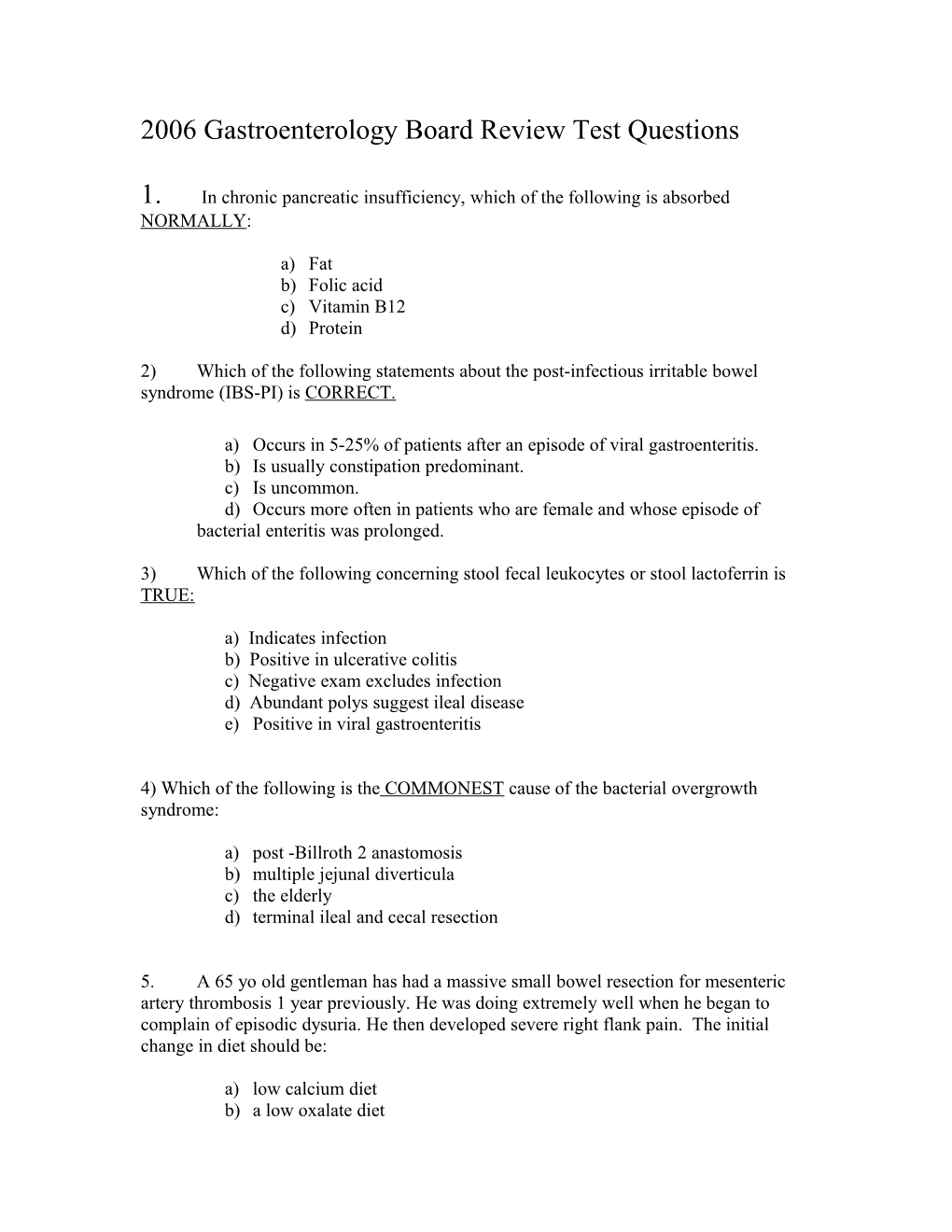
2006 Gastroenterology Board Review Test Questions
1. In chronic pancreatic insufficiency, which of the following is absorbed NORMALLY:
a) Fat b) Folic acid c) Vitamin B12 d) Protein
2) Which of the following statements about the post-infectious irritable bowel syndrome (IBS-PI) is CORRECT.
a) Occurs in 5-25% of patients after an episode of viral gastroenteritis. b) Is usually constipation predominant. c) Is uncommon. d) Occurs more often in patients who are female and whose episode of bacterial enteritis was prolonged.
3) Which of the following concerning stool fecal leukocytes or stool lactoferrin is TRUE:
a) Indicates infection b) Positive in ulcerative colitis c) Negative exam excludes infection d) Abundant polys suggest ileal disease e) Positive in viral gastroenteritis
4) Which of the following is the COMMONEST cause of the bacterial overgrowth syndrome:
a) post -Billroth 2 anastomosis b) multiple jejunal diverticula c) the elderly d) terminal ileal and cecal resection
5. A 65 yo old gentleman has had a massive small bowel resection for mesenteric artery thrombosis 1 year previously. He was doing extremely well when he began to complain of episodic dysuria. He then developed severe right flank pain. The initial change in diet should be:
a) low calcium diet b) a low oxalate diet c) a low fat diet d) no change in diet
6. Which of the following is the MOST COMMON cause of intractability to therapy of celiac sprue:
a) Continued gluten intake b) collagenous sprue c) lymphoma d) viral gastroenteritis e) microscopic colitis
7. Which of the following GI infections should be treated with antibiotics?
A. E. coli 0157:H7 B. Shigellosis C. Campylobacter D. Salmonella
8. Which histologic features favor a diagnosis of ulcerative colitis over infectious colitis?
A. Normal crypt architecture B. Acute PMN infiltration C. Crypt Abscesses D. Basal plasmacytosis
9. A 35-year-old patient with a previous history of duodenal ulcers presents for evaluation because of recurrent pain unresponsive to over-the-counter prilosec therapy. The patient emphatically denies NSAID use. Endoscopy reveals another duodenal ulcer. Histologic evaluation of biopsies obtained from the gastric antrum does not reveal H. pylori infection and gastric pH measured at the time of endoscopy is 2.5. The next most appropriate test is:
a) urea breath test b) serum gastrin d) H. pylori serology d) gastric acid analysis e) serum salicylate concentrations
10. Eradication of Helicobacter pylori infection is least likely to benefit patients who present with which of the following diseases?
a) NSAID-induced ulcers b) Gastric cancer c) Gastric maltoma d) Gastroesophageal reflux disease
11. A previously healthy 45 year old male experiences sudden hematemesis without abdominal pain. Emergency endoscopy is performed after resuscitation and admission to the ICU. Apparent arterial blood is seen pumping from the surface of the proximal stomach without any obvious surrounding ulceration. Endoscopic thermal therapy and injection therapy are performed and the bleeding resolves. What would be the next most appropriate management step?
a) estrogen/progesterone therapy b) placement of an endoscopic tattooing adjacent to the bleeding site c) Helicobacter pylori testing d) endoscopic mucosal resection
12. A 60 year old physician colleague is scheduled for colonoscopy after a flexible sigmoidoscopy demonstrated a 1 cm sigmoid polyp. She has a history of paroxysmal atrial fibrillation for which she takes warfarin. There is no known valvular heart disease. Her INR ranges from 2.5-3.5 over the last year. How should the warfarin be managed to prepare for the colonoscopy?
a. Stop warfarin for 3-5 days before procedure, restart after procedure is completed b. Stop warfarin for 3-5 days before procedure. Use low molecular weight heparin until day before procedure, restart warfarin day after procedure c. Stop warfarin for 3-5 days, admit her to the hospital for intravenous heparin. Stop intravenous heparin 2 hours before procedure, restart heparin and warfarin after procedure, and stop heparin after INR returns to therapeutic level d. Perform procedure without any change in warfarin therapy e. Stop warfarin for 3-5 days, use aspirin daily until procedure, restart warfarin after procedure
13. Which of the following is the most significant risk factor for post-ERCP pancreatitis? a. Participation in the procedure by a trainee b. Placement of a pancreatic stent c. Dilation of a pancreatic duct stricture d. History of previous ERCP-induced pancreatitis e. Removal of a pancreatic duct stone
14. You are asked to evaluate a 72 year-old man who complains of difficulty with swallowing both liquids and solids for 8 months. He claims that he often experiences choking and nasal regurgitation when he swallows. Among the following disorders, the most likely diagnosis is: A. Achalasia B. Scleroderma C. Cerebrovascular accident D. Adenocarcinoma of the esophagus
15. Pill esophagitis often involves the esophagus at the level of the aortic arch. This is because the aortic arch narrows the lumen of the esophagus and because: A. This is the area where the amplitude of peristaltic waves normally is the lowest. B. This is the area where the density of inhibitory neurons normally is the highest. C. This is the area where the number of submucosal glands normally is the highest. D. This is the area where infiltration by eosinophils normally is the highest.
16. A 48 year-old woman complains of hoarseness for the past 6 months. Three weeks ago, she was evaluated by an otolaryngologist who diagnosed laryngopharyngeal reflux and prescribed omeprazole 20 mg QD. She has taken the medication every day since, but she is no better. A physical examination and routine blood tests are normal. Which of the following is the best management strategy at this time: A. Continue omeprazole 20 mg QD, perform 24-hour esophageal pH monitoring B. Discontinue omeprazole, perform 24-hour esophageal pH monitoring C. Increase the dose of omeprazole to 20 mg BID, re-evaluate in 3 months C. Add ranitidine 300 mg HS
17. A 61 year-old man has an endoscopic examination for the evaluation of chronic heartburn. He is found to have columnar epithelium starting at 30 cm from the incisor teeth and extending to the gastroesophageal junction at 38 cm from the incisor teeth. A nodular area is noted at 37 cm. Biopsies are taken only from the nodular area and show specialized intestinal metaplasia with a single focus of high-grade dysplasia in one of the biopsy specimens. Which of the following is the best management option:
A. Repeat the endoscopy and take 4-quadrant biopsies at one-cm intervals from 30 to 38 cm. B. Perform photodynamic therapy C. Perform endoscopic mucosal resection of the nodular area D. Refer for esophagectomy
18. You are caring for a 41 year old woman with short gut syndrome on home intravenous artificial feeding. After doing well for the past two years, she rapidly develops nausea, vomiting, bilateral sixth nerve palsies, nystagmus, ataxia, and slow mentation. You remember learning about this complication at the Bill Steinberg Board Review Course. Your immediate next action is to: a. Eliminate copper from the trace element formulation because of acute copper toxicity causing an iatrogenic Wilson’s disease. b. Query the Home IV company about whether they have been adding vitamins to the solutions. Immediately request high doses of thiamin to correct thiamin deficiency, which has caused multiple neurologic complications. c. Eliminate vitamin A from the solution because this represents acute vitamin A toxicity. Query the Home IV company about whether they have been adding vitamins to the solutions. Immediately request high doses of niacin to correct niacin deficiency causing pellagra.
19. A 35-year old lady with a remote history of DVT in her lower extremities on hormone replacement therapy presents with abdominal and pelvic pain. Her abdomen is soft. Bowel sounds are present. A CT of the abdomen revealed extensive thrombosis of the superior mesenteric venous system. The next best step would be to: A. Intervene surgically to resect thrombosed necrotic bowel B. Diagnostic mesenteric angiography C. IV Heparin D. Small bowel enteroclysis E. Thrombolytic therapy
20. A 70-year old male with a history of cardiovascular disease presented with sub-acute onset of diffuse abdominal pain and rectal bleeding. Physical examination reveals abdominal tenderness but no involuntary guarding. Bowel sounds are present. White blood cell count is 15,000. A plain film of the abdomen revealed mild ileus, and thickened folds in the right colon. Colonoscopy was performed and he was found to have edematous hemorrhagic folds in the right colon. The most likely diagnosis and management is which one of the following: A. Ischemic colitis and observe his clinical course B. Superior mesenteric artery thrombosis and proceed with urgent angiography C. Consider superior mesenteric venous thrombosis and obtain a dynamic CT scan D. Consider superior mesenteric artery embolization E. Start IV Heparin and supportive care
21. Defecation is associated with which of the following?
a) Contraction of external anal sphincter b) Contraction of puborectalis muscle c) Widening of anorectal angle d) Ascent of the pelvic floor
22. . A 10 year old year girl is evaluated in the emergency room with complains of severe colicky abdominal pain of 3 hours duration. The parents report that the patient has complained on intermittent abdominal discomfort associated with nausea and vomiting for the past 6 months. HEENT exam reveals pigmentation of the lips and bucal mucosa. Abdominal exam reveals distention and high pitched bowel sounds with intermittent rushes. On palpation the abdomen is diffusely tender with rebound. Abdominal x-ray reveals dilated loops of small bowel. Which of the following is the correct statement concerning this patient?
A. Has an autosomal recessive syndrome caused by mutation of the STK 11 gene B. Patient’s disorder is characterized by melanotic pigmentation that increases with age C. Patient is at high risk for breast and colon cancer D. Patient is suffering from intestinal dysmotility.
23. In UC when colectomy is performed because of confirmed LGD, colon cancer is reported to be found in approximately: A. 2% B. 20% C. 40% D. 60% E. 75%
24. In inflammatory bowel disease (IBD), which extra-intestinal condition generally does not parallel IBD disease activity?
A. Erythema nodosum B. Sclerosing cholangitis C. Episcleritis D. Peripheral arthritis E. Pyoderma gangrenosum
25. With respect to pregnancy and UC which one of the following are true?
A. Increased risk of flare up. B. Relapses tend to be more severe. C. Sulfasalazine causes kernicterus and should be stopped. D. Sulfasalazine is teratogenic. E. Sulfasalaziine appears in breast milk and should be stopped.
26. The sensitivity of a new blood test for Barrett’s esophagus is 90% and the specificity is 80%. The prevalence of Barrett’s esophagus among patients with gastroesophageal reflux disease is 10%. What is the positive predictive value of a positive test in a patient with gastroesophageal reflux disease? a. 90% b. 10% c. 33% d. 50%
27. Select the most accurate statement regarding the localization characteristics of a gastrinoma. a) Greater than 80% of gastrinomas occur within the pancreas. b) The most common extrapancreatic location of a gastrinoma is the stomach. c) Gastrinomas occur within the duodenum in as many as 50% of cases. d) Bone is the most common site for metastatic gastrinomas to develop.
28. Risk factors for development of drug induced liver injury include all of the following EXCEPT: a. Age greater than 70 years b. Obesity c. Female sex d. Presence of cirrhosis
29. All of the following are true of PSC EXCEPT: a. Liver biopsy is not diagnostic in most cases b. Most patients have co-existent UC c. Cholangiocarcinoma is a common complication d. Stenting of bile duct strictures improves survival.
30. A patient with new-onset ascites but who was not previously known to have liver disease is admitted for evaluation. You order a transjugular liver biopsy and measurement of portal pressures. The following pressures are obtained: wedged hepatic vein = 32 mmHg; free hepatic vein = 12 mmHg. The most likely cause of this patients ascites is: a. Right heart failure b. Extrahepatic portal vein thrombosis c. Alcoholic cirrhosis d. Nephrogenic ascites e. Budd-Chiari syndrome
31. The following are characteristics of ascites from a patient with alcoholic cirrhosis: (SAAG= serum ascites albumin gradient) a. Total protein 3.5 g/dl, SAAG 0.8 g/dl b. Total protein 0.8 g/dl, SAAG 1.4 g/dl c. Total protein 3.5 g/dl, SAAG 1.4 g/dl d. Total protein 0.8 g/dl, SAAG 0.8 g/dl
32. Which of the following underlying liver diseases has the lowest 10-year graft survival after liver transplantation? a. Alcohol b. Hepatitis C c. Hepatitis B d. PBC
33. A 45 year old man is admitted with nausea and jaundice. There is no history of fever. He reports consuming a fifth of vodka per day for the past 15 years. Physical examination reveals tender hepatomegaly; splenomegaly is also present. Laboratory tests reveal a serum biliruin of 3 mg/dl, albumin 3 gm/dl. AST 250 IU/L, ALT 110 IU/L, Alk phos 155 IU/L, PT 14 secs and serum creatinine 2.1 mg/dl. The most appropriate for this patient is: A. prednisone 30 mg/day B. prednisolone 30 mg/day C. hydration, vitamin K, monitor for alcohol withdrawal D. propylthiouracil E. referral to a liver transplant center
34. For immunosuppressed, high-risk individuals, who have received and responded to the three-dose regimen of HBV vaccine, booster doses are:
a) currently recommended at yearly intervals if anti-HBs levels fall below 10 mIU/mL b) currently recommended at 5 year intervals after primary immunization c) currently recommended at 15 year intervals after primary immunization d) not currently recommended after primary immunization
35. For patients receiving a liver transplant for acute liver failure, the one-year survival rate is approximately: a) 25% b) 50% c) 75% d) 100%
36. Which of the following patients with chronic hepatitis C is most likely to respond to pegylated interferon plus ribavirin treatment:
a. A 44 year-old man with continuing chronic alcoholism, and HCV genotype 1 b. A 44 year-old man with decompensated cirrhosis, and HCV genotype 1 c. A 44 year-old woman who dates her infection to injecting drug use, begun at age 40, HCV genotype 2, and who has a HCV RNA level of 80,000 IU/mL d. A 44 year-old woman with a history of injecting drug use 30 years ago, HCV genotype 1, and who has a HCV RNA level of 6 million IU/mL
37. The most common liver disease during pregnancy is:
a. Cholestasis of pregnancy
b. Acute fatty liver of pregnancy
c. HELLP syndrome
d. Viral hepatitis
e. Cholelithiasis
38. Small duct pancreatitis:
A) Invariably progress to steatorrhea B) Is usually caused by alcohol-abuse C) Is frequently associated with pancreatic calcification D) Is a frequent cause of unexplained chronic abdominal pain
39. The most appropriate medication to employ in treating pancreatitis secondary to hypertriglyceridemia is: A) Simvastatin B) Atrovastatin C) Gemfibrozil D) Niacin preparations
40. Which of the following neural system inhibit pancreatic secretion? a. vagal nerves b. sympathetic nerves c. postganglionic parasympathetic nerves d. all nerves passing through the celiac plexus to the pancreas