Cricothyrotomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Generic Procedures for Assessment and Response During a Radiological
IAEA-TECDOC-1162 Generic procedures for assessment and response during a radiological emergency August 2000 The originating Section of this publication in the IAEA was: Radiation Safety Section International Atomic Energy Agency Wagramer Strasse 5 P.O. Box 100 A-1400 Vienna, Austria Emended version, March 2013. Details of revisions are available at: www.pub.iaea/books/ GENERIC PROCEDURES FOR ASSESSMENT AND RESPONSE DURING A RADIOLOGICAL EMERGENCY IAEA, VIENNA, 2000 IAEA-TECDOC-1162 ISSN 1011–4289 © IAEA, 2000 Printed by the IAEA in Austria August 2000 FOREWORD One of the most important aspects of managing a radiological emergency is the ability to promptly and adequately determine and take actions to protect members of the public and emergency workers. Radiological accident assessment must take account of all critical information available at any time and must be an iterative and dynamic process aimed at reviewing the response as more detailed and complete information becomes available. This manual provides the tools, generic procedures and data needed for an initial response to a non-reactor radiological accident. This manual is one out of a set of IAEA publications on emergency preparedness and response, including Method for the Development of Emergency Response Preparedness for Nuclear or Radiological Accidents (IAEA-TECDOC-953), Generic Assessment Procedures for Determining Protective Actions During a Reactor Accident (IAEA-TECDOC-955) and Intervention Criteria in a Nuclear or Radiation Emergency (Safety Series No. 109). The procedures and data in this publication have been prepared with due attention to accuracy. However, as part of the ongoing revision process, they are undergoing detailed quality assurance checks; comments are welcomed, and following a period of time that will have allowed for a more extensive review, the IAEA will revise the publication as part of the process of continuous improvement. -

Emergency Plan Checklist Center Name: License ID
Emergency Plan Checklist Center Name: License ID: Prepare written emergency procedures delineating the following: Location of the first aid kit and additional first aid supplies Name, address and telephone number of the physician retained by the center or of the health facility used in emergencies Procedure for obtaining emergency transportation Hospital and or clinic to which injured or ill children will be taken Phone numbers for police, fire, ambulance and Poison Control (National Poison Emergency Hotline at 800-222- 1222) Location of written authorization from parent(s) for emergency medical care for each child Diagram indicating how the center is to be evacuated in an emergency from each classroom and the outdoor play area Location of fire alarms and fire extinguishers Procedures for ensuring children’s safety and communicating with parents in the event of evacuation, lockdown, natural or civil disaster and other emergencies Plan for informing parents of their children’s whereabouts The local law enforcement agency or emergency management office that has been notified of the center’s identifying information as listed below: The center’s name and location The number and ages of children enrolled The number of staff The need for emergency transportation; the location to which children will be evacuated The plan for a lockdown The plan for reuniting children with their parents To Find Your County’s Office of Emergency Management Coordinators, Visit: http://ready.nj.gov/about-us/county-coordinators.shtml Other: Ensure emergency plan is posted for reference or is readily accessible in a designated location in the center Maintain 1 evacuation crib per 4 enrolled non-ambulatory infant/toddler children (if applicable) Staff have been trained in procedures for operating locking devices used for lockdown procedures (if applicable) Notes for Emergency Plan: OOL/10.28.2017 . -

Voice After Laryngectomy ANDREW W
Voice After Laryngectomy ANDREW W. AGNEW, DO APRIL 9, 2021 Disclosures None Overview Normal Anatomy and Physiology Laryngectomy versus Tracheotomy Tracheostomy Tubes Voice Rehabilitation Case Scenarios Terminology Laryngectomy – surgical removal of the entire larynx (voice box) Laryngectomy stoma– opening the neck after a laryngectomy Tracheotomy – procedure to create a surgical airway from the neck to the trachea Tracheostomy – the opening in the neck after a tracheotomy Normal Anatomy of the Airway Upper airway: Nasal cavities: ◦ Warm, filter and humidify inspired air Normal Respiration We breathe primarily by the action of the diaphragm and rib cage Thus, whether people breathe through the nose and mouth or a tracheostoma, the physiology of respiration remains the same Normal Anatomy of the Airway ◦ Phonation ◦ Respiration ◦ Airway Protection during deglutition ◦ Val Salva Postsurgical Anatomy Contrast Patient s/p tracheotomy Patient s/p total laryngectomy Laryngectomy •Removal of the larynx (voice box) •Indications • Advanced laryngeal cancer • Recurrent laryngeal cancer • Non functional larynx Laryngectomy •Fundamentally life changing operation •Voice will never be the same •Smell decreased or absent •Inspired air is not warmed and moisturized •Permanent neck opening (stoma) •Difficult to have head under water Laryngectomy Operative Otolaryngology Head and Neck Surgery. Pou, Anna. Published January 1, 2018. Pages 118-123. Laryngectomy Operative Otolaryngology Head and Neck Surgery. Pou, Anna. Published January 1, 2018. Pages 118-123. Laryngectomy Operative Otolaryngology Head and Neck Surgery. Pou, Anna. Published January 1, 2018. Pages 118-123. Postsurgical Anatomy Contrast Patient s/p tracheotomy Patient s/p total laryngectomy Tracheotomy •Indications • Bypass upper airway obstruction • Prolonged ventilator dependence • Pulmonary hygiene • Reversible Tracheotomy Byron J. -

2Nd Quarter 2001 Medicare Part a Bulletin
In This Issue... From the Intermediary Medical Director Medical Review Progressive Corrective Action ......................................................................... 3 General Information Medical Review Process Revision to Medical Record Requests ................................................ 5 General Coverage New CLIA Waived Tests ............................................................................................................. 8 Outpatient Hospital Services Correction to the Outpatient Services Fee Schedule ................................................................. 9 Skilled Nursing Facility Services Fee Schedule and Consolidated Billing for Skilled Nursing Facility (SNF) Services ............. 12 Fraud and Abuse Justice Recovers Record $1.5 Billion in Fraud Payments - Highest Ever for One Year Period ........................................................................................... 20 Bulletin Medical Policies Use of the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Codes on Contractors’ Web Sites ................................................................................. 21 Outpatient Prospective Payment System January 2001 Update: Coding Information for Hospital Outpatient Prospective Payment System (OPPS) ......................................................................................................................... 93 he Medicare A Bulletin Providers Will Be Asked to Register Tshould be shared with all to Receive Medicare Bulletins and health care -

Tracheostomy Technique: Approach Considerations 11/10/2016, 18:05
Tracheostomy Technique: Approach Considerations 11/10/2016, 18:05 No Results News & Perspective Drugs & Diseases CME & Education close Please confirm that you would like to log out of Medscape. If you log out, you will be required to enter your username and password the next time you visit. Log out Cancel Tracheostomy Technique Author: Jonathan P Lindman, MD; Chief Editor: Ryland P Byrd, Jr, MD more... Updated: Jan 21, 2015 Approach Considerations http://emedicine.medscape.com/article/865068-technique Page 6 of 15 Tracheostomy Technique: Approach Considerations 11/10/2016, 18:05 Endoluminal Intubation may replace or precede tracheostomy and is comparably easy, more rapidly performed, and well tolerated for short periods (generally 1-3 weeks). The intraoperative control provided by an endotracheal tube facilitates tracheostomy. The only reason not to intubate is the inability to do so. Contraindications to intubation include C-spine instability, midface fractures, laryngeal disruption, and obstruction of the laryngotracheal lumen. Supplements to intubation include the nasal airway trumpet, which provides dramatic relief of airway obstruction caused by soft tissue redundancy, collapse, or enlargement in the nasopharynx. The oral airway prevents the tongue from collapsing against the back wall of the oropharynx. Alert patients do not tolerate the oral airway, and patients obtunded enough to tolerate the oral airway without gagging should probably be intubated. Intubation can be performed orally or nasally, depending on local trauma and the logistics of planned operative intervention. Emergent Cricothyrotomy The advantage of performing emergent cricothyrotomy is that the cricothyroid membrane is superficial and readily accessible, with minimal dissection required. The disadvantage is that the cricothyroid membrane is small and adjacent structures (eg, conus elasticus, cricothyroid muscles, central cricothyroid arteries) are jeopardized; moreover, the cannula may not fit. -

CONFINED SPACE ENTRY PROGRAM Owner: Risk Management Document Number: EHS S-004 Revision No: 01 Date Last Revised: 08-2-2018
CONFINED SPACE ENTRY PROGRAM Owner: Risk Management Document number: EHS S-004 Revision No: 01 Date last revised: 08-2-2018 Contents 1.0 Applicability ......................................................................................................................................................2 2.0 Scope ...............................................................................................................................................................2 3.0 Definitions ........................................................................................................................................................2 4.0 Core Information and Requirements ...............................................................................................................4 5.0 Roles and Responsibilities ............................................................................................................................ 29 6.0 Goals, Objectives and Performance Measures ............................................................................................ 32 7.0 Training ......................................................................................................................................................... 33 8.0 Program Evaluation ...................................................................................................................................... 34 9.0 Resources .................................................................................................................................................... -
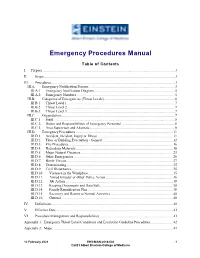
Emergency Procedures Manual
Emergency Procedures Manual Table of Contents I. Purpose ............................................................................................................................................ 3 II. Scope ........................................................................................................................................... 3 III. Procedures ................................................................................................................................... 3 III.A. Emergency Notification Process ........................................................................................... 3 III.A.1. Emergency Notification Diagram...................................................................................... 5 III.A.2. Emergency Numbers ........................................................................................................ 5 III.B. Categories of Emergencies (Threat Levels) ........................................................................... 6 III.B.1. Threat Level 1 .................................................................................................................. 7 III.B.2. Threat Level 2 .................................................................................................................. 7 III.B.3. Threat Level 3 .................................................................................................................. 7 III.C. Organization........................................................................................................................ -

Model SOP Standard Operating Procedure
Model SOP for Training Purposes Only Firetactics.com Model SOP Standard Operating Procedure Firetactics.com Paul Grimwood FIFireE ‐ SOP 1/Version 2/2009 1. TACTICAL DEPLOYMENT INTO FIRE INVOLVED STRUCTURES Sections 1. Purpose 1. Purpose The following bulletin serves as a training 2. Pre‐planning document that covers a range of critical 3. Information ‘in’ tasking issues associated with the safe 4. Risk Management and effective deployment of firefighters 5. Information ‘out’ into fire involved structures. It is not a 6. Situation Awareness complete SOP by any means but simply 7. Staffing stands to inform of a risk‐assessed 8. Water Supply process for compartment and structural 9. Primary Attack fire‐fighting. 10. Search & Rescue However, this document may serve as a 11. Securing Team Safety model upon which more detailed 12. Tactical Ventilation operational procedures may be 13. Primary (First Response) Command & Control developed. 14. Accountability 15. BA Emergency Procedure All students are strongly advised to follow 16. Communication their own departmental SOPs at all times. 17. Principal Officer (First Chief) Command & Control Any deviation from such procedure must 18. Large Volume Structures only be made with good reason and 19. High‐rise Buildings should be held accountable at a later stage. 20. The Most Common Reasons for Traumatic Fire‐fighter Life Losses 2. Pre‐planning It is essential that familiarization visits are made to all large volume structures, or those presenting excessive or unusual risks, so that plans may are organised and provided on‐site in special premises information boxes located at main entry points. Alternatively, these may be held on computer terminals and down loaded into a fire engine’s computer system as they arrive on‐scene. -

Tracheotomy in Ventilated Patients with COVID19
Tracheotomy in ventilated patients with COVID-19 Guidelines from the COVID-19 Tracheotomy Task Force, a Working Group of the Airway Safety Committee of the University of Pennsylvania Health System Tiffany N. Chao, MD1; Benjamin M. Braslow, MD2; Niels D. Martin, MD2; Ara A. Chalian, MD1; Joshua H. Atkins, MD PhD3; Andrew R. Haas, MD PhD4; Christopher H. Rassekh, MD1 1. Department of Otorhinolaryngology – Head and Neck Surgery, University of Pennsylvania, Philadelphia 2. Department of Surgery, University of Pennsylvania, Philadelphia 3. Department of Anesthesiology, University of Pennsylvania, Philadelphia 4. Division of Pulmonary, Allergy, and Critical Care, University of Pennsylvania, Philadelphia Background The novel coronavirus (COVID-19) global pandemic is characterized by rapid respiratory decompensation and subsequent need for endotracheal intubation and mechanical ventilation in severe cases1,2. Approximately 3-17% of hospitalized patients require invasive mechanical ventilation3-6. Current recommendations advocate for early intubation, with many also advocating the avoidance of non-invasive positive pressure ventilation such as high-flow nasal cannula, BiPAP, and bag-masking as they increase the risk of transmission through generation of aerosols7-9. Purpose Here we seek to determine whether there is a subset of ventilated COVID-19 patients for which tracheotomy may be indicated, while considering patient prognosis and the risks of transmission. Recommendations may not be appropriate for every institution and may change as the current situation evolves. The goal of these guidelines is to highlight specific considerations for patients with COVID-19 on an individual and population level. Any airway procedure increases the risk of exposure and transmission from patient to provider. -

Subcutaneous Emphysema Complicating Asthma
Arch Dis Child: first published as 10.1136/adc.31.156.133 on 1 April 1956. Downloaded from SUBCUTANEOUS EMPHYSEMA COMPLICATING ASTHMA BY J. R. K. HENRY From Hammersmith Hospital, London (RECEIVED FOR PUBLICATION JANUARY 5, 1956) Subcutaneous emphysema complicating asthma She was given adrenaline, 4 minims subcutaneously, is a somewhat rare condition and when first met with crystalline penicillin, 250,000 units six-hourly, 'gantrisin', rather an alarming one. Subcutaneous emphysema 1 g. six-hourly, phenobarbitone, i grain, and oxygen by as a secondary manifestation of trauma of the chest mask immediately. There was some improvement following the sub- wall, fracture of the orbit with escape of air from cutaneous adrenaline, and it was thought that she would the nasal sinuses to the neck and thorax, or on probably settle down and have a good night. However, occasion complicating tracheotomy or thoracentesis, she was restless and vomited three times during the night. is probably more common, and the mechanism The following morning her condition had obviously whereby the air reaches the subcutaneous tissues is deteriorated, and on questioning she admitted to having certainly more easily understood. had a severe pain in the left chest. The respiratory rate Elliott (1938) reports subcutaneous emphysema was now 70 per minute, pulse 170 per minute, and in a woman of 46, developing at the onset of an temperature 1010 F. The cyanosis was more marked asthmatic attack and followed two days later by a and had an unusual maroon tinge. She was obviously in great distress. partial pneumothorax. In this case the sub- On examination there was surgical emphysema copyright. -

Laryngectomy
LARYNGECTOMY Definitlon Laryngectomy is the partial or complete surgical removal of the larynx, usually as a treatment for cancer of the larynx. Purpose Normally a laryngectomy is performed to remove tumors or cancerous tissue. In rare cases, it may be done when the larynx is badly damaged by gunshot, automobile injuries, or similar violent accidents. Laryngectomies can be total or partial. Total laryngectomies are done when cancer is advanced. The entire larynx is removed. Often if the cancer has spread, other surrounding structures in the neck, such as lymph nodes, are removed at the same time. Partial laryngectomies are done when cancer is limited to one spot. Only the area with the tumor Is removed. Laryngectomies may also be performed when other cancer treatment options, such as radiation or chemotherapy. fail. Precautions Laryngectomy is done only after cancer of the larynx has been diagnosed by a series of tests that allow the otolaryngologist (a specialist often called an ear, nose, and throat doctor) to look into the throat and take tissue samples (biopsies) to confirm and stage the cancer. People need to be in good general health to undergo a laryngectomy, and will have standard pre-operative blood work and tests to make sure they are able to safely withstand the operation. Description The larynx is located slightly below the point where the throat divides into the esophagus, which takes food to the stomach, and the trachea (windpipe), which takes air to the lungs. Because of its location, the larynx plays a critical role in normal breathing, swallowing, and speaking. -

Conversion of Emergent Cricothyrotomy to Tracheotomy in Trauma Patients
REVIEW ARTICLE Conversion of Emergent Cricothyrotomy to Tracheotomy in Trauma Patients Peep Talving, MD, PhD; Joseph DuBose, MD; Kenji Inaba, MD; Demetrios Demetriades, MD, PhD Objectives: To review the literature to determine the patients for whom cricothyrotomy was performed, in- rates of airway stenosis after cricothyrotomy, particu- cluding 368 trauma patients who underwent emergent larly as they compare with previously documented rates cricothyrotomy. The rate of chronic subglottic stenosis of this complication after tracheotomy, and to examine among survivors after cricothyrotomy was 2.2% (11/ the complications associated with conversion. 511) overall and 1.1% (4/368) among trauma patients for follow-up periods with a range from 2 to 60 months. Only Data Sources: We conducted a review of the medical 1 (0.27%) of the 368 trauma patients in whom an emer- literature by the use of PubMed and OVID MEDLINE da- gent cricothyrotomy was performed required surgical tabases. treatment for chronic subglottic stenosis. Although the literature that documents complications of surgical air- Study Selection: We identified all published series that way conversion is scarce, rates of severe complications describe the use of cricothyrotomy, with the inclusion of up to 43% were reported. of the subset of patients who require an emergency air- way after trauma, from January 1, 1978, to January 1, Conclusions: Cricothyrotomy after trauma is safe for ini- 2008. tial airway access among patients who require the estab- lishment of an emergent airway. The prolonged use of a Data Extraction: Only 20 published series of crico- cricothyrotomy tube, however, remains controversial. Al- thyrotomy were identified: 17 retrospective reports and though no study to date has demonstrated any benefit 3 prospective, observational series.