Symptom Management Guidance to be used with Care Pathway for the Last Days of Life-V2.00-0266-GUI-CHOSPDCHS Version No 3 Version Date 9/09/13 Review Date 09/09/2013
SYMPTOM MANAGEMENT GUIDANCE PALLIATIVE CARE PAIN
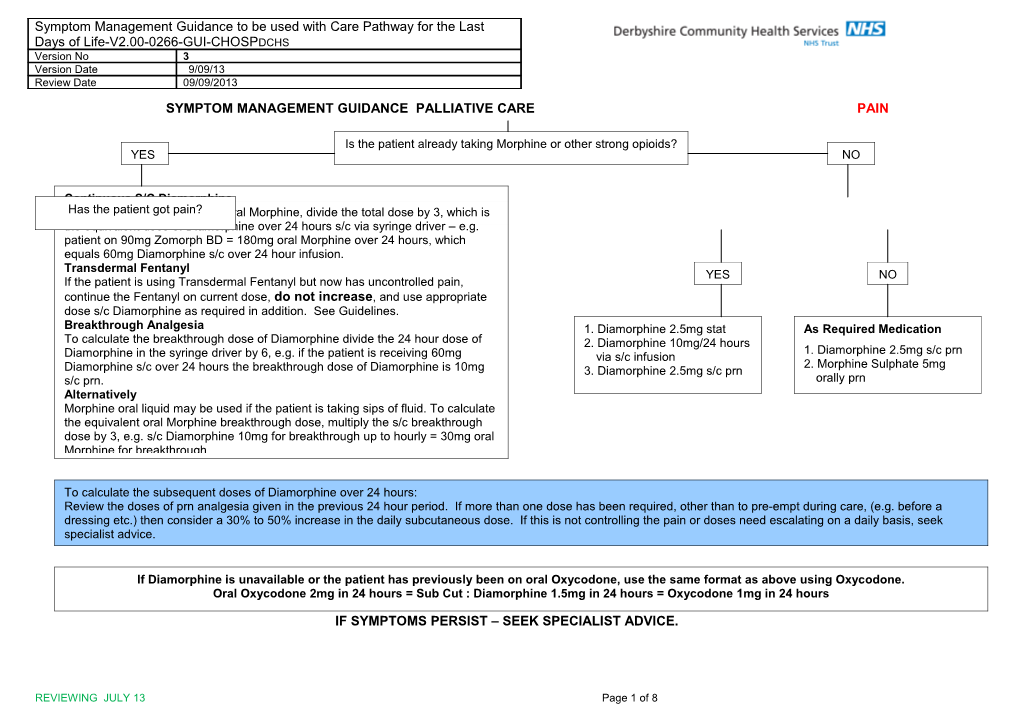
Is the patient already taking Morphine or other strong opioids? YES NO
Continuous S/C Diamorphine CalculateHas the patient the 24 gothour pain? dose of oral Morphine, divide the total dose by 3, which is the equivalent dose of Diamorphine over 24 hours s/c via syringe driver – e.g. patient on 90mg Zomorph BD = 180mg oral Morphine over 24 hours, which equals 60mg Diamorphine s/c over 24 hour infusion. Transdermal Fentanyl YES NO If the patient is using Transdermal Fentanyl but now has uncontrolled pain, continue the Fentanyl on current dose, do not increase, and use appropriate dose s/c Diamorphine as required in addition. See Guidelines. Breakthrough Analgesia 1. Diamorphine 2.5mg stat As Required Medication To calculate the breakthrough dose of Diamorphine divide the 24 hour dose of 2. Diamorphine 10mg/24 hours 1. Diamorphine 2.5mg s/c prn Diamorphine in the syringe driver by 6, e.g. if the patient is receiving 60mg via s/c infusion 2. Morphine Sulphate 5mg Diamorphine s/c over 24 hours the breakthrough dose of Diamorphine is 10mg 3. Diamorphine 2.5mg s/c prn s/c prn. orally prn Alternatively Morphine oral liquid may be used if the patient is taking sips of fluid. To calculate the equivalent oral Morphine breakthrough dose, multiply the s/c breakthrough dose by 3, e.g. s/c Diamorphine 10mg for breakthrough up to hourly = 30mg oral Morphine for breakthrough.
To calculate the subsequent doses of Diamorphine over 24 hours: Review the doses of prn analgesia given in the previous 24 hour period. If more than one dose has been required, other than to pre-empt during care, (e.g. before a dressing etc.) then consider a 30% to 50% increase in the daily subcutaneous dose. If this is not controlling the pain or doses need escalating on a daily basis, seek specialist advice.
If Diamorphine is unavailable or the patient has previously been on oral Oxycodone, use the same format as above using Oxycodone. ForOral further Oxycodone information, 2mg in including 24 hours if = CKD Sub Cut4 or : 5, Diamorphine see the Dose 1.5mg Equivalence in 24 hours Guidance = Oxycodone Chartpages 1mg in 247 & hours 8. IF SYMPTOMS PERSIST – SEEK SPECIALIST ADVICE.
REVIEWING JULY 13 Page 1 of 8 RETAINED SECRETIONS
Present Absent
1. Explain to relatives that for the patient retained As required medication secretions are not bothersome due to decreased sensitivity of pharynx. Hyoscine Butylbromide 20mg s/c - Maximum dose up to 80mg in IF the relatives are concerned or the patient 24hrs appears distressed:
2. Hyoscine Butylbromide 20mg s/c stat. 3. Hyoscine Butylbromide 60mg / 24 hours via s/c Infusion. 4. Hyoscine Butylbromide 20mg s/c hourly prn - Maximum dose up to 80mg in 24hrs
IF SYMPTOMS PERSIST – SEEK SPECIALIST ADVICE
REVIEWING JULY 13 Page 2 of 8 TERMINAL RESTLESSNESS AND AGITATION
Present Absent
1. Exclude Treatable Causes Pain As Required Medication Retention of urine or faeces Haloperidol 2.5mg s/c prn– up to Hypercalcaemia if it would be appropriate to treat hourly (maximum including syringe driver dose 15mg in
2a. Delirium 2b. Anxiety / Dyspnoea 24hrs) i. Haloperidol 2.5mg stat. i. Midazolam 2.5mg s/c stat. ii. Haloperidol 5mg/24 hours ii. Midazolam 10mg / 24 hrs via s/c infusion. via s/c infusion. iii. Haloperidol 2.5mg s/c prn iii. Midazolam 2.5mg s/c prn– one hourly for maximum of 3 doses, then seek medical Review in 24 hours advice. Review Every 24 Hours Increase the dose of Haloperidol to 10mg / 24 Review every 24 hours hours via s/c infusion if Increase the 24 hour dosage necessary. according to the total dose of NB: A total dose of 15mg / 24 Midazolam given on a prn hours – including stat dose, basis. The dose should not be continuous dose and prn increased by more than doses should not be 10mg/day without specialist exceeded. advice
IF SYMPTOMS PERSIST – SEEK SPECIALIST ADVICE
REVIEWING JULY 13 Page 3 of 8 NAUSEA
Previously on Anti-Emetic NO YES
Nausea Convert to s/c as appropriate YES present NO
1. Haloperidol 1.5 – 2.5mg s/c stat. Prescribe, so available 2. Haloperidol 5mg via s/c infusion. if needed, Haloperidol 3. Haloperidol 1.5 – 2.5mg s/c prn. 1.5 – 2.5mg s/c prn (up to a total of 15mg / 24 NB: A total of 15mg / 24 hours – hours) including stat doses, continuous s/c doses and prn doses – should not be exceeded.
Review in 24 hours
Increase to 10mg / 24 hours s/c if nausea persists
For persistent nausea switch to: 1. Levomepromazine 6.25mg / via s/c infusion. 2. Levomepromazine 6.25mg prn s/c.
NB: A total of 50mg / 24 hours – including continuous and prn doses – should not be exceeded.
IF SYMPTOMS PERSIST – SEEK SPECIALIST ADVICE
REVIEWING JULY 13 Page 4 of 8 TERMINAL BREATHLESSNESS
YES
Absent Present
Prescribe so available if needed: Previously on oral Opioid or Diamorphine 2.5mg (or if on regular Fentanyl patch Opioids dose as per equivalence chart) s/c hourly for Tachypnoea. Midazolam 2.5-5mg s/c hourly for distress Give as soon as possible appropriate prn of: Diamorphine s/c (see equivalence chart) for YES NO Convert to s/c pump (or in case of Fentanyl patch add CSCI, DO NOT REMOVE Tachypnoea. PATCH) following Guidelines for Pain Management, BUT consider increasing Midazolam 2.5-5mg s/c if patient distressed Opioid dose, e.g. give 30-50% more than the recommended equivalent dose (or for Transdermal Fentanyl add 30-50% of the equivalent dose). Give as soon as possible: Prescribe appropriate prn as for breakthrough pain, e.g.1/6th of total daily dose Diamorphine 2.5mg s/c hourly for Tachypnoea. Diamorphine for Tachypnoea. Midazolam 2.5-5mg s/c hourly for distress. If no relief 30 minutes after first drug, try alternative, Prescribe Midazolam 2.5-5mg s/c hourly prn for distress caused by repeating if necessary. breathlessness – hourly for a maximum of 3 doses then seek medical advice
Consider adding Midazolam 10mg to s/c pump, particularly if prn dose has helped. If repeated doses are needed, consider starting syringe driver with combination of Diamorphine and Midazolam. Suggested starting doses are 5mg of each over 24 hours. Remember to use AIM for patient’s breathing to be calm and effortless prns as needed.
IF SYMPTOMS PERSIST – SEEK SPECIALIST ADVICE. If CKD 4 or 5, see the Dose Equivalence Guidance Chart, page 7 & 8
REVIEWING JULY 13 Page 5 of 8 GUIDELINES FOR CARE OF DIABETES IN PATIENTS IN THE LAST FEW DAYS OF LIFE
Aim of treatment is to avoid symptoms of hyperglycaemia and hypoglycaemia Practical points:-
1. In Type 2 diabetes insulin and oral agents can usually be stopped in the terminal phase; steroid treated patients may be an exception.
2. Blood glucose monitoring should be kept to the minimum necessary.
3. It is important to ensure clinical deterioration not due to hyperglycaemia or hypoglycaemia before making decisions re management.
4. Regular review of the patient and management plan is necessary, due to difficulties with prognostication of death and varying terminal phase.
5. If death imminent i.e. expected in less than 24 hours it may be appropriate to discontinue all monitoring and insulin, usually after discussion with the family.
6. SEEK SPECIALIST ADVICE EARLY
Community Diabetes Specialist Nurse
Monday to Friday, in office hours, usually 9am to 5pm
REVIEWING JULY 13 Page 6 of 8 Tel 01629 817878 Mobile 07884415168 or 07900584162
Out of Hours Ashgate Hospice Tel 01246 568801
Further information also available at http://www.trend-uk.org/documents
PALLIATIVE CARE DOSE EQUIVALENCE GUIDANCE CHART, Page 7 & 8
Bupren- Morphine Zomorph or MXL o.d. Oxycodone Oxycodone Oxycodone Diamorphin Diamorphin Fentanyl orphine patch 4 hourly MST 12 immediate MR s/c in 24 e s/c 4 e s/c in 24 patch 72 per hour po hourly po release 12 hourly hours hourly hours hourly po 4 hourly po po 5mg 15mg 30mg 2.5mg 5-10mg 5-10mg 2.5mg 10mg 6mcg 5mcg 7.5 20mg 40mg 2.5mg 10mg 10mg 2.5mg- 15mg 12mcg 10-20mcg
10mg 30 mg 60 mg 5 mg 15 mg 15 mg 5 mg 20 mg 12-25 mcg 35mcg 15mg 40mg 90mg 7.5 20mg 20mg 5mg 30mg 25mcg 35mcg
20 mg 60 mg 120 mg 10 mg 30 mg 30mg 7.5mg 40 mg 37mcg 52.5mcg
30 mg 90 mg 180 mg 15 mg 45 mg 45 mg 10 mg 60 mg 50 mcg 70mcg Suggest use 40 mg 120 mg 240 mg 20 mg 60 mg 60 mg 15 mg 80 mg 62mcg Fentanyl Patch
“ 50 mg 150 mg 300 mg 25mg 75 mg 75 mg 20 mg 100 mg 75 - mcg
60 mg 180 mg 360 mg 30 mg 90 mg 90mg 20 mg 120 mg 100 mcg “
70 mg 200 mg 400 mg 35 mg 100 mg 100mg 20 mg 140 mg 125 mcg “
80 mg 240 mg 480mg 40 mg 120 mg 120 mg 30 mg 160 mg 125-150 mcg “
90 mg 260 mg 540 mg 45 mg 130 mg 130mg 30 mg 180 mg 150 mcg “
100 mg 300 mg 600 mg 50 mg 150 mg 150mg 30 mg 200 mg -175 mcg “
110 mg 330 mg 660 mg 55 mg 160 mg 160mg 40 mg 220 mg 175 mcg “
REVIEWING JULY 13 Page 7 of 8 120 mg 360 mg 720 mg 60 mg 180 mg 180mg 40 mg 240 mg 200 mcg “
140 mg 420 mg 840 mg 70 mg 200mg 200mg 50 mg 300 mg 250 mcg “
160 mg 480 mg 960 mg 80 mg 240 mg 240mg 50mg 330 mg -275 mcg “
180 mg 540 mg 1080 mg 90 mg 250 mg 250 mg 60 mg 360 mg 300 mcg “
Tramadol po100mg = 10mg po Morphine. Tramadol po 100mg qds ie 400mg/24 hours = Morphine po 40mg/24 hours Suggested breakthrough dose of po Morphine =7.5mg 4 hourly
These doses are only approximate and the dose may need to be adjusted A patient may be routinely missing dose(s) e.g. night dose of 4 hourly regime so accordingly to responses. check recent totals over 24 hours for this and prn regimes. Breakthrough analgesia, dose of Opioid should be ONE SIXTH of the total daily For patients with known CKD 4 or 5 adjust doses accordingly and seek specialist dose (dose over 24 hours). This is the same as the four hourly dose. help if needed. Repeat routine testing of U&E’s in last days of life need not be done.
Immediate Release Preparations Slow Release Preparations Diamorphine Injections Fentanyl Patches Sevredol tablets 10, 20, 50mg MXL 30, 60, 90, 120, 150, 200mg 5, 10, 30, 100, 500mg 12, 25, 50, 75, 100mcg/hr Morphine Sulphate liquid Zomorph 10, 30, 60, 100, 200mg 10 mg/5ml e.g. Oramorph 100mg/5ml, MST 5, 10, 15, 30, 60,100, 200mg Oxycodone Injection Buprenorphine Patches e.g. Oramorph concentrate Oxycodone MR 5, 10, 15, 20, 40, 60, 80, 10mg/ml. 20mg/2ml 5, 10, 20mcg/hr (seven day patches) Oxycodone capsules 5, 10, 20mg, e.g. 120mg e.g. Oxycontin 35, 52.5, 70mcg/hr (four day patches) Oxynorm Oxycodone liquid 5mg/5ml, 50mg/5ml, e.g. Oxynorm
References:- Palliative Care Formulary (PCF4). Fourth Edition. ISBN: 978-0-9552547-5-8. Editors: Robert Twycross Andrew Wilcock Summary of Product Characteristics:- Oxynorm Injection. Napp Pharmaceuticals, EMC updated 22/06/2013; Oxycodone injection, Wockhardt UK Ltd EMC Updated 14/01/2011. British National Formulary (BNF) 65 March-September 13
REVIEWING JULY 13 Page 8 of 8