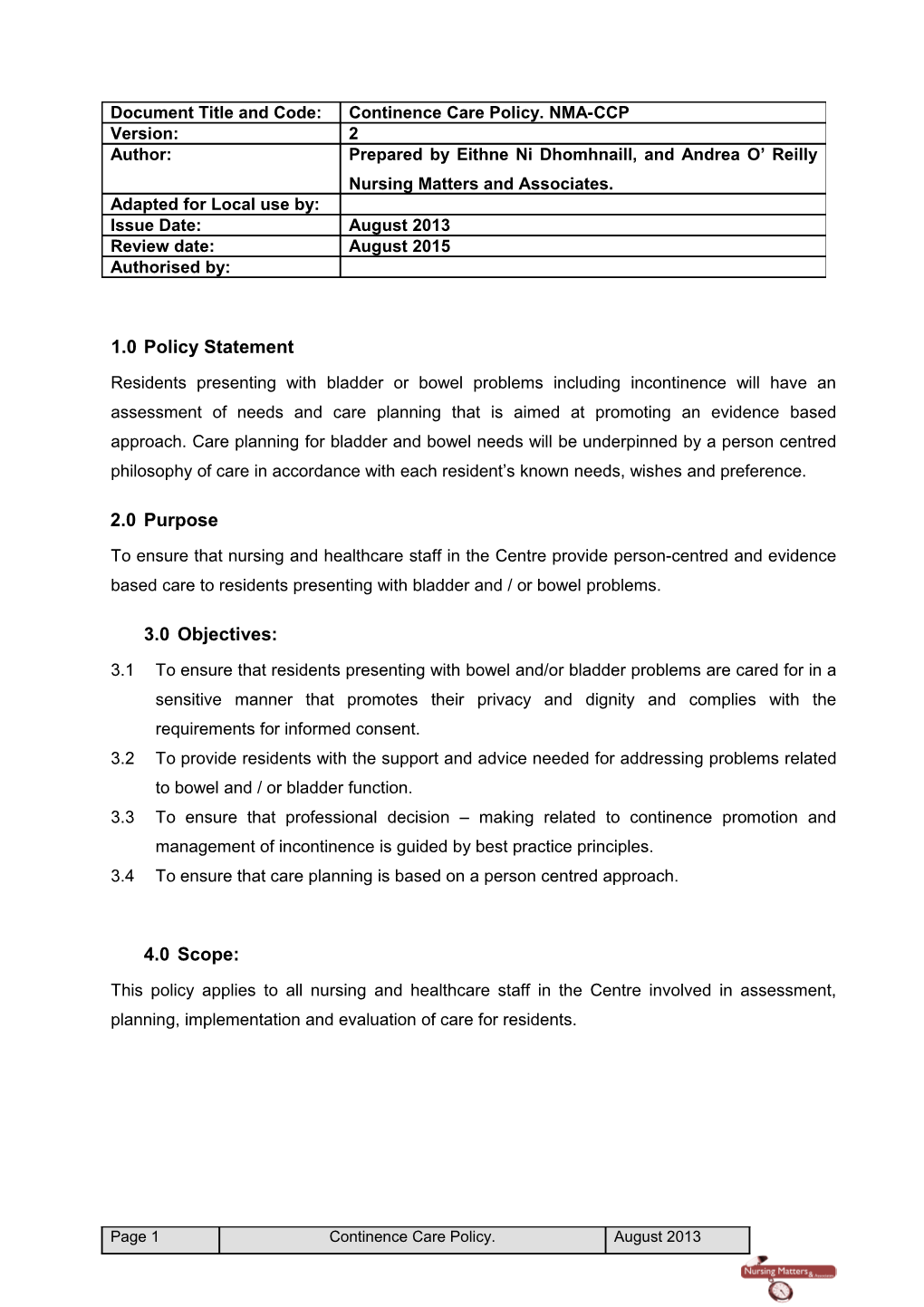
Document Title and Code: Continence Care Policy. NMA-CCP Version: 2 Author: Prepared by Eithne Ni Dhomhnaill, and Andrea O’ Reilly Nursing Matters and Associates. Adapted for Local use by: Issue Date: August 2013 Review date: August 2015 Authorised by:
1.0 Policy Statement
Residents presenting with bladder or bowel problems including incontinence will have an assessment of needs and care planning that is aimed at promoting an evidence based approach. Care planning for bladder and bowel needs will be underpinned by a person centred philosophy of care in accordance with each resident’s known needs, wishes and preference.
2.0 Purpose
To ensure that nursing and healthcare staff in the Centre provide person-centred and evidence based care to residents presenting with bladder and / or bowel problems.
3.0 Objectives:
3.1 To ensure that residents presenting with bowel and/or bladder problems are cared for in a sensitive manner that promotes their privacy and dignity and complies with the requirements for informed consent. 3.2 To provide residents with the support and advice needed for addressing problems related to bowel and / or bladder function. 3.3 To ensure that professional decision – making related to continence promotion and management of incontinence is guided by best practice principles. 3.4 To ensure that care planning is based on a person centred approach.
4.0 Scope:
This policy applies to all nursing and healthcare staff in the Centre involved in assessment, planning, implementation and evaluation of care for residents.
Page 1 Continence Care Policy. August 2013 5.0 Definitions:
5.1 Continence: is defined as ‘having the ability to store urine in the bladder and to excrete voluntarily and comfortably where and when it is socially appropriate’ (Feneley 1979) 5.2 Transient incontinence: Appears suddenly, is present for six months or less and is usually caused by reversible / treatable conditions (Sprecht, 2005). 5.3 Urge incontinence: refers to involuntary urination that happens soon after the resident feels an urgent need to void. It is characterised by the resident by an inability to suppress the urge to void resulting in loss of urine before the resident gets to the toilet. It is the most common type of urinary incontinence in older adults (Sprecht, 2005). 5.4 Stress incontinence: ‘involuntary urine leakage on effort or exertion, or on sneezing or coughing. Associated with short urethras and poor pelvic floor muscle tone in women. In men it is associated with prostate surgery and radiation (Queensland Government, 2007; Sprecht, 2005)). 5.5 Overflow incontinence: Involuntary loss of urine resulting from an over distension of the bladder resulting in frequent release of small amounts of urine usually in the form of dribbling. It is associated with obstruction of the urethra by faecal impaction or an enlarged prostate; smooth muscle relaxants or an impaired ability to contract as a result of peripheral neuropathy or neurological disease (Sprecht, 2005). 5.6 Constipation: a decrease in the frequency of passage of formed stools and characterized by stools that are hard and difficult to pass (McMillan, 2004). 5.7 Faecal overflow incontinence is leakage of loose stool around impacted faeces. Small quantities of stool are passed frequently and without sensation. It is also known as bypass soiling (Hyman et al, 2006). 5.8 Functional incontinence: The inability to reach the toilet because of environmental barriers; physical limitations and / or cognitive impairment (Sprecht, 2005). 5.9 Mixed incontinence: Involuntary loss of urine having features of two or more types of incontinence, usually a combination of stress and urge incontinence (Sprecht, 2005). 5.10 Reflex incontinence: Bladder empties automatically without the sensation to void eg. in spinal cord injuries. 5.11 Total incontinence: Refers to a continuous and unpredictable loss of urine resulting from surgery, trauma or a malformation such as ectopic ureter. Urination cannot be controlled because of anatomical abnormalities (Sprecht, 2005). 5.12 Catheter: A hollow tube inserted into a body organ / cavity to remove or instil fluid. Urinary catheters are designed for insertion into the bladder, either on an intermittent or constant basis for the purpose of draining urine from the bladder or for the instillation of medication (Pomfrey, 2000).
Page 2 Continence Care Policy. August 2013 5.13 Intermittent Catherisation (IC) involves the episodic introduction of a catheter into the bladder to drain any residual urine where normal voiding is not possible, and then the removal of the catheter leaving the client catheter free between catherisations. (Dougherty and Lister, 2004). 5.14 Clean Intermittent Catheterisation is a clean procedure involving the cleansing of the urethral meatus with soap and water and or disposable wipes (Dougherty and Lister, 2004). 5.15 Polyuria: Refers to an excessive urine output of either a 24hr urine output of more than 40ml/Kg. body weight or a urine output of more than 2,500mls in 24 hours. Causes of polyuria include: Habitual excess fluid intake. Diabetes Mellitus. Diabetes Insipidus. Hypercalcaemia. (Queensland Government, 2007) 5.16 Nocturia: The complaint of waking one or more times to void even if the urge to void is not perceived as the reason for waking, where this would not be the usual pattern for the resident. A common cause is nocturnal polyuria. (Queensland Government, 2007) 5.17 Nocturnal Polyuria: Nocturnal polyuria is present when 6.0 The total 24 hour urine volume is normal and a. The total volume of all night time voids and first morning void id greater than 33% of the total 24 hour output. (Queensland Government, 2007)
Page 3 Continence Care Policy. August 2013 7.0 Bladder and Bowel Care Quick Reference Guide.
Admission: Screening for Bladder/Bowel Problems. Ask the resident / representative if the resident has any difficulties or urgency with the functions of their bladder or bowel eg. ‘ have you any difficulties or urgency with your bladder or bowel function?’ Complete a screening assessment of bladder and bowel function to include: Establish usual elimination patterns. Perform urinalysis Red Flag Findings. Pain Based on initial assessment observe for / note any ‘red flag’ factors Recent unexplained weight and refer to resident’s general practitioner if ‘red flag’ present. loss. If bowel or bladder problems present, commence comprehensive Recent sudden changes in assessment. bowel habit. Document any problems and needs in the resident’s care plan and Rectal bleeding. communicate to care team. Persistent diarrhoea. Blood in urine visible to the naked eye. Comprehensive Assessment of Bladder or Bowel problems Haematuria. present. Symtoms of prolapse. Recurrent symptomatic UTI’s Carry out comprehensive assessment of bowel or bladder problems using focused assessment tool. Refer to resident’s GP as indicated by ‘Red Flag’ and ‘DIAPPERS’ mnemonic. Consider the need for bladder diary to establish patterns. Establish resident’s bladder and bowel problems and any related Causes of Transient factors/causes/associated risks e.g. environmental, medicines etc Urinary Incontinence. Identify any known wishes / preferences regarding care from the resident and / or representative. ‘DIAPPERS’ Document resident’s problems and care needs in the care plan. D - Delirium I - Infection (urinary) Care Planning A - Atrophic vaginitis/urethritis. Commence a care plan to include: P – Pharmacueticals/Medicines. ◙ Resident and / or family/carer as appropriate. P – Psychological. ◙ Collaboration with other nurses and healthcare professionals involved in the resident’s care. E – Excess urine output. ◙ Consider non-pharmacological treatments that may be effective R – Reduced mobility. and acceptable to the resident adequate fluid intake, dietary changes, bladder retraining, toileting regime etc. ◙ Include interventions to prevent deterioration in functional ability; address skin care needs and the use of incontinence wear aids. ◙ Include methods to monitor and evaluate effectiveness of care. ◙ Agree review schedule / date. Document care plan. Communicate care plan to other healthcare team members involved in the residents care
Monitoring. ◙ Monitor and document effectiveness of interventions planned. ◙ Liaise with resident’s GP. and other healthcare professionals involved in the resident’s care regarding effectiveness or otherwise of treatment. ◙ Amend/ update care plan in accordance with changing needs. ◙ Reassess three monthly or sooner if there is a significant change in care or condition.
Page 4 Continence Care Policy. August 2013 8.0 Responsibilities.
Actions Responsible Person (s)
A record of all staff that have read and signed this policy document will be Person in Charge/Director of maintained. Nursing. Nurses and healthcare staff will be provided with an explanation of the continence Person in Charge/Director of care policy as part of an induction programme. Nursing. All nursing and care staff will attend training on continence care on induction and Person in Charge/Director of every three years. Nursing. Nurses will maintain their competence in continence care and communicate any All registered nurses. knowledge deficits / education needs to the Person in Charge.
Nurses and healthcare staff will sign the policy acknowledgement forms having All nursing and healthcare satisfied themselves that they understand the contents of this policy document. staff.
Each resident will have an initial screening for the presence of bladder or bowel Admitting nurse and/or problems as part of their admission assessment process and as part of their three designated nurse. monthly reassessment or more frequently if there is a significant change to their condition.
Comprehensive assessment of bladder and bowel problems as per policy will be Designated nurse in carried out on all residents identified as having problems in these areas. collaboration with the resident’s GP and other healthcare professionals involved in the residents care Each resident with bowel or bladder problems will have a care plan as per this policy Designated nurse in developed in accordance with her needs and wishes. collaboration with the resident’s GP and other healthcare professionals involved in the residents care Care plans will be developed in collaboration with the resident and /or representative Designated nurse in and other healthcare professionals involved in the care of the resident. collaboration with other nurses on duty as well as other healthcare professionals involved in the resident’s care. A full assessment of the resident’s needs and wishes will be carried out prior to the Nursing and or medical staff use of any type of catheterisation. performing catheterisation.
The resident is monitored for the effectiveness or otherwise of treatments / Nursing staff on duty. interventions being used to promote continence and / or manage incontinence.
Page 5 Continence Care Policy. August 2013 Assessment and Care Planning Protocol for Bladder and Bowel Problems.
8.1 Admission assessment. All residents should be screened for the presence of bladder or bowel problems on admission using the following trigger question: ‘Does the resident have any difficulty or urgency with bladder or bowel function?’ (Essence of Care, 2010).
8.1.1 Screening for bladder and bowel problems should also involve asking the resident and / or representative about any difficulties / needs the resident may have with going to the toilet and what is their normal elimination pattern.
8.1.2 A urinalysis should be performed.
8.1.3 Based on initial assessment observe for / note any ‘red flag’ factors and refer to resident’s general practitioner as appropriate.
8.2 Comprehensive assessment.
8.2.1 Completion of a continence assessment should take place when a resident has been identified as having a bladder or bowel problem.
8.2.2 The purpose of the continence assessment is to attempt to identify the nature of the problem, associated factors or cause(s) so as to inform care planning.
8.2.3 When completing a continence assessment, the nurse should gather the following information: Main complaint / presenting problem and symptoms. Onset of problem. Previous assessments treatments/ management strategies tried: what worked or didn’t work. Any known related causes and/or contributing factors. Volume, frequency and timing of voiding and incontinent episodes from the resident/representative and / or bladder diary. Usual bowel pattern including any incontinence, straining, constipation. Mobility, dexterity and functional ability to eliminate independently: what can the resident do and what assistance does he/she require. Aids and appliances used and efficacy of same. Fluid intake: type and amount of fluids. Psychological / behavioural factors. Medications. Usual diet. Medical / surgical history. Page 6 Continence Care Policy. August 2013 Condition of skin. Effect on quality of life. Resident’s expectations, preferences. (NHS Quality Improvement Scotland, 2005; Deakin University,Australia 2010).
8.2.4 Where urinary incontinence is present, a bladder chart should be completed for the resident (Insert here which bladder chart is in use eg. The 4 day Continence Promotion Unit (HSE) or another). The purpose of the bladder diary is to:
Provide a better picture of the type of incontinence if not already known. To identify the resident’s pattern of fluid intake, amount, types and frequency of fluid intake. To establish the relationship/ association between fluid intake and urinary voiding pattern and output. In particular, the bladder diary can enable nursing staff calculate: Daytime frequency. Nocturia. Total 24 hour input. Maximum and minimum volumes of urine voided and intervals. Total 24 hour urine output. Leakage episodes.
8.2.5 Where assessment identifies any of the following, the resident should be referred to her general practitioner:
9.0 Pain associated with urinary incontinence. 10.0 Recent unexplained weight loss. 11.0 Recent sudden changes in bowel habit. 12.0 Rectal bleeding. 13.0 Persistent diarrhoea. 14.0 Blood in urine visible to the naked eye. 15.0 Haematuria. 16.0 Symptoms of prolapse. 17.0 Recurrent symptomatic UTI’s
Page 7 Continence Care Policy. August 2013 17.1 Care Planning for Bladder and / or Bowel Problems. 17.1.1 Assessment information should be analysed by nursing staff to identify and document the resident’s problem(s/needs) and develop a care plan to meet these needs. 17.1.2 Nursing staff should liaise with the resident’s general practitioner regarding the need for specialist referral. 17.1.3 Care planning should involve the resident as far as he/she is able; the resident’s representative and other healthcare professionals involved in the resident’s care. 17.1.4 The contents of a resident’s care plan will depend on the underlying causes and contributing factors and how these affect the resident on a day to day basis. 17.1.5 Problems /Care needs should be clearly described and interventions should be documented which are evidence based and intended towards a specific outcome or goal.
17.1.6 Problems/care needs related to incontinence may result from or affect a range of daily activities including communication; cognition; skin care, nutrition; toileting needs; mobility; behaviour management and the care for these can be documented under the relevant activities in the resident’s overall care plan. For example, where a resident has dementia and is unable to communicate the need to eliminate or requires their incontinence wear to be changed, the care plan should include any non-verbal cues the resident may use to indicate their need e.g. becomes restless 17.1.7 The care plan should identify what the resident is able to do for him/herself and what assistance he/she need. For example, walking to and from the toilet, managing clothing and meeting personal hygiene needs. 17.1.8 A review schedule for the care plan should be identified and documented. 17.1.9 The resident’s care plan should be amended in accordance with changing needs. 17.1.10 Significant change in the resident’s care and / or condition may trigger the need for reassessment. 17.2 Skin Care for Incontinence.
17.2.1 Excess moisture due to incontinence, perspiration, or wound drainage must be identified and actions documented to eliminate this where possible. When moisture cannot be controlled, interventions that can assist in preventing skin damage should be used.
17.2.2 Consideration to the use of barrier creams should be given where residents are incontinent.
17.2.3 Soap should be avoided where possible, as it tends to dry the skin further. If soap is to be used, it should ideally be unperfumed and rich in moisturisers.
Page 8 Continence Care Policy. August 2013 17.2.4 A soap substitute, such as aqueous cream is preferable to soap as it can be applied to the body and rinsed off with water or used on a sponge or flannel. Although this does cleanse adequately, soap can be used if required to wash flexures and groin or particularly dirty areas.
17.2.5 Washing water should not be too hot as the heat tends to dry the skin further, but it should be warm enough to be comfortable
17.2.6 A no-rinse cleanser, such as Clinisan can be applied during daily care for at least 14 days to reduce the risk of pressure ulcer formation.
17.2.7 Emollient soaps are more effective in prevention of skin tears than non-emollient
17.2.8 The zinc cream, Sudocrem, if used for at least 14 days can reduce skin redness caused by incontinence in older adult residents in long term care.
17.3 Incontinence Dermatitis /Moisture Lesions.
17.3.1 Moisture lesions, also referred to as incontinence associated dermatitis (IAD) are areas of inflammation and irritation, which occurs in the perineal or perigenital areas when the skin comes in contact with urine, faeces or both. They can be very painful. Prolonged contact with urine or faeces can result in tissue breakdown, increase the risk of infection and adversely affect residents’ ’ physical and psychological wellbeing. Factors such as change in pH, activation of proteases, transepidermal water loss (TEWL) and ageing skin are thought to be responsible for the resulting tissue damage.
17.3.2 IAD associated with urinary incontinence tends to occur in skin folds and on the labia majora or the scrotum, whereas IAD associated with faecal incontinence tends to originate in the perianal area. In severe cases, erythema may extend to the lower abdomen and sacrum (Beldon, 2008).
17.3.3 Candidiasis is a common complication of IAD and exhibits as a maculopapular rash with satellite lesions. Other conditions that may appear similar to IAD include:
■ Intertrigo (inflamed skin folds caused by exposure to perspiration, friction and bacterial or fungal bioburden); ■ Periwound maceration (skin breakdown as a result of exposure to wound);
■ Exudate.
■ Pressure ulcers.
Page 9 Continence Care Policy. August 2013 17.4 Prevention and Management of Incontinence Associated Dermatitis.
17.4.1 Every resident with incontinence must have a care plan in place to identify their skin care needs.
17.4.2 Where a resident has excoriation, the grade of the excoriation should be recorded on skin excoriation grading tool (Fig 2 below).
17.4.3 Soap must be avoided. The care plan for the resident will include the use of aqueous cream or clinisan as a soap substitute
17.4.4 Skin must be kept clean and dry. Containment products such as pads must be changed regularly, based on each resident’s assessed needs.
17.4.5 Barrier creams, such as E45 or barrier films should be used to protect the skin in accordance with the grade of excoriation.
17.4.6 If the resident’s skin condition does not improve through the use of the above, the nurse should liaise with the resident’s general practitioner regarding the use of medication ointments.
17.4.7 If the resident has skin excoriation, he /she should have a pain assessment completed.
Page 10 Continence Care Policy. August 2013 Page 11 Continence Care Policy. August 2013 17.5 Use of Containment Products.
17.5.1 Containment products are used for residents to manage incontinence where continence promotion approaches such as bladder retraining are unsuitable. 17.5.2 Each resident must be assessed for selection of the most appropriate containment products that meets their needs and preferences. Containment products include hand held urinals, lifestyle aids, adaptations such as raised toilet seats or commodes. 17.5.3 Residents should be supplied with products that are discreet, of correct size and absorbency and are acceptable to them. 17.5.4 In general Mini pads are recommended for light to moderate urinary incontinence or faecal staining.
Page 12 Continence Care Policy. August 2013 17.5.5 Shaped pads are recommended for moderate to heavy incontinence. They are more appropriate than diapers for residents who are mobile, can stand or transfer, or being toilet trained. They may be used night or day and may be used for residents who are immobile or bed bound. 17.5.6 Pads must be worn with close fitting underpants or net pants. 17.5.7 Taped pads are recommended for use for intractable diarrhoea or for special cases i.e. residents where shaped pads were tried and were unsuccessful; residents with behavioural problems when shaped pads are not tolerated. (Incontinence wear may sometimes increase agitation) 17.5.8 As pad types vary according to the manufacturers, the nurse must always check the manufacturer’s guidance when choosing the appropriate pad. 17.5.9 Barrier creams should be used sparingly because they can block the pores of the pad.
17.5.10 Talcum powders should be avoided as they can reduce the absorbency of the pad. 17.5.11 The practise of double padding is not recommended 17.5.12 Used products should be bagged and disposed of in domestic waste. Infected soiled products should be disposed as per infection control policy.
(Midland Health Board Continence Advisory Service, 2006)
18.0 Guideline for Nursing Management of Bladder and Bowel Problems.
Presenting Problem Possible Causes. Nursing Management. New /recent onset of urinary ? Urinary tract infection. Ascertain baseline urinary incontinence or voiding ? Cognitive changes – function/routine. difficulties. delirium. Check urinalysis – if positive to protein, ? Medications. nitrites, leucocytes, blood – send MSU and treat accordingly. ? Decline in function due to Review medications: see drug-use- acute illness. effect table and discuss with GP if on ? Environmental barriers. any of these drug groups. ? Change in mood. Outrule delirium / depression as cause. ? Use of restraint. Address any functional decline. ? Faecal impaction. Check if any environmental changes / barriers and adjust accordingly. Review restraint if in use. Assess for faecal impaction and refer to GP for examination and further investigation. Page 13 Continence Care Policy. August 2013 Resident has inadequate or ? Inadequate or excessive Discuss further investigations to excessive urinary output. fluid intake. outrule cause with GP and treat / plan ? Underlying diabetes, high care accordingly calcium. Readjust intake to between 1,000mls and 1,500mls.
Nocturnal Polyuria Primary causes Refer to G.P. to investigate causes. Present when: ? Congestive heart failure. Adjustment of secondary causes such Total 24 hour urine volume is ? Renal insufficiency. as caffeine and alcohol intake, fluid normal and the total volume of ? Oestrogen insufficiency consumption close to bedtime and any night time voiding and the first other factors affecting sleep. void of the morning is greater ? Daytime fluid retention than 33% of the total 24 hour ? Venous insufficiency fluid volume in older adults or ? Hypoalbuminaemia greater then 22% in younger ? Diuretic therapy. adults. Secondary causes: (International Continence ? May be due to caffeine Society,) intake, alcohol intake or excessive fluid intake in the evening.
Voiding Difficulties. Overflow due to: Check for UTI Sensation of not emptying Outflow obstruction eg Refer to GP for assessment and bladder completely after enlarged prostate manage care according to cause. finishing urination. Underactive bladder Difficulty starting to pass urine muscle Bladder muscle Dribbling following urination contraction and urethral sphincter relaxation not co-ordinating during voiding
Presenting Problem Possible Causes. Nursing Management. Resident leaks with Stress incontinence Check for UTI physical movement ? due toCaffeine intake Low/high fluid Refer to GP for assessment and such as coughing, intake Urinary tract infection manage care according to cause eg: sneezing, standing up Anxiety and/or laughing. Obesity Reduce caffeine intake Chronic cough Normalise fluid intake Low oestrogen levels. inappropriate fluid Treat UTI intake/voiding pattern Urinary tract Normalise bowel habit infection Constipation Individualised toileting Vaginal prolapse Atrophic changes programme/bladder retraining Neurological disease Diabetes mellitus Refer to dietician re obesity. Advice re smoking Sudden urge to pass Urgency /Overactive bladder – bladder Check for UTI urine and having to rush contracts during filling phase. ? due to: Refer to GP for assessment and to the toilet. Caffeine intake manage care according to cause eg: Difficulty holding on to Low fluid intake Diuretic medication urine before reaching Urinary tract infection Reduced Normalise fluid intake the toilet. mobility/dexterity Anxiety Urinary tract Treat urinary tract infection Page 14 Continence Care Policy. August 2013 infection Constipation Neurological Normalise bowel habit disease Post void residual urine Individualised toileting Diabetes mellitus programme/bladder retraining Reduce caffeine intake if appropriate Functional Difficulties. Address: Resident’s need to be close to toilet. Poor mobility. Clear signage of toilets Difficulty with undoing Assistance / referral to address clothing. mobility and/or dexterity problems Difficulty with personal Eyesight impairment hygiene following Privacy issues toileting. Positioning advice for bladder / bowel Unable to find toilet. emptying Difficulties related to Aids to adjust height of seat in line privacy; height of seat. with resident’s needs/ use footrest. Bowel Movements. See management of Constipation Less than three bowel Constipation. guideline. movements per week and/or Bristol Stool form between 1 and 3 and / or Pain, difficulty or straining to open bowels. Faecal incontinence / leakage related to above symptoms.
Faecal incontinence / leakage not related to symptoms of constipation. Daily exercise programmes designed to improve walking and upper body strength have been shown to be effective in reducing daytime urinary incontinence in cognitively impaired older people living in residential care. (Skelly and Flint, 1995; Tannenbaum and DeBeau, 2004 cited in Queensland Government, 2007.
Guidelines adapted from Queensland Government, 2007; Sprecht, 2005; NHS Scotland, 2005
19.0 Guideline for Management of Constipation. STEP ONE: Fluids, fibre and exercise ◙ A balanced diet, with sufficient fibre and fluid is essential. Increasing fluid intake is one means of managing constipation. Increasing fibre to 25-35g per day is another means of managing constipation. However, a sudden increase in fibre in the older individual is likely to result in abdominal bloating and cramping, flatulence and diarrhea, (Folden, 2002). ◙ Regular exercise is encouraged. 30 minutes exercise per day has been proven to assist in management of urinary incontinence. ◙ Allow two to four weeks for these steps to work, ensuring there are bowel actions in this time period. If this does not resolve constipation, move to step two. ◙ Referral to attending physician GP. /dietitian is indicated when: Compliance with initial dietary advice does not begin to resolve constipation within seven days. The individual has any condition requiring specialist dietitian management, such as diabetes, cardiovascular disease, coeliac disease, food intolerance, advanced renal disease, malnutrition or cancer. An individual is significantly overweight or obese ◙ Referral to other members of the multidisciplinary team may also be appropriate at this stage.
Page 15 Continence Care Policy. August 2013 STEP TWO: Bulk forming laxatives eg Citrucel; fybogel, (Liaison with and prescription by GP.) ◙ Like fibre, bulk forming laxatives increase the bulk of the bowel contents, thus stimulating contraction of bowel muscles. ◙ Adequate fluid intake must be maintained when using bulk-forming laxatives, otherwise they can worsen constipation. In the older immobile individual, it is better to use osmotic or stimulant laxatives instead of bulking agents. ◙ Allow one to three days for these to establish regular bowel motions.
STEP THREE: Stool softeners e.g. Dulcolax (Liaison with and prescription by GP.) 1. These agents soften bowel motions by increasing the amount of lubricant and fluid secreted into the bowel. 2. They are best used when a hard stool mass is present, or to prevent excessive straining. 3. Allow one to five days for these to work.
STEP FOUR: Oral osmotic laxatives e.g. lactulose; movicol (Liaison with and prescription by GP.)
◙ These agents draw fluid into the large intestine. The resulting bulk stimulates bowel movement. ◙ Effect is variable depending on the type and dose of laxative.
STEP FIVE: Stimulants e.g. senekot (Liaison with and prescription by GP.) ◙ These agents stimulate gut movement via an indirect irritant effect. Sometimes they can cause abdominal cramps. ◙ Prolonged use is not recommended as it can lead to a non-functioning colon. Stimulants therefore have a limited role in the treatment of chronic constipation. ◙ Allow six to twelve hours for these to work.
STEP SIX: Suppositories and enemas (Liaison with and prescription by GP.) ◙ These agents act locally by various methods to promote evacuation. They should not be used routinely. Rather, they should be reserved for acute situations. ◙ Allow fifteen to thirty minutes for these to work.
Adapted from Queensland Government, 2007: ‘Stepping out of Constipation’.
Page 16 Continence Care Policy. August 2013 20.0 Catheter Use Protocol.
20.1 The use of internal catheters for the management of incontinence in the Centre is avoided.
20.2 External catheters, where clinically appropriate are used in preference to urinary catheterization.
20.3 Any consideration to use a catheter for a residents must be discussed with the resident and / or representative as appropriate and the resident’s GP.
20.4 The benefits and risks of catheterisation must be discussed with the resident as far as he / she is able and / or the resident’s representative as appropriate.
20.5 The resident’s consent must be sought prior to any form of catheterization. If the resident is unable to give consent, this must be documented.
20.6 Intermittent urethral catheterisation is preferred to indwelling catheters for the management of urinary retention
20.7 Catheterisation should only be carried out by a healthcare professional (nurse/doctor) who has the required training and competence to do so.
20.8 Assessment for Catheter Use:
20.8.1 Assessment for catheterisation will involve the resident/representative as appropriate; the resident’s general practitioner and nursing staff and includes consideration of the following factors: a) Relevant medical, surgical and obstetric history which may directly impact on the use / risk of catheterisation for the resident or contra-indicate use. b) Risks associated with the procedure itself or the use of catheterisation and how these will be managed. c) The type of catheterisation most appropriate to meet the needs and preferences of the resident (eg. Intermittent or indwelling). d) Catheter size. e) Material of catheter most appropriate to the needs and wishes of the resident: The choice of material should be determined by the length of time the catheter will be in use; comfort and tolerance; low rate of infection and any risk of allergies to materials such as latex which may cause an allergic reaction. f) Drainage systems.
Page 17 Continence Care Policy. August 2013 20.9 Where urinary indwelling catheterization is indicated, it is used for the shortest time possible.
20.9.1 Urinary Catheters are considered as part of a resident’s care only in the following circumstances:
◙ The resident has chronic urinary retention / incomplete bladder emptying in residents with idiopathic or neurogenic bladder dysfunction, which may lead to incontinence and repeated urine infections.
◙ To assist in healing an open sacral or perineal wound.
◙ Where it is necessary to monitor urinary output and there is no alternative method available to accurately measure same.
◙ Where the resident expresses a preference for this type of treatment having been given an explanation of all the options available.
◙ To promote the resident’s comfort during end of life care.
(CDC, 2009: HSPC, 2011).
20.9.2 Intermittent Catheterisation (ICS) is indicated for residents with incomplete bladder emptying such as occurs with idiopathic or neurogenic bladder dysfunction. It is the preferred option of catheterisation for the above conditions as it is associated with a reduced risks of catheter associated urinary tract infections (CAUTI) and a better quality of life (HPSC, 2011). However, ICS should not be used in the following circumstances:
21.0Where there is suspected urethral injury or urethral tumours.
22.0Where there is false passage, stricture and for some diseases of the penis, such as injury, tumours or infection (RCN, 2008)
Caution should be displayed with patients following prostatic, bladder neck or urethral surgery and in patients with stent or artificial prosthesis (RCN, 2008).
Page 18 Continence Care Policy. August 2013 22.1.1 Charriere (Ch) size: This refers to the size of the external diameter of the catheter. The smallest size should be chosen so as to allow for adequate drainage of urine. Larger sizes are reserved for residents who have debris, mucous or clots in the urine. Larger sizes can cause irritation and by-passing of urine around the catheter. A size 12-14 Ch is the recommended size for women while 12-16 Ch is generally sufficient for men.
22.1.2 Catheter shaft length: Catheters are available in a variety of lengths. Only male length catheters are long enough to enter the bladder in males. These are usually 40- 45cms.Use of short (female length) catheters in adult males have resulted in trauma to the urethra (NPSA, 2009). Female catheters are usually 23-25cms.However, catheter sizes should be used in accordance with the manufacturer’s instructions.
22.1.3 Balloon size: As a general rule, a balloon size of 10mls for adults is recommended. Larger balloon sizes are generally for post operative use and have been associated with leakage of urine around the catheter.
22.1.4 Catheter Material: According to HPSC, 2011, The selection of catheter material must be based on the following:
23.0The expected duration of use. ◙ Comfort for the resident. ◙ History of allergies to any of the components. ◙ Ease of insertion and removal. ◙ The ability of the catheter material to reduce the likelihood of complications such as colonisation with bacteria; encrustations and tissue damage.
23.1.1 Nurses must check the manufacturers’ instructions regarding the use and maintenance of different types of these catheters.
23.1.2 Drainage systems: It is important to maintain a closed drainage system. The catheter, drainage tubing and bag should form a continuous circuit. This is vital for the prevention of infection. The choice of drainage system will depend on the needs and wishes of the resident, but includes the following options: A leg drainage bag with a drainage tap, which is directly attached to the catheter after insertion and secured to the leg. A drainage bag with a drainage tap, which is secured to a catheter stand. This bag is either attached directly to the catheter after insertion or attached to the drainage tap of a leg bag for overnight drainage (link-system). A non-drainable bag (i.e., no drainage tap) which is secured to a catheter stand. This bag is used for overnight drainage by attaching it to the leg bag drainage tap.
Page 19 Continence Care Policy. August 2013 A combined drainage bag and urinary catheter. This drainage bag is pre-connected to the catheter during the manufacturing process.
23.1.3 2 litre drainage bags connected directly to the catheter are used for residents confined to bed or for night time use and allow for downward drainage of urine. The bag must be connected to a stand and can be used for up to seven days unless there is accidental disconnection, in which case a new bag must be attached. If urine is thick, offensive or mucoid, the bag may need to be changed more often. Where large drainage bags are being used for night time only, a new bag must be connected each night.
23.1.4 Leg bags are more discreet, allow for more freedom of movement and can remain in situ for up to seven days subject to the same exceptions as large drainage bags.
23.1.5 Catheter valves are sometimes used as an alternative to drainage bags for some residents, but are recommended only where the resident has reasonable bladder capacity; adequate cognitive function; adequate dexterity; normal renal function; no evidence of detrusor instability or over activity and no known upper tract dilatation or reflux.
23.1.6 The following principles must be adhered to with drainage systems in use in the centre:
The bag must be kept below the level of the bladder. A catheter stand must be used and the drainage bag outlet port must not be in contact with the floor or other surfaces. The drainage bag must only be changed as recommended by the manufacturer’s instructions. The drainage bag must be emptied regularly and not be allowed to be over two thirds full. A separate clean container must be used for each resident when emptying the drainage bag and it must not touch the drainage tap. Increased fluid intake must be encouraged for each resident, unless contra indicated.
The above information about catheter devices should serve as guidance. Nurses should always check the manufacturers’ instructions prior to the use of any of these devices.
Page 20 Continence Care Policy. August 2013 23.2 Care Planning for Catheter Use.
23.2.1 Every resident who is using either intermittent or indwelling catheterisation must have a plan of care developed to address care and monitoring needs during the period of use.
23.2.2 The plan of care should be developed with the resident and / or his representative in collaboration with other healthcare professionals involved in this aspect of the resident’s care.
23.2.3 The care plan should address the following areas: Date of insertion of the catheter and date of next catheter change. Adequate fluid intake to dilute the urine and promote drainage as well as reduce the risk for constipation, which can contribute for to leakage and by-pass of urine. Daily washing around the meatal junction (opening of the urethra) using soap and water. Avoidance of talcs and creams, which can increase the risk of ascending infection and affect the material of the catheter. Hand washing before and after manipulation of any part of the catheter and drainage system. Education for the resident to enable them carry out self care if they are able and if it is in keeping with their wishes. Emptying of the drainage bags once they are two thirds full. Interventions to address any quality of life issues affecting the resident through use of catheterisation. Monitoring for risks/complications associated with the type of catheterisation in use. Review schedule.
Page 21 Continence Care Policy. August 2013 24.0 Catherisation Procedures.
24.1 General Principles.
24.1.1 Urinary catheterisation should be prescribed by the medical practitioner who is responsible for the resident (HSE, 2006).
24.1.2 An aseptic non-touch technique (Appendix 1) must be used by nurses during insertion of urinary catheteristation (HPSC, p.10, 2011).
24.1.3 A clean technique can be used for self intermittent cathetrisation (HPSC, p. 12, 201.
24.1.4 Suprapubic catheters are initially inserted in theatre.
24.1.5 The resident’s informed consent must be sought and recorded for catheter use and their permission to proceed must be obtained prior to the actual procedure.
25.0 Procedure for Female Catheterisation.
1.1 The nurse carrying out urinary catheterization must have a second member of nursing staff to act as an assistant for the procedure. 1.2 The nurse carrying out the procedure must ensure that requirements for consent have been met prior to the procedure being carried out. 1.3 The nurse must explain the procedure to the resident answering any questions he/she may have and seek permission to continue with the procedure. 1.4 The nurse then carries out the following steps: 1.4.1 Wash hands using soap and water and make sure hands are dried thoroughly using disposable towel. 1.4.2 Clean and disinfect the top of a dressing trolley using Meliseptol disinfectant spray. 1.4.3 Gather the following equipment and place it on the bottom shelf of the dressing trolley: Sterile catheterisation pack. Single use sachets of normal saline for meatal cleansing. Single use 10ml. ampoules of sterile water x 2. Urine specimen container (if required). Catheter of agreed length, size and type. Catheter drainage bag. NB: Ensure that the catheter and drainage bags are compatible –check manufacturers instructions. 10ml syringe to fill the balloon. Anaesthetic gel. Catheter stand if required Bag for waste.
Page 22 Continence Care Policy. August 2013 Light source. 2 pairs of sterile gloves.
1.4.4 Check the equipment for expiry dates and ensure packaging is intact. 1.4.5 Assist the resident into a supine position with her knees drawn up. (The lateral position can be used for residents with limited mobility). 1.4.6 Ensure privacy for the resident. 1.4.7 Place a draw sheet under the lower half of the resident’s body.
1.4.8 Clean hands and put on a disposable apron. 1.4.9 Open the outer packaging of sterile catheter pack and drop the inner pack onto the top of the trolley. 1.4.10 Open the covering of the inner pack ensuring not to touch the inside of the covering and any of the contents. 1.4.11 Open the outer packaging of; Sterile gloves and 10ml syringe and empty onto aseptic field. 1.4.12 Clean hands, return to the trolley and put on sterile gloves. 1.4.13 Arrange equipment on the sterile field. 1.4.14 Ask the assistant to open the sterile water and pour into the small round collection bowl. 1.4.15 Draw up 10mls of sterile water into the syringe and leave for the balloon. 1.4.16 Ask the assistant to open the normal saline and pour it into the empty round collection bowl. 1.4.17 Apply sterile drapes provided over the genitals and between the resident’s legs. 1.4.18 Clean the meatal area with cotton balls soaked in saline using downward wipes. 1.4.19 Hold up a gauze square and ask the assistant to squeeze lubricant anaesthetic gel onto the gauze square. 1.4.20 Apply the anaesthetic gel to the resident’s urethral orifice. 1.4.21 Remove gloves, clean hands and put on the second pair of sterile gloves. 1.4.22 Ask the assistant to open the outer packaging of the catheter and the nurse removes the sterile inner pack containing the catheter. 1.4.23 Open the inner packaging using the perforations to approximately one third of the length of the catheter. 1.4.24 Ask the assistant to open a second ampoule of sterile water and pour a small amount over the tip of the catheter to activate lubrication. 1.4.25 Place the kidney dish/bowl between the resident’s legs to collect urine. 1.4.26 Holding the labia apart, gently introduce the catheter holding the plastic packaging into the urethral orifice.
Page 23 Continence Care Policy. August 2013 1.4.27 Advance the catheter inwards until urine starts to flow and then another two inches to ensure the balloon is in the bladder. 1.4.28 Inflate the balloon with the sterile water from the syringe. 1.4.29 Connect the drainage bag and ensure it is below the level of the bladder. 1.4.30 Secure the drainage bag either to the resident’s thigh or using a catheter stand. 1.4.31 Clean the area, disposing of waste and gloves into the waste bag provided. 1.4.32 Provide advice to the resident about fluid intake, meatal hygiene and positioning of bag as far as they are able. 1.4.33 Ensure the resident is comfortable. 1.4.34 Bring the trolley back to the nurses’ station. 1.4.35 Dispose of waste into domestic waste unless contaminated with infectious material or blood and dispose of syringe into a sharps box. 1.4.36 Wash hands, clean the trolley and clean hands again. 1.4.37 Document procedure in the resident’s progress notes, to include: Indication for catheter insertion. Date and time of catheter insertion. Type and size of catheter. Amount of water used to inflate the balloon. Any complications encountered. Review date. Signed by the nurse who inserted the catheter. 1.4.38 Update the resident’s care plan with instructions for catheter care and meeting the needs of the resident while the catheter is in situ. 1.4.39 Place the sticker on the catheter packaging into the residents notes. 1.4.40 Note any difficulties and / or abnormalities and communicate to the resident’s G.P. Adapted from HSPC (2011).Guidelines for the Prevention of Catheter associated Urinary Tract Infection based on the principles of Aseptic Non Touch Technique.
Page 24 Continence Care Policy. August 2013 26.0 Procedure for Intermittent Catheterisation.
NB: While the HPSC, 2011 state that an aseptic technique be used for intermittent catheterisation, the CDC, (2009) states that In the non-acute care setting, clean (i.e., non- sterile) technique for intermittent catheterization is an acceptable and more practical alternative to sterile technique for patients requiring chronic intermittent catheterization 1.5 Equipment needed Catheter according to resident’s needs. Lubricant, such as Surgilube if catheter is not prelubricated or activated by application of water. Toilet facilities or receptacle for urine. Wet wipe. Measuring jug 1.5.1 Explain the procedure to the resident. 1.5.2 Wash hands using bacterial soap and water or bacterial alcohol hand rub. Apply non- sterile gloves. 1.5.3 Position the resident comfortably, depending on their mobility eg. lying on bed, sitting on toilet or wheelchair. Encourage client to establish the most appropriate/comfortable position to facilitate access to the urethra. (Dougherty and Lister, 2004). 1.5.4 Wash the resident’s genital area with either water and mild soap or a disposable wipe. Clean from front to back. 1.5.5 Apply lubricant to catheter if required. If using a coated catheter which requires activation of the lubricant, fill catheter packet with sterile water. Allow 30 seconds for activation of lubricant.
27.0 Suprapubic Catheterisation
27.1 Suprapubic catheterisation is the insertion of a urinary catheter through the interior wall of the abdomen into the dome of the bladder.
27.2 The procedure is carried out under general or local anesthetic using a percutaneous system.
27.3 For long term use a large charriere size (18 – 22ch) foley catheter is recommended.
27.4 The risks associated with Suprapubic catheters are:
Pain, discomfort and irritation for some people.
Bladder stone formation.
Possible squamous cell carcinoma.
Page 25 Continence Care Policy. August 2013 Urethral leakage.
Infection, swelling encrustation and granulation of the insertion site.
27.5 Care for a Suprapubic catheter is the same as for a urethral catheter.
27.6 Post insertion (7 – 10 days), aseptic technique should be used to clean the insertion site and if required a dressing may be used but is not essential.
27.7 Following this, the site and catheter may be cleaned with warm soapy water using a clean cloth.
27.8 In the event that the suprapubic catheter is accidently removed, a new catheter should be replaced as soon as possible as the stoma closes within a very short period of time.
28.0 Procedure for use of External Catheter in Males
28.1 External catheter devices are urine storage products that may be useful for short-term incontinence treatment in men. Condom catheters are made of latex rubber, polyvinyl or silicone. They are affixed to the shaft of the penis by adhesive and are connected by a tube to a urine-collecting bag.
28.2 External catheters are preferred over indwelling catheters for residents who do not have urinary retention. However, these devices also may lead to urinary tract infections. In addition, external catheters may cause damage to the penis due to friction, ischemia (insufficient blood flow), and obstruction.
28.3 Residents should have an assessment as to the suitability of using an external catheter as residents with cognitive impairment may pull or tamper with the sheath. Also, there is potential for penile trauma if a poor technique by staff or resident is used to remove the sheath.
28.4 Equipment.
External catheter sheath of suitable size.
Drainage bag.
NB: Ensure that the catheter and drainage bags are compatible –check manufacturer’s instructions.
Paper towel
Catheter stand if required
Bag for waste.
Page 26 Continence Care Policy. August 2013 Light source.
28.4.1 Explain the procedure to the resident and as far as he is able obtain his informed consent to proceed.
28.4.2 Assist the resident into a comfortable semi-prone position with protection underneath, while maintaining their dignity
28.4.3 Wash hands and put on apron to prevent the risk of cross infection and protect uniform.
28.4.4 Put on gloves.
28.4.5 To stop pubic hair tangling in or sticking to the sheath it may be necessary to trim the public hair. Trim the hair away from the base of the penis. Shaving should be avoided as re-growth may cause irritation.
28.4.6 To ensure a comfortable fit, use the measuring guide to determine the appropriate sheath size that is required. The measuring guide should be placed at the widest point of the penile shaft. If the size of the penis is measured to be between two sheath sizes, choose the smaller size to prevent leakage.
28.4.7 Wash and dry the penis thoroughly. Avoid creams or powders as this may affect the adhesive of the sheath.
28.4.8 The sheath should be long enough to extend to the base of the penis.
28.4.9 Place sheath over tip of the penis leaving a small gap between the tip of the penis and the narrow outlet tube of the sheath to allow for the free flow of urine.
28.4.10 Hold the sheath in place with one hand, and with the other hand slowly pull the strip of the sheath towards the resident. Unroll the sheath completely.
28.4.11 Gently squeeze the unrolled sheath around the shaft of the penis to ensure a secure fit.
28.4.12 If the sheath does not already have a self adhesive, place the adhesive tape around the base of the penis.
28.4.13 Connect the drainage bag and ensure it is below the level of the bladder.
28.4.14 Secure the drainage bag either to the resident’s thigh or using a catheter stand.
28.4.15 Disposing of equipment according to infection control guidelines.
Page 27 Continence Care Policy. August 2013 28.4.16 Provide advice to the resident about fluid intake and positioning of bag as far as they are able.
28.4.17 Ensure the resident is comfortable.
28.4.18 Document procedure in the resident’s progress notes.
28.4.19 Develop and document care plan for catheter use in the resident’s care plan.
28.4.20 Note any difficulties and / or abnormalities and communicate to the resident’s G.P.
29.0 Daily Care including Catheter and Drainage Bag Changing
29.1 Standard precautions must always be used for catheter care.
29.2 Non sterile gloves should always be worn when handling a catheter.
29.3 Cleaning of the urethral meatus (where the catheter enters the body) is carried out by using routine personal hygiene. 29.3.1 First, use a clean cloth, warm water, and soap to gently wash the urinary meatus.
29.3.2 Wash in a circle-like motion, moving away from the meatus. This helps prevent germs from being moved from the anus into the urethra.
29.3.3 Hold the end of the catheter tube to keep it from being pulled while cleaning.
29.3.4 Wash around the catheter to remove any crust, or mucus.
29.3.5 Always wash the area around the anus last.
29.3.6 Rinse and pat dry the genital area and catheter with a clean towel.
29.4 If the catheter is attached to a leg bag, it is only necessary to change the bag once a week.
29.5 If the leg bag is removed for any reason a new leg bag should be attached.
29.6 Where a long bag is being attached to the leg bag at night, a new long bag should be used each night.
29.7 Long term catheters should be changed only when clinically necessary or according to the manufacturers’ recommendations (usually every 6 -12 weeks).
Page 28 Continence Care Policy. August 2013 30.0 Catheter Maintenance Solutions
30.1 Catheter maintenance solutions should only be used in the following circumstances following prescription by the resident’s G.P.: After an unsuccessful change of catheter program to address blocking. After a catheter history has been taken and recurrent blockage is proven. When there is obvious encrustation. To extend the life of a catheter where blocking is an established problem Catheter maintenance solutions should be used according to the manufacturers’ instructions as part of an individual maintenance programme for the resident. They should not be used in residents with low urinary output and low fluid intake as the acidic solutions could promote the formation of uric acid crystals. There are three types:
1. Normal Saline Normal saline should only be used to identify a blockage and the washing of debris such as blood, mucous and pus. It will not dissolve encrustation but works by gently washing out the lumen of the catheter.
2. Citric acid (3.2%) such as Suby G For the dissolution of struvite crystals which form on the catheter tip under alkaline conditions (pH 7.5-9.5).
3. Citric acid (6%) eg Solution R Effective at dissolving severe encrustation due to its acidic nature. It is used for more persistent crystallisation. It can also be used just prior to catheter removal to dissolve any crystals on the tip of the catheter, which may cause trauma.
(NHS Quality Scotland, 2004., East Cambridge and Fenland Primary care Trust, 2005; Pomfrey, 1999; West Lincolnshire Primary Care Trust, 2005).
30.2 Procedure for Use of Catheter Maintenance Solutions.
30.2.1 Equipment.
Apron New Drainage Bag Prescribed Maintenance Solution Non-sterile Gloves x 2 pairs Page 29 Continence Care Policy. August 2013 Sterile Dressing Towel
30.2.2 Explain the procedure to the resident and as far as he/she is able obtain their informed consent to proceed.
30.2.3 Assist the resident into a comfortable semi-prone position with protection underneath, while maintaining their dignity
30.2.4 Wash hands and put on apron to prevent the risk of cross infection and protect uniform.
30.2.5 Remove leg bag straps and position leg bag beside the resident
30.2.6 Warm the solution in outer packaging, to body temperature by immersing partially in warm water. (To avoid causing bladder spasm).
30.2.7 Open dressing pack. Open outer packaging and slide inner pack into sterile field.
30.2.8 Put on gloves to prevent cross infection.
30.2.9 Close clip on solution container, remove security ring on connection port and disconnect drainage bag from catheter
30.2.10 Remove protective cover from connection port and insert into catheter bell end without touching the connection ends so as not to introduce infection.
30.2.11 Open clip to allow solution to run into the bladder. To prevent damage to the bladder urothelium, this should run in by gravity – the maximum amount would be 50mls (30mls if Urotainer Twin).
30.2.12 Close clip and leave for 15 minutes or as per manufacturers' instructions. Cover the resident with a blanket.
30.2.13 Discard gloves and wash hands
30.2.14 When the required time has elapsed, return to the resident, wash hands and put on new gloves. Remove clip and lower bag to allow the solution in the bladder to drain out by gravity. If using Urotainer Twin, repeat with second sachet. Close clips and remove solution bag.
30.2.15 To reduce contamination from the old bag, connect a new leg bag, and strap to the resident’s leg.
30.2.16 Document procedure in the resident’s progress notes.
Page 30 Continence Care Policy. August 2013 31.0 Infection and Antibiotic Treatment
31.1.1 Infection may arise
either at the time of or immediately following catheter insertion or
subsequently because the colonising flora within the catheterised urinary tract becomes invasive (this may occur spontaneously or follow catheter manipulation).
31.1.2 The presence of pus cells in the urine (pyuria) of a resident with an indwelling catheter does not, by itself, signify infection. Distinguishing between bacteriuria and infection can be difficult making it important to:
Send catheter specimen only if clinical signs of infection are present and not routinely.
Collect a urine sample carefully and transport it rapidly to the laboratory.
If this is not possible, refrigerate sample until immediately prior to transportation
Review positive lab report in conjunction with signs and symptoms of infection before commencing antibiotics.
31.1.3 Clinical signs of infection determine the need for antibiotic therapy; the lab result will guide the choice of the most appropriate agent.
31.1.4 The routine use of prophylactic antibiotic administration in catheterised residents is not recommended because of its tendency to encourage the emergence of resistant organisms.
31.1.5 Antibiotic prophylaxis when changing catheters should only be used for residents with a history of catheter-associated urinary tract infection following catheter change, or for residents who have a heart valve, septal defect, patent ductus or prosthetic valve.
Page 31 Continence Care Policy. August 2013 Appendix 1: Insertion of Indwelling Catheter Non –Touch Technique.
(Original Poster Can be Downloaded from http://www.hpsc.ie/hpsc/A- Z/MicrobiologyAntimicrobialResistance/InfectionControlandHAI/UrinaryCatheters/Posters/File,1 2911,en.pdf)
Page 32 Continence Care Policy. August 2013 2.0 References. 1. NHS Modernisation Agency, (2003) Essence of Care; Patient-focused benchmarks for clinical governance. NHS. 2. NHS Quality Improvement Scotland, (2005). Best Practice Statement: Continence – adults with urinary dysfunction. 3. NHS Quality Improvement Scotland, (2004). Best Practice Statement: Urinary Catheterisation and Catheter Care. 4. Royal College of Nursing, (2002) Improving continence care for patients. The role of the nurse. RCN. London. 5. Whitehead WE, Wald A, Diamant NE et al. (2002) Functional faecal incontinence. In: Drossman DA, eds. Rome 11: The functional Gastrointestinal Disorders: Diagnosis, Pathophysiology, and Treatment- A multinational Concensus.2nd Ed McLean, Va: Degnon Assoc, 2000. 6. Pomfrey, I (2000) Catheter care in the community. Nursing Standard. 14(27) pp. 46-51. 7. East Cambridgeshire and Fenland Primary Care Trust (2005) Catheter care Guidelines. Accessed 4/02/2008 @ http://www.eastcambsandfenland-pct.nhs.uk/documents/About %20us/Clinical%20Governance/DtGP/Clinical%20Policies/Continence %20Team/Catheter%20Care%20Guidelines.pdf? preventCache=15%2F09%2F2006+12%3A56 8. National Institute for Health and Clinical Excellence (2006) The management of urinary incontinence in women accessed 2/02/2008 @ www.nice.org.uk 9. Midland Health Board, (2006) Guideline for adult catheter management in females. Accessed 3/02/2008 @ www.mhb.ie 10. Health Surveillance and Protection Agency (2011) Guidelines for the Prevention of Catheter associated Urinary Tract Infection. 11. Centre for Disease Control (2009) 12. Specht, J. (2005) 9 Myths of Incontinence in Older Adults. American Journal of Nursing Vol. 105(6) pp. 58-65. 13. Hartford Institute for Geriatric Nursing (2008) Urinary Incontinence. Nursing Standard of Practice Protocol: Urinary Incontinence in Older Adults admitted to Acute Care. 14. Scottish Intercollegiate Network (2004) Management of urinary incontinence in primary care accessed 2/02/2008 @ www.sign.ac.uk 15. The State of Queensland, Queensland Health, (2007) First Steps in the management of urinary incontinence in community dwelling older people: a clinical practice guideline for primary clinicians.accessed 3/02/2008 @ http://www.health.qld.go GUIDELINE FOR PREVENTION OF CATHETER- ASSOCIATED URINARY TRACT INFECTIONSv.au/mass/docs/resources/continence/firststepsrevfront.pdf
Page 33 Continence Care Policy. August 2013 16. West Lincolnshire Primary Care Trust (2005) Catheterisation Policy accessed 4/02/2008 @ www. westlincs pct.nhs.uk/ Policies &manuals/Clinical%20governance/WLQD23%20- %20 Catheterisation %20 Policy .pdf 17. Nursing Standard, (2000) Continence Assessment Quick Reference Guide. Nursing Standard. Vol 14(24). 18. Dougherty L., Lister, S. (2004) The Royal Marsden Hospital Manual Clinical Nursing Procedures. Blackwell Publishing: London. 19. Barton, R. (2000) Intermittent self-catherisation. Nursing Standard 15(9) 1-9 20. Bennett, E (2002) Intermittent self-catherisation and the female patient. Nursing Standard. 30(17) 37-42. 21. Midland Health Board, (2005) Guideline for Intermittent Urethral Catheterisation of Adults and Children accessed at www.mhb.ie 22. The Association for Continence Advice, (2004) Intermittent Catheterisation. Notes on Good Practice. www.aca.uk.com 23. Midland Health Board, Continence Advisory Service (2006) Guideline for The provision of Disposable Containment Products accessed at www.mhb.ie
Page 34 Continence Care Policy. August 2013