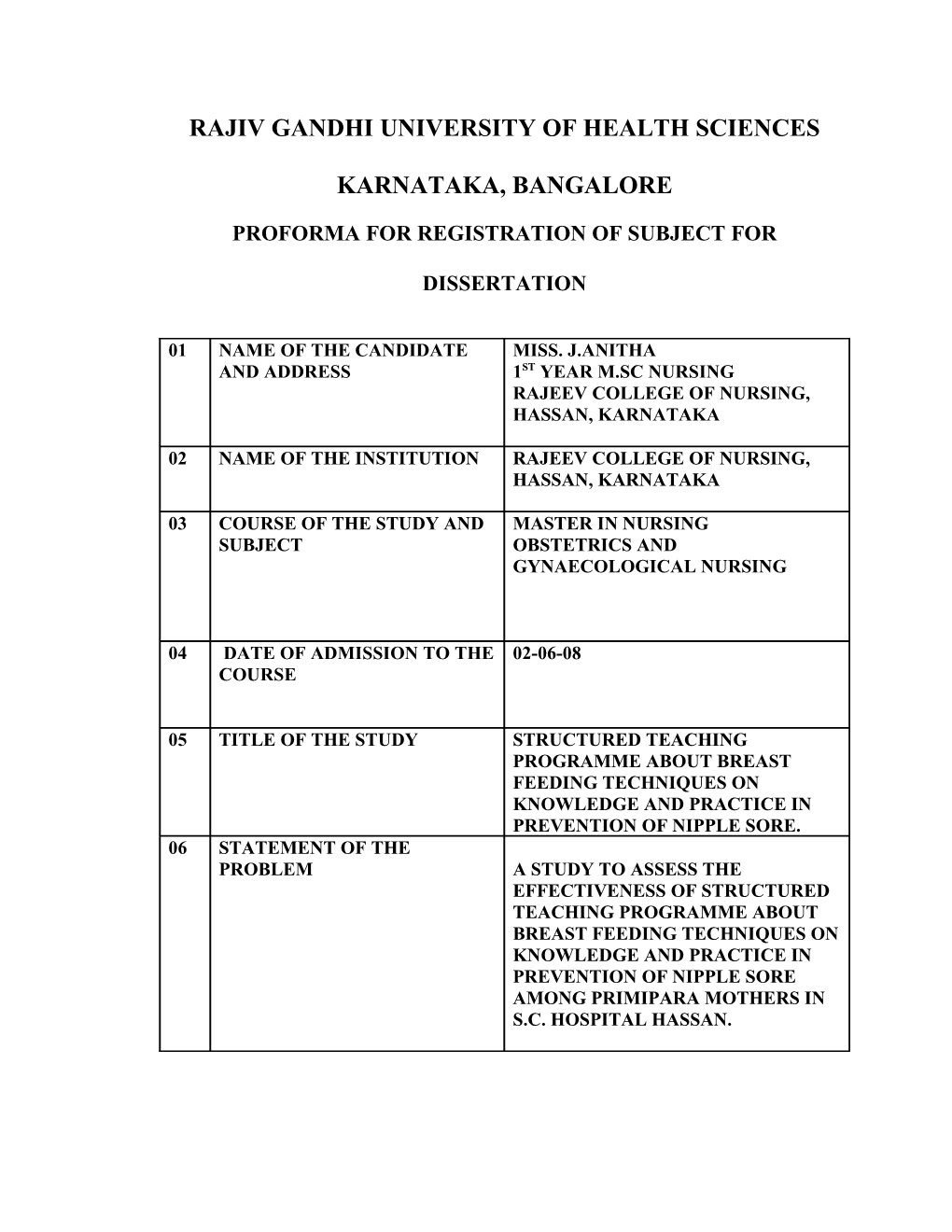
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
KARNATAKA, BANGALORE
PROFORMA FOR REGISTRATION OF SUBJECT FOR
DISSERTATION
01 NAME OF THE CANDIDATE MISS. J.ANITHA AND ADDRESS 1ST YEAR M.SC NURSING RAJEEV COLLEGE OF NURSING, HASSAN, KARNATAKA
02 NAME OF THE INSTITUTION RAJEEV COLLEGE OF NURSING, HASSAN, KARNATAKA
03 COURSE OF THE STUDY AND MASTER IN NURSING SUBJECT OBSTETRICS AND GYNAECOLOGICAL NURSING
04 DATE OF ADMISSION TO THE 02-06-08 COURSE
05 TITLE OF THE STUDY STRUCTURED TEACHING PROGRAMME ABOUT BREAST FEEDING TECHNIQUES ON KNOWLEDGE AND PRACTICE IN PREVENTION OF NIPPLE SORE. 06 STATEMENT OF THE PROBLEM A STUDY TO ASSESS THE EFFECTIVENESS OF STRUCTURED TEACHING PROGRAMME ABOUT BREAST FEEDING TECHNIQUES ON KNOWLEDGE AND PRACTICE IN PREVENTION OF NIPPLE SORE AMONG PRIMIPARA MOTHERS IN S.C. HOSPITAL HASSAN. 6. BRIEF RESUME OF INTENDED WOEK: 6.1 INTRODUCTION
Breast-feeding is good for new mothers as well as for their babies. There are no bottles to sterilize and no formula to buy, measure and mix. It may be easier for a nursing mother to lose the pounds of pregnancy as well, since nursing uses up extra calories. Lactation also stimulates the uterus to contract back to its original size.
A nursing mother is forced to get needed rest. She must sit down, put her feet up,and relax every few hours to nurse. Nursing at night is easy as well. No one has to stumble to the refrigerator for a bottle and warm it while the baby cries. If she's lying down, a mother can doze while she nurses.
Nursing is also nature's contraceptive--although not a very reliable one. Frequent nursing suppresses ovulation, making it less likely for a nursing mother to menstruate, ovulate, or get pregnant. There are no guarantees, however. Mothers who don't want more children right away should use contraception even while nursing. Hormone injections and implants are safe during nursing, as are all barrier methods of birth control. The labeling on birth control pills says if possible another form of contraception should be used until the baby is weaned.
Breast-feeding is economical also. Even though a nursing mother works up a big appetite and consumes extra calories, the extra food for her is less expensive than buying formula for the baby. Nursing saves money while providing the best nourishment possible. The WHO recommends breastfeeding the baby exclusively (no water, formula, juice or solid food) for the fist six months of life and then continuing to breastfeed until the second year of age or longer as mutually desired by both mother and child.
Breast-feeding problems can be avoided if the mothers understand the basics of breastfeeding technique. Proper Breastfeeding techniques (positioning, latching and sucking) and “let down” of milk is crucial to exclusive breastfeeding and long term breastfeeding success.99% of all mothers around the world can make enough breast milk to feed one baby, or multiple babies, if they learn how. It is all in the techniques.
How Breastfeeding Enhances Mother-Child Bonding
Scientists have long known that the mother's brain is flooded with oxytocin when breastfeeding. But until recently, they had been puzzled as to how enough oxytocin was produced to alter the mother's moods.
A study published on July 18, 2008 at the Public Library of Science Computational Biology found that breastfeeding mobilizes more than the usual brain cells that secrete oxytocin. Breastfeeding puts dendrites to work as well to secrete oxytocin.
Oxytocin, which is also secreted during labor and sexual intercourse, is also known as the "love hormone". It increases feelings of trust, relaxation and love. It has a sedative effect. No wonder many women report feeling drowsy while breastfeeding. Breastfeeding also fosters closeness between mother and child in other ways. It enables Mommy and baby to have more physical and skin-to-skin contact. Mothers and babies gaze into each other's eyes for extended periods of time while breastfeeding. Mothers also tend to interact in other ways with their babies when breastfeeding. In contrast, bottle-fed babies can easily be passed on to other people to be fed -- making it easier for Mom to be separated from baby - and worse be fed without any human contact at all, through a bottle prop While breastfeeding has been shown in several studies to help immensely with mother- child bonding,
Getting off to the Right start; Initiate Breast feeding for the first time as soon as after birth as possible, using proper techniques, including “let down” and ask to “room-in” with the baby Breast feeding “on demand” between 8-12 times per day throughout the first six to eight weeks of life.
Many women who breastfeed their babies have sore nipples at some timed using their experience. While mothers nursing their first babies and some mothers with delicate skin seem to develop sore nipples more easily than other mothers, and any woman can gets it if she does not follow proper nipple care and nursing techniques.
Sore nipples are probably the most common complaint after the birth. They are generally reported by the second day after delivery but improve with in five days. Pain beyond the first week, severe pain, cracking, fissures or localized swelling is not normal. The mother should see a doctor for further evaluation. Sore nipples, a common cause of pain often comes from the baby if latching is not proper.
Sore nipples in the first days and weeks of postpartum are usually the result of poor latch on or baby’s sucking techniques. Sore nipples that persist beyond the early weeks of post partum or that occur after weeks or months of pain-free Breastfeeding may have other causes such as a candidia infection.
The best way to prevent sore nipple is the mother to make sure the baby is properly positioned at the breast and has latched on correctly, taking all the nipple and as much of the areola (colored part of the breast) as possible in to his mouth. Check to see that the baby is turned in to mother, tummy to tummy, his mouth at the level of mother’s nipple, and that he does not have to turn his head to grasp the nipple. When we help him latch on, gently touch his lower lip with mother’s nipple and wait until he opens his mouth, as if yawning. Then hug him quickly on to the breast. Ninety (90%)percent of sore nipples complaints are caused by poor positioning and poor latching. Nursing mothers counselor can help to evaluate and make adjustments in getting the baby to breast.
Many women avoid breast-feeding their newborns simply because they are afraid they will suffer from sore nipples. The most difficult period of nursing is during the first few days and weeks as mothers are forming a relationship with their newborn. They are most likely tired from the lack of sleep and if this is their first breast-feeding experience, they could be struggling to find the right positioning for their baby during feeding time. One of the best ways to prevent sore nipples is to get their baby positioned properly. There are several different positions that they can choose from, the cradle hold, cross- cradle hold, the football or clutch hold or both are lying down. Regardless of which position they choose, there is some things mothers need to do to be sure that both are in a comfortable position. 6.2 NEED FOR THE STUDY
A sore nipple associated with breast-feeding is a common problem, with an incidence ranging from 11% to 90% and may lead to premature weaning. This frequently occurs from incorrect positioning at the breast. In addition traumatized nipples can readily become super infected with bacteria or yeast, the presence of which can delay healing, even when positioning and latching on are corrected.
Latching on and suckling of healthy term neonates breastfeeding assessment was conducted in USA (2007). Increasing Breast-feeding duration and exclusively is an acknowledged public health priority. Breast feeding problems especially with the healthy term neonates latching on or feeding with a sub optimal latch are common reason for early breast feeding termination when they result in inadequate breast feeding, poor milk transfer and sore nipples. This article describes clinical strategies for systematic latch on and suckling assessment with the goal of improving the skills of Clinicians who provide care for Breast-feeding women.
A study conducted on Training health care workers to counsel Breast-feeding mothers. They have designed 40 hours counselling course for maternal and child health workers that aim to impact the skills needed to assist mothers to Breast feeding their infants. The health workers are trained on the attachment and positioning techniques that promote successful breast-feeding. Such techniques include having the infant’s chin touch the breast. More areola exposed above than below the infant’s mouth, close contact with the mother’s body and arrangement of the baby’s head and body in a straight line. Finally the study recommended that such as mother’s fears that they are not producing enough milk, sore nipples and breast-feeding practice when the infant is sick. At the conclusion of the training health workers apply the skills, they have learned in maternity wards and maternal child clinic. A study about the influence of breastfeeding techniques on the frequencies of exclusive breastfeeding and nipple trauma in the first month of lactation (2005). Among 211 unfavorable parameters of breastfeeding mother-baby pairs in the maternity ward and at day 30, at home. This study compared the frequencies of these parameters between mothers practicing or not exclusive breastfeeding at days 7 and 30, and between mothers with or without nipple trauma at the hospital. This study shown the number of unfavorable parameters in the maternity ward was similar for mother-baby pairs practicing or not exclusive breastfeeding at day 7 and 30. However, at day 30,it was on average, lower among those under exclusive breastfeeding, regarding positioning. This study concluded that the frequencies of exclusive breastfeeding in the first month and of nipple trauma were not influenced by the breastfeeding technique in the maternity ward, but there was an association between a better technique at day 30 and the practice of exclusive breastfeeding.
A Study of the latching process and pain in breast-feeding mothers with sore nipples in USA (2003). The purpose of this study to examine the relationship between various aspects of optimal breastfeeding. E.g. the positioning of the baby at. The mothers’ breast. The positioning of the baby’s head and mouth. The dynamic and the latching process.95 healthy postpartum breast feeding mothers reported sore nipples within 10 days of giving birth to healthy term baby participated in the study. Four categories were scored and examined as related to the pain levels of the mother; the baby’s face position, the baby’s body position, the breast-feeding dynamic and the latching process of the baby. This study result shows no difference was found between the mother’s level of reported pain and the assessed head position, body position and breast-feeding dynamic attributes of the baby. More optimal latching process behavior of the baby is slightly related to lower levels of reported nipple pain. The investigator came across, Primipara mothers those who are Breastfeeding immediately after delivery they are not practicing proper breastfeeding techniques. So, they are more risk of getting nipple sore. This insisted me to take this study. The investigator felt that it is a need to educate mothers on proper breast feeding techniques to prevent nipple sore.
6.3 STATEMENT OF THE PROBLEM
A Study to assess the effectiveness of Structured Teaching Programme about Breast-feeding techniques on knowledge and practice in prevention of nipple sore among primi Para mothers in SC Hospital, Hassan.
6.4 OBJECTIVES 1.To assess the level of knowledge and practice before STP on breastfeeding techniques to prevent nipple sore in both groups.
2.To assess the level of knowledge and practice after STP on breast-feeding techniques to prevent nipple sore in both groups.
3. To evaluate the effectiveness of STP regarding breastfeeding techniques on knowledge and practice to prevent nipple sore.
4.To correlate the level of knowledge with practice in both groups.
5.To associate the posttest level of knowledge and practice with demographic variables in both group. 6.5 HYPOTHESES 1. There is a significant increase in the level of knowledge regarding breastfeeding techniques in prevention of nipple sore in the study group than the control group.
2. There is a significant change in the practice regarding Breastfeeding techniques in prevention of nipple sore in the posttest than the pretest in study group.
6.6 ASSUMPTION 1. Proper Breast-feeding techniques will improve bonding. 2. The knowledge will influence the attitude of mother regarding Breast-feeding techniques.
6.7 OPERATIONAL DEFINITION 1.ASSESSMENT; It is a method of estimating the level of knowledge regarding Breast-feeding techniques to prevent nipple sore among primipara mothers by comparing pretest and posttest. 2. EFFECTIVENESS. The difference in the level of knowledge after the STP in Breastfeeding techniques on knowledge and practice in prevention of nipple sore among primi Para mothers. 3. STRUCTURED TEACHING PROGRAMME. It is planned information regarding Breast-feeding techniques on knowledge and practice in prevention of nipple sore by using flashcards will be given to the group of primipara mothers in Post natal ward for 30 minutes by explanations. 4.BREASTFEEDING TECHNIQUES. The method or procedure of feeding Breast milk to the baby by the mothers. 5.KNOWLEDGE It is the information gained by the mothers regarding breast-feeding techniques being measured through questionnaires.
6. PRACTICE The performance of the primipara mothers on Breastfeeding techniques is assessed through checklist. 7.NIPPLE SORE The lesion of the nipple and pain feel by the mothers. 8. PRIMI PARA MOTHERS. A woman who has given birth to a baby that has reached the point of viability.
6.8 INCLUSION CRITERIA AND EXCLUSION CRITERIA INCLUSION CRITERIA 1.Primi Para mothers delivered through LSCS. 2.Mothers who are willing to participate in the study. 3.Mothers who delivered full term baby.
EXCLUSION CRITERIA 1. Mothers who are developed Breast complications and nipple problems. 2. Mothers who are affected by anesthetic complications. 3. Mothers who are affected by systemic diseases.
6.9 DELIMITATIONS 1.The sample size is limited to 30 experimental, 30 control group of primi Para mothers with LSCS. 2.The prescribed data collection is only 4 to 6 weeks.
6.10 CONCEPTUAL FRAME WORK The conceptual framework is based on Betty Neuman’s system theory. 6.11 REVIEW OF LITERATURE
STUDIES RELATED TO BREAST FEEDING TECHNIQUES
A true experimental study of Breast-feeding techniques in prevention of nipple sore conducted in India, Sir Ivan stedeford Hospital, Chennai (2002). Among 60 Primi postnatal mothers by means of convenience sampling. 30 experimental groups of mothers given an intervention (Structured Demonstration programme), 30 Control group of mothers no intervention. This study results showed the knowledge gain and skill gain in experimental group is high than control group and also nipple sore is high in control group than the experimental group.1
A cross sectional study conducted on Knowledge, attitude and practice of breastfeeding in the north of Jordan (2003). Among 344 women with children aged between 6 months and 3 years from five different village, randomly selected and interviewed. Information regarding participant’s demographics, infant feeding in six months of life, knowledge and attitude towards breast-feeding was collected. This study results shown that full breast- feeding was reported by 58.3%, mixed feeding was reported by 30.3%. Almost 1/3 of the full breast-feeding group did so for 6-12 months, and almost 2/3 did continue breast- feeding for more than one year. Employed women were more likely not to practice full breast-feeding compared to unemployed women and women who had caesarian delivery were more likely not to practice full breast-feeding compared to those who had vaginal delivery. This study recommended that adopting facilitatory measures at hospital and work place could increase the rate of full breast-feeding.2 A study of Multiprofessional training for Breast-feeding management in primary care was conducted in UK (2006). Six U.K general practitioned practices were involved in a questionnaire survey of multi professional groups before and after and interactive training session. This focused on managing and solving problem. This study results shown that 50 primary care health professionals attended the session. There was an increased in scores relating to knowledge about breast-feeding after training. The health visitors improved their scores and recognition of the symptoms of poor attachment at the breast. This study recommended using an electronic teaching resource is feasible for updating the knowledge of the primary care team.10
STUDIES RELATED TO BREAST COMPLICATIONS DUE TO IMPROPER BREAST FEEDING TECHNIQUES: A study of views of breastfeeding difficulties among drop-in-clinic attendees conducted in UK (2005), Liverpool john moors university liver pool. The aim of the present study was to describe breast-feeding difficulties reported by women who attended the infant feeding clinic at a women’s hospital in the North-West of England. During the study period the clinic was attended mainly by primiparous mothers who were educated beyond 18 years of age and of higher socio-economic status. They presented with variety of problems including baby not latching on, concerns about baby’s weight gain or loss. Sore nipples and advice about expressing milk in preparation for return to work. This study concluded that many women felt they were able to continue breastfeeding but without the support.3
A prospective cohort study of Breastfeeding as well as breast feeding problems of mothers in Bavaria was conducted in German (2005) The frequency of breast feeding exclusively according to needs at 2-6 days following delivery was about 62%. At the end of the infants second month of life only 46.7% of the infants were breast feed at least 7 times. In the first two months the prevalence of breast-feeding problems in mothers who still breast feed and those who had stopped was about the same. In mother-infants pairs who no longer breast-feed, Sore nipples and drinking or suckling problems of the infant predominated.4
A study of Breast feeding problems related to incorrect Breastfeeding techniques and the use of pacifiers and bottles was conducted in Western countries (Sweden) (1998) Fifty-two healthy mothers infant pairs with Breast feeding problems were referred for observation of nursing behaviors to a Breast feeding clinic and the Department of pediatric of malmo general hospital. The infants ranged in age from 1 to 17 weeks. A faulty nursing pattern was corrected as necessary. 40 mother-infant pairs with no breast- feeding problems provided a control group. The study results shown that in most cases the nursing problems were related to incorrect suckling techniques. The different technique of the study group compared with control group was significant (p=0.0001). This study concluded Breast-feeding problems may be prevented by the adoption of hospital routines that do not interfere with the start of Breast-feeding and to by the avoidance of extensive use pacifiers.5
A Randomized trial study conducted on nipple care, sore nipples and Breast feeding in Italy (1999) among 96 control group of mothers given routine nipple care including ointments and 123 intervention group of mothers to avoid the use of nipple creams and other products. Breast-feeding duration also compared between the 2 groups. The study results shows that no difference was found between the control and the intervention group in the incidence of sore and crack nipples and breast feeding duration. The study recommends that providing the mother and guidance and support on positioning and latching and modification of hospital practices may be more effective the reducing nipple problems.6
A Cross sectional survey study of the prevalence of nipple disease among breast feeding mothers of HIV 0 positive infants was conducted in Zimbave. One Hundred and four symptomatic HIV 0 positive Breast feeding infants and their mothers. This Study results shown that the prevalence of nipple problems was high (30.8%). Nipple eczema was seen in (22.1%). The crack nipples in 10.6% and sore nipple diseases in the mother if the infant had oral disease were 11.47 (95%). There was no significant association between nipple diseases, and mother’s age, infant’s age. This study concluded Nipple diseases were highly prevalent and oral diseases were the major risk factors for the development of nipple diseases in Breast-feeding HIV 0 positive mothers.7 A study of Randomized clinical trial compared frequencies of exclusive Breast-feeding and lactation related problems during the first 30 days was conducted in Brazil (2006). Among 74 mothers who received a 30 minutes counselling session on Breast-feeding techniques in the maternity ward and 137 controls. The frequency of exclusive breast- feeding among mothers who had received intervention was similar to controls by 7 days. (79.7% Vs 82.5% respectively) and 30 days (60.8% Vs 53.3%). There was no different between groups in the frequency of sore nipple at 7 and 30 days in breast engorgement and mastitis. This study concluded a single intervention at maternity was not sufficient to improve breast-feeding technique. Increase exclusive breast-feeding rates and reduce the incidence of Breast-feeding problems during the first month.8
A study of Ankyloglossia in Breast feeding infants can cause ineffective latch, inadequate milk transfer, and maternal nipple pain resulting in untimely weaning was conducted in USA (2002). They examine 2763 breast-feeding inpatients infants and 273 outpatient infants with breast-feeding problems for possible ankyloglossia. This study results shown Ankyloglossia was diagnosed 88 (3.2%) of the inpatients and in 35 (12.8%) of the outpatients. The score were similar for presenting symptoms of poor latch and nipple pain. Ankyloglosssia is a relatively common finding in the newborn population and represents a significant proportion of breast-feeding problems. Poor infant latch and maternal nipple pain are frequently associated with these findings.9
A study conducted on causes, treatment and prevention of nipple pain in breast-feeding women in (2000). This article identifies problems and conditions that contribute to nipple pain during lactation and that may lead to early session of breast-feeding. Signs and symptoms of poor latch on and positioning. Oral anomalies and suckling disorders are reviewed. Diagnosis and treatment of infectious agents that may cause nipple pain are presented. Comfort measures for sore nipples and current treatment recommendations for nipple wound healing are discussed. The suggestions are made for incorporating in depth breast-feeding content in to midwifery education programmes.11 A study of randomized double blinded clinical trial of to formulate a peppermint gel and to evaluate its effect on the prevention of nipple crack associated with breast-feeding was conducted in Tabriz Iran (2007). 210 Primiparas participants were assigned randomly to 3 groups. Each group applied only 3 one of the above.3 participants on both breast for 14 days. Each group consisted of 72 primiparas’ mothers and was seen for a maximum of four followed up visits within 14days and a final visit at week six. This study Results shown Nipple crack were less in mothers who received peppermint gel than in those who received lanolin ointment or placebo. Relatively risk of nipple crack in the lanolin group was higher than in the peppermint group. This study concluded the prophylactic peppermint gel in Breast-feeding lactating women is associated with small number of nipple cracks and is more effective than lanolin and placemo. It could be recommended for preventing of nipple crack along with teaching with better breastfeeding technique at the initiation of breastfeeding.12
7 MATERIALS AND METHODS OF STUDY
SOURCE OF DATA The data will be collected from the primipara mothers of S.C Hospital at Hassan.
RESEARCH DESIGN
The research design adopted for the study is True experimental design. A true experiment is characterized by the following properties. 1.Manipulation. 2.control. 3.Randomisation. GROUPS PRETEST INTERVENTION POSTTEST
Experimental group Primi post natal 01 X 02 mothers, SC Hospital, Hassan
Control group 01 - 02
Key: 01 – pretest on knowledge and practice regarding breast-feeding techniques In prevention of nipple sore. 02 – post test on knowledge and practice regarding breast-feeding Techniques in prevention of nipple sore. X - Structured demonstration regarding breastfeeding techniques to Prevent nipple sore.
7.1 METHOD OF DATA COLLECTION Using close-ended questionnaires.
POPULATION: All primi Para mothers admitted in LSCS ward of S.C Hospital, Hassan.
SAMPLES: Primi Para mothers those who are fulfilling the sampling criteria. SAMPLE SIZE Sample comprises of 30 experimental and 30 control groups of primipara mothers in SC Hospital, Hassan.
SAMPLING TECHNIQUES Probability sampling- Simple Random method. SETTING The study will be conducted in SC Hospital at Hassan.
PILOT STUDY. Pilot study has planned with the 10% of population.
8. VARIABLES: 8.1 INDEPENDENT VARIABLE In this study the independent variable is structured teaching programme regarding breast-feeding techniques in prevention of nipple sore.
8.2 DEPENDENT VARIABLE In this study dependent variable is knowledge and practice regarding breast-feeding techniques in prevention of nipple sore.
9. PLAN FOR DATA ANALYSIS: Descriptive analysis: Demographic information’s, level of knowledge and level pf practice score will be given in frequencies with their percentages. Knowledge score and skill score will be given in mean and standard deviations. Inferential analysis: Pre-test and post-test differences will be analyzed using student paired t-test and Mcnomars test. Experimental and control group differences will be analyzed using student independent t-test. Co-relation between knowledge score and practice score will be analyzed using pearson corelation coefficient.
Association between level of knowledge and level of practice and their demographic variables are analyzed using pearson chisquare test.
10 ETHICAL CONSIDERATIONS 1.Does the study require any intervention to be conducted on primi postnatal mothers in SC Hospital, Hassan? Yes. 2.Has ethical clearance being obtained from institution? Yes. 11. LIST OF REFERENCE: 1. Vijayalakshmi s. Raman Breast feeding technique in prevention of nipple sore. Nursing journal India.2002. Aug: 93(8). 2. Mohammad khassawneh. Knowledge, attitude, and practice of breast-feeding in the north of Jordan. 2006. 3. Berridge k. Breastfeeding difficulties among drop in clinic attendees.2005.Liver pool John Moore University. Liver pool. U.K. 4. Rebhan B.Breast feeding frequency and problems. 2008. March: 70. 1:S8-S12. Related Articles. German. 5. Rig hard L. Breast feeding problems related to incorrect breast-feeding technique and the use of pacifiers and bottles.1998.University of London university hospital. Sweden. 6. Centuori S. Nipple care, sore nipples, and Breast-feeding. 1999 June: 15 (2). Italy. 7. Kambarami. The prevalence of nipple disease among Breast-feeding mothers of HIV Seropositive infants. 1998. Department of pediatrics and child health. Zimbabwe. 8. De oliveira LD. Effect of intervention to improve Breast-feeding. techniques on the frequency of exclusive breastfeeding and lactation related problems. 2006. Brazil. 9. Ballard JL. Ankyloglossia Assessment, incidence and effect of frenuloplasty on the Breast-feeding dyad. 2002 Nov: 110(5). Page no.63. USA. 10. Ingram J. Multi professional training for breast-feeding management in primary care.2006.center for child and adolescent Health. University of Bristol. UK. 11. Tait p. Midwifery womens Health Article, Nipple pain in Breast feeding women: causes, treatment, and prevention strategies. 2000.may-Jun: 45(3). 12. Mr. Nokhoodchi. A Randomized trial of peppermint gel, lanolin ointment. 2007. Tabriz university of medical sciences. Tabriz Iran.
13 Signature of the Candidate
Good Methodology, Intervention is 14. Remarks of the Guide appreciated
Prof. Susila M.Sc.,(N) 15. Name & Designation of Guide Department of Obstetrics & Gynecological Nursing Rajeev College of Nursing Hassan, Karnataka
15.1 Guide
15.2 Signature
Prof. Susila M.Sc.,(N) 15.3 Head of the Department Department of Obstetrics & Gynecological Nursing Rajeev College of Nursing Hassan, Karnataka
15.4 Signature
16 Remarks of the Principal
16.1 Signature