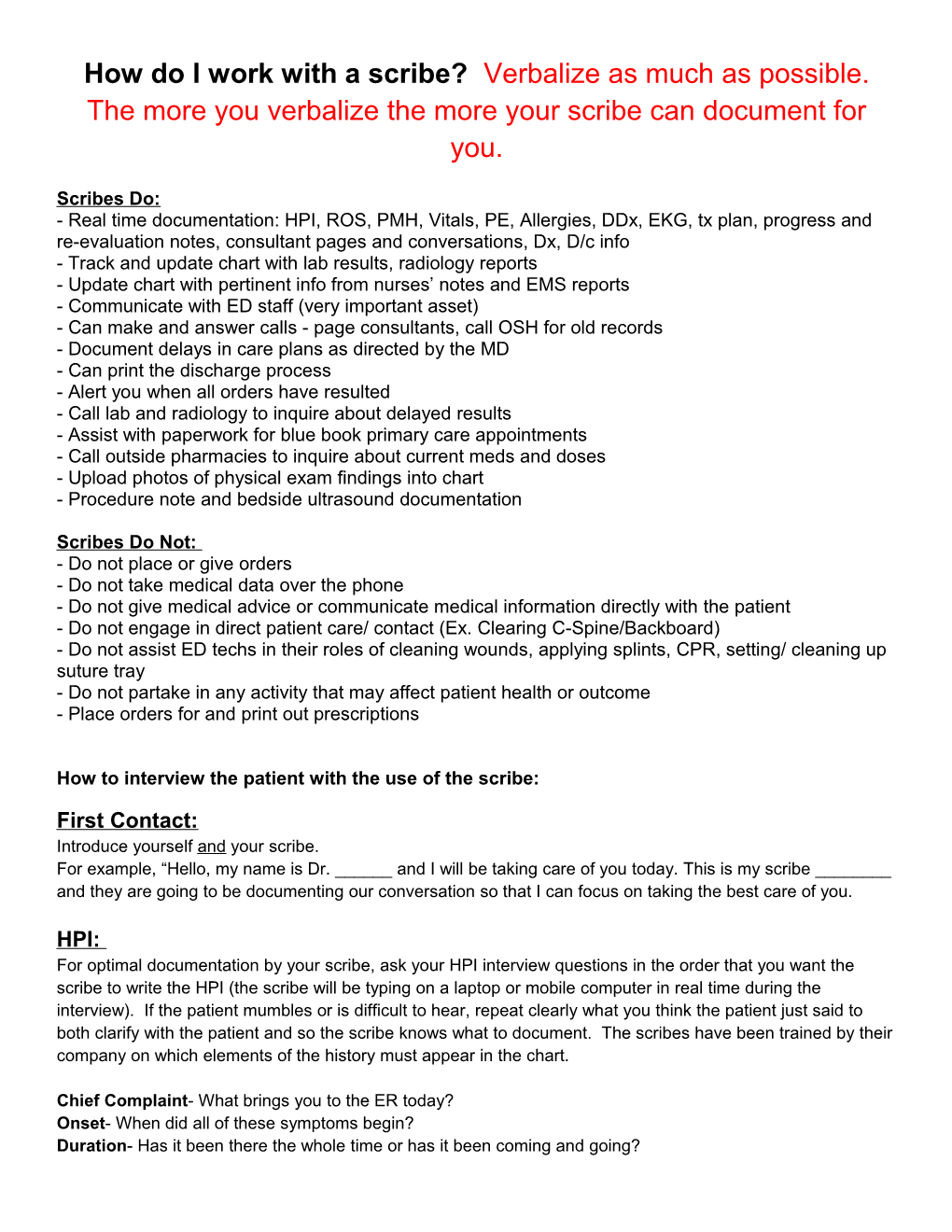
How do I work with a scribe? Verbalize as much as possible. The more you verbalize the more your scribe can document for you.
Scribes Do: - Real time documentation: HPI, ROS, PMH, Vitals, PE, Allergies, DDx, EKG, tx plan, progress and re-evaluation notes, consultant pages and conversations, Dx, D/c info - Track and update chart with lab results, radiology reports - Update chart with pertinent info from nurses’ notes and EMS reports - Communicate with ED staff (very important asset) - Can make and answer calls - page consultants, call OSH for old records - Document delays in care plans as directed by the MD - Can print the discharge process - Alert you when all orders have resulted - Call lab and radiology to inquire about delayed results - Assist with paperwork for blue book primary care appointments - Call outside pharmacies to inquire about current meds and doses - Upload photos of physical exam findings into chart - Procedure note and bedside ultrasound documentation
Scribes Do Not: - Do not place or give orders - Do not take medical data over the phone - Do not give medical advice or communicate medical information directly with the patient - Do not engage in direct patient care/ contact (Ex. Clearing C-Spine/Backboard) - Do not assist ED techs in their roles of cleaning wounds, applying splints, CPR, setting/ cleaning up suture tray - Do not partake in any activity that may affect patient health or outcome - Place orders for and print out prescriptions
How to interview the patient with the use of the scribe:
First Contact: Introduce yourself and your scribe. For example, “Hello, my name is Dr. ______and I will be taking care of you today. This is my scribe ______and they are going to be documenting our conversation so that I can focus on taking the best care of you.
HPI: For optimal documentation by your scribe, ask your HPI interview questions in the order that you want the scribe to write the HPI (the scribe will be typing on a laptop or mobile computer in real time during the interview). If the patient mumbles or is difficult to hear, repeat clearly what you think the patient just said to both clarify with the patient and so the scribe knows what to document. The scribes have been trained by their company on which elements of the history must appear in the chart.
Chief Complaint- What brings you to the ER today? Onset- When did all of these symptoms begin? Duration- Has it been there the whole time or has it been coming and going? Timing- Did it come on all of a sudden or gradually? Severity- On a scale of 1-10 what would you rate your pain? Quality- What does it feel like? Location- Where is your discomfort? Associated Symptoms- List specific symptoms pertinent to the complaint Modifying Factors- Does anything make it better or worse? Context- Did you take anything for the pain?
ROS: When starting your shift with a scribe, if you have not worked with that certain scribe before, make sure that they are aware of your standard ROS questions. * Create a phrase that you would be comfortable asking every patient “Do you have any fever, chills, SOB, cough, CP, N/V/D, Abd pain, urinary symptoms, or headache?” Before beginning the exam, close your interview with “Is there anything else bothering you today?” Residents, it is best to help the scribe create a macro that encompasses all of your standard questions. Attendings, show the scribe your standard ROS that you include in your addendum. - The biggest challenge for scribes is not having enough information to document a Level 5 charts. They are instructed to only document the questions the physician asks
Physical Exam: Our scribes observe at bedside while you perform the patient’s physical exam. Some physicians verbalize findings while doing the exam, others wait and verbalize their findings once outside the room. To avoid frequent repetition many physicians choose to only mention the abnormal findings. For example, “The exam is benign except for some mild LUQ tenderness.”
Like with the ROS, clarify with the scribe when you begin working together what your normal benign physical exam is. For residents, this involves having the scribes make a macro, and for attendings this could be showing them your normal exam that you have in your standard attending addendum.
For optimal charting, verbalizing your exam out loud as you are performing it is recommended. This will allow the scribe to have a majority of the documentation completed before you exit the room allowing you to move on to the next patient to be seen. The patient also feels that they are getting a thorough and complete exam, which will help with overall patient satisfaction
As soon as you exit the patient’s room ask your scribe the following questions: 1. Do you have any questions or would you like me to repeat anything? 2. Tell them your Differential Diagnoses 3. Tell them your treatment plan and medical decision making- Obtain labs and CT to evaluate for -----, administer IV fluids, pain meds, anti-emetics and reassess
ED Course:
Inform your scribe when you are getting ready to go see a patient. If you need to do a few more things before going in the room (wait for a phone call, enter orders etc), your scribe can go find the clipboard and EKG if already done, and begin documenting the EKG, vitals and other info from the paper chart before entering the room. You can also have your scribe look up certain info about a patient before going into a room (for example if going to see a CP pt with known CAD, ask the scribe to pull up the last cath report for you). For residents going to see multiple patients at a time, it can work well for you and your scribe to go see the first patient, then exit the room and stop by one of the computers. The resident can quickly place orders, and the scribe can finish up typing on the chart. Then move on to the next patient.
After seeing the patient, instruct your scribe to document all components of your treatment plan.
1. Laboratory Orders
- Scribes will closely monitor results throughout the patient’s ED stay and update the chart accordingly.
-Please inform your scribe if you order any additional lab tests later to ensure documentation and close follow up.
-Scribes can call the lab to ask about the problem with results that are taking too long.
2. Radiology Studies
-Scribes can monitor progress of patients going to radiology to get studies, and can inform the physician if it has been a long time and the patient has not gone for the study
-Scribes can call to the reading room to ask for studies that are taking a long time to be read
-Scribes copy reads in to chart once they are complete and inform physician as soon as read is available.
3. Medications Ordered
-Scribes will document all medications ordered initially
-Scribes will document progress notes that include further doses of medications ordered when patients’ symptoms are not relieved with initial medication.
4. EKGs
-Scribes will find EKGs, document time and rate, then ask physician for interpretation to document
5. Vital signs
-Scribes will document vital signs if not in computer on initial physical exam
-Scribes will document vital signs from pre hospital EMS documentation if pertinent
-Scribes will document vital signs multiple times in progress notes
6. Procedures (Non-Critical Care)
- Scribes have been taught how to document procedure notes using the procedure section in Cerner. They have been instructed to document in the room during the procedure completion. Please verbalize your findings out loud so that the documentation can be completed as “real-time documentation” for a quick disposition.
-Inform your scribe once you plan to start the procedure so that they are prepared to begin documenting and are present at the start of the procedure or you can give them the details after the procedure if that saves time
-Please allow your scribe to witness procedures. A majority of the scribes are interested in the medical field and would like to have the opportunity for the learning experience.
7. Procedures (Critical Care) -Scribes have been instructed to take notes on a separate sheet of paper once a patient arrives into the ED if they have not been registered before documentation begins. The scribe will become a “fly on the wall” in the room while codes, intubations, and other resuscitations are being performed. They will document the clinical events as they unfold allowing you to focus on caring for the patient.
-During traumas, scribes will pay close attention to EMS reports to document the mechanism of trauma, including details that are often difficult to hear when the resident and attending are immediately focusing on patient care
8. Re-Evaluations
-Scribes have been instructed to prompt the physicians to complete a re-evaluation note on every patient they see.
-If the physician performs a re-eval without the scribe, please verbalize your findings out loud to the scribe. Ex: “I re-evaluated room 8. Pt in NAD. Feeling better. Respiratory exam improved. Wheezing resolved. Pt stable for discharge with PCP follow up”.
-Physicians can ask the scribe to go to the monitor and document a current set of vital signs
9. Critical Care- Scribes have been instructed to ask the physicians if their patients qualify for Critical Care time. They are well educated on the criteria that qualify for Critical Care time.
Dispositioning:
The scribe will notify the physician once all of the orders are completed or vice versa, and scribe will be prepared to document the discharge process.
-Scribes can fill out the Impression and Plan section of the chart. Tell them the dx, which patient education sheet you would like, and follow up clinic or provider. Dictate any special instructions you would like typed on the follow up section, and tell them if the patient needs a work note or financial screening information. If consultants call you back with follow up info, relay that information to the scribe and have them take down the info and immediately put it in the chart.
-Scribes will place an attestation identifying them as the person who documented the information for the resident or the attending.
We intend to provide scribes with macros for each attending’s standard addendum, so that they can begin the documentation for the atttending while scribing for the third year resident.
Scribe Priority:
When multiple faculty and residents are present in a clinical area, and not enough scribes are scheduled to accommodate all providers, the order of scribe utilization shall be by seniority: 1. Faculty
2. EM3 (EM/IM4 or 5)
3. EM2 (EM/IM 2 or 3)
Faculty in mainly a supervisory role should defer scribe use to the senior resident on duty in most circumstances.
When two providers are in a clinical area of the same seniority, scribe use will defer to provider on in the following order based on shift assignment:
1. 9p-7a
2. 7a-5p
3. 5p-3a
4. 12p-10p
5. 9a-7p
If the scribe is not actively in use, he/she may be shared with another qualified provider to assist in documentation. This should not jeopardize the quality of efficiency of the work done for the senior provider. Scribes are not to be used by unapproved providers, EM1’s (EM/IM1), off-service residents, or students.