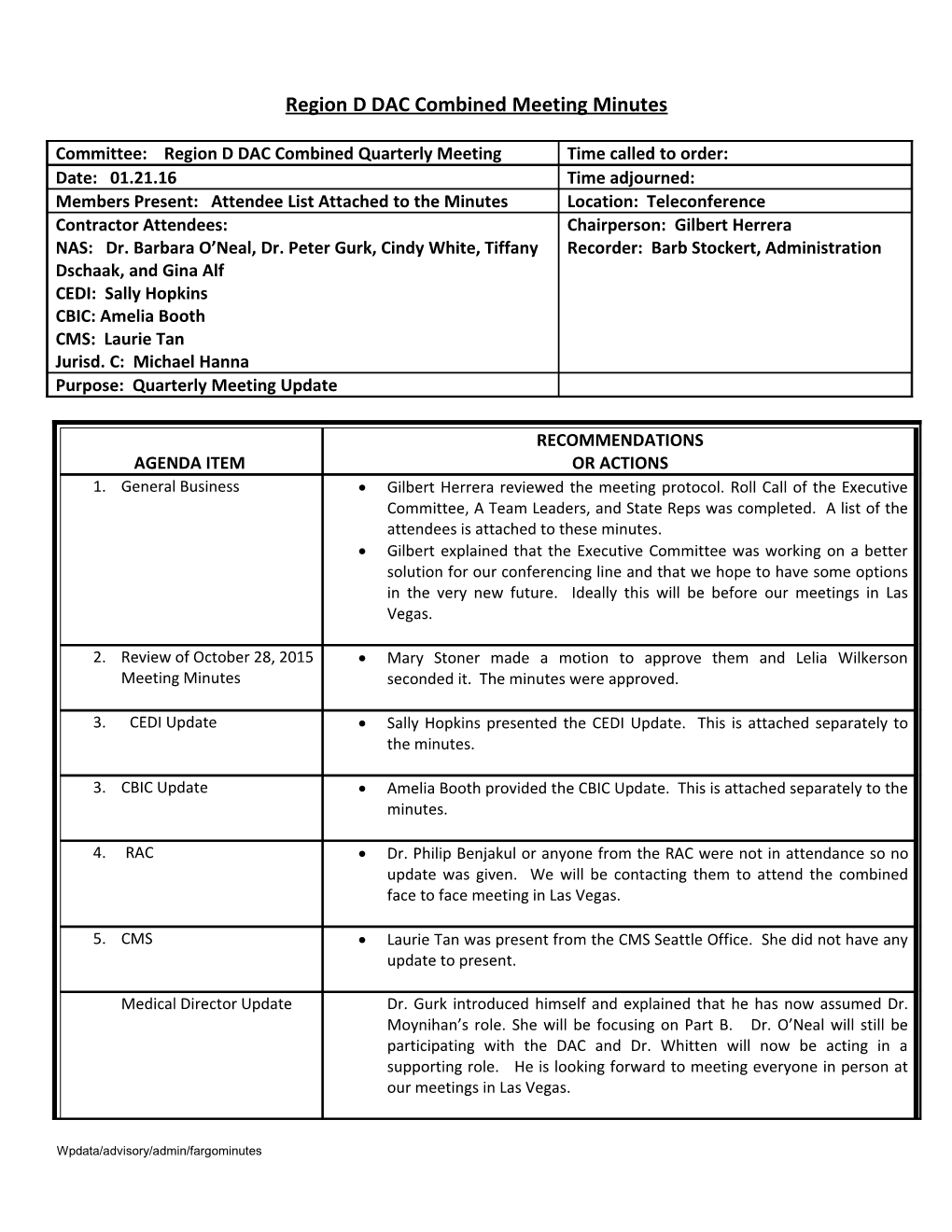
Region D DAC Combined Meeting Minutes
Committee: Region D DAC Combined Quarterly Meeting Time called to order: Date: 01.21.16 Time adjourned: Members Present: Attendee List Attached to the Minutes Location: Teleconference Contractor Attendees: Chairperson: Gilbert Herrera NAS: Dr. Barbara O’Neal, Dr. Peter Gurk, Cindy White, Tiffany Recorder: Barb Stockert, Administration Dschaak, and Gina Alf CEDI: Sally Hopkins CBIC: Amelia Booth CMS: Laurie Tan Jurisd. C: Michael Hanna Purpose: Quarterly Meeting Update
RECOMMENDATIONS AGENDA ITEM OR ACTIONS 1. General Business Gilbert Herrera reviewed the meeting protocol. Roll Call of the Executive Committee, A Team Leaders, and State Reps was completed. A list of the attendees is attached to these minutes. Gilbert explained that the Executive Committee was working on a better solution for our conferencing line and that we hope to have some options in the very new future. Ideally this will be before our meetings in Las Vegas.
2. Review of October 28, 2015 Mary Stoner made a motion to approve them and Lelia Wilkerson Meeting Minutes seconded it. The minutes were approved.
3. CEDI Update Sally Hopkins presented the CEDI Update. This is attached separately to the minutes.
3. CBIC Update Amelia Booth provided the CBIC Update. This is attached separately to the minutes.
4. RAC Dr. Philip Benjakul or anyone from the RAC were not in attendance so no update was given. We will be contacting them to attend the combined face to face meeting in Las Vegas.
5. CMS Laurie Tan was present from the CMS Seattle Office. She did not have any update to present.
Medical Director Update Dr. Gurk introduced himself and explained that he has now assumed Dr. Moynihan’s role. She will be focusing on Part B. Dr. O’Neal will still be participating with the DAC and Dr. Whitten will now be acting in a supporting role. He is looking forward to meeting everyone in person at our meetings in Las Vegas.
Wpdata/advisory/admin/fargominutes Dr. O’Neal did not provide an update and said that Dr. Gurk covered it.
6. Yondelis and Blincyto Deanne Birch asked the following question regarding the recent release of 2 Joint DME MAC publications released regarding coverage and coding for 2 new drugs, Yondelis and Blincyto™. Could the Medical Directors provide some insight as to why it was determined that Blincyto administration via External Infusion pump would be covered and included under the EIP LCD benefit but Yondelis via External infusion pump was determined as NOT eligible for inclusion under the EIP LCD?
01/21/16 Dr. Gurk replied that he will take this question back and provide an update in Las Vegas.
7. Previously Submitted We need assistance from CMS on a claim processing issue. Suppliers sometimes Questions to CMS/Noridian provide capped rental items to Medicare customers that are not medically and CEDI necessary per Medicare coverage criteria. However, that item may be covered by Medicaid or another funding source, as a purchase. The secondary funding Billing for Purchase requires a denial from Medicare. Currently, any claim submitted for a capped rental item with a NU modifier will be rejected on the front end as an invalid code/modifier combination. This does not give an actual claim denial. Will CMS please issue claim processing instruction revisions to allow submission, and subsequent denial, for capped rental items provided and billed as purchases with NU modifiers? Examples of applicable situations can be provided.
10/28/15 Update: Most often these companies require a Medicare denial to process and pay the claim. The way it is currently set up the claim cannot even get into the system. Discussion followed and this will be researched. It is possible something could be done or an edit added.
01/21/16 Update: Cindy replied that there is not a solution for this. Mary Stoner asked if a modifier could be created or another means to identify claims in this situation. Cindy replied she will bring it back but because we are asking for a different pricing category they might not be able to do this.
HyQvia Coverage Policy HyQvia Coverage Policy: This was brought forth in Oct. 2015. The IV PEN team wanted to know when the HyQvia coverage would be added to the External Infusion Pump LCD. It was understood that there were numerous comments on this. Bill Noyes asked that this be added to the LCD. It is only seen in the joint publication. As a reminder: this was/is the concern noted: The issue is conflicting/contradictory language between with the EIP LCD and the HyQvia Joint publication. The EIP LCD states: H. Subcutaneous immune globulin (J1559, J1561, J1562, J1569) is covered only if criteria 1 and 2 are met: 1. The subcutaneous immune globulin preparation is a pooled plasma derivative which is approved for the treatment of primary immune deficiency disease; and, 2. The beneficiary has a diagnosis of primary immune deficiency disease (See Diagnosis Codes Group 3 that Support Medical Necessity section below). Coverage of subcutaneous immune globulin applies only to those products that are specifically labeled as subcutaneous administration products. Intravenous immune globulin products are not covered under this LCD. Only an E0779 infusion pump is covered for the administration of subcutaneous immune globulin. If a different pump is used, it will be denied as not reasonable and necessary. But the HyQvia (which is Subcutaneous IG) Joint Publication specifies the need to use an E0781 pump. HYQVIA is administered using a programmable variable infusion pump (HCPCS code E0781), that is capable of infusing a patient’s therapeutic dose at infusion rates of up to 300 mL/hr/site. Coverage is available for claims with dates of service on or after September 12, 2014 when all of the following requirements have been met:
The criteria for Subcutaneous Immune Globulin as specified in the External Infusion Pump LCD are met, and
HYQVIA is administered subcutaneously through an E0781 pump that is pre-programmed, and
The E0781 pump is delivered to the Medicare beneficiary in a “locked mode” i.e., the patient is unable to self-adjust the infusion rate. The medical record must contain sufficient information to clearly demonstrate that the beneficiary meets all of the requirements specified above.
10/28/15 Update: It is a coding issue and is addressed in the publication. They will take this back and look at it.
01/21/16 Update: Dr. Gurk commented that the Medical Directors Are working on this and the IV Policy is being updated. He said to expect an answer sooner rather than later this. They meet again next Tuesday so hopefully this can be put to rest then.
PECOS Denials 10/28/15 Numerous concerns were noted. Many physicians that are listed as PECOS certified on a date of service are not listed there when the claim is processed. Cindy clarified that it should be the date of service not the date of submission. Sheila Roberson said that Jody gave her some information that the information might not pick up when it is reactivated. Such as ½-12/31. Jody suggested to do a print screen of each and send the examples in. Cindy asked that these now be submitted to her. Mary Stoner asked how does the Supplier know and how can we get claims to pay? She stated it should not be the patient’s responsibility to pay either. Cindy said we have to figure out the problem and then find the solution. DAC members are to submit issues to the DAC Office. They will be sent to Cindy.
Paula Koenig asked about a situation when a Dr. is elgible when the order is written but they retire and give up their number, so the order would not be valid. The answer received was a joint answer from all the MAC’s. The will relook at this 13 months after implementation.
01/21/16 Mary Stoner asked about PECOS Denials on claims which are denying because the Dr. is not enrolled in PECOS. When the Supplier checks the PECOS website it shows the Physician is enrolled, but when the claim is submitted it will deny because they are not enrolled. Mary said the information you are seeing on your side is not what we are seeing on our side. Laurie Tan CMS Representative requested for Mary to send her examples of where this has been an issue. She will look into it and send to Central enrollment staff. Mary will send these to her after the call. a. Date on DIF 10/28/15 Jeff Schwindt, IV PEN Team asked what date/timeline should be on the DIF and if it should be the date of the order? Dr. Whitten said this is still under active discussion but they have not changed their process at this time. Date on DIF: What date/timeline should be on the DIF and if it should be the date of the order?
10/28/15 Update: Dr. Whitten said this is still under active discussion but they have not changed their process at this time.
01/21/16 Update: Cindy responded that there had been a lot of discussion on this but they have determined that the date of the order should be the date on the DIF. Deanne Birch thanked Noridian for their response but questioned if it is okay to use the date a verbal order was received. Cindy explained as long as the item does not require a WOPD the verbal order date would be acceptable and the claim date would not deny. The verbal order date must be the date on the DIF. b. Issue with Orthotic Fitters 10/28/15 Joe McTernan, AOPA and O&P Team asked about requirements in the states for Orthotic Fitters. Since many of these regulations were written prior to states requiring licensing it could be a legal question. Dr. Whitten asked for some examples of specific states where there might be an issue. He expects that CMS will be actively involved in this.
10/28/15 Update: Dr. Whitten asked for some examples of specific states where there might be an issue. He expects that CMS will be actively involved in this.
01/05/16 Update: The examples requested did not get submitted to NAS. The DAC Office just received these today and am attaching with to this email.
01/21/16 Update: Cindy responded that she had just recently received these examples but wanted clarification on what we were asking. Wendy Miller, O&P A Team Leader responded there are a few states that license orthotic fitters and they are allowed to fit prefabricated devices. She requested a better explanation of the rule and the requirements. Cindy will take this back for further discussion. c. Quantities on Written 10/28/15 Paula Koenig presented this and said that it is now a requirement from Orders the article that the number of units need to show on the written order. Sometimes on wheelchair orders these initial units do not match up later. Cindy will check on this and send to Barb.
10/28/15 Update: Cindy will check on this and send to Barb.
01/21/16 Update: Cindy explained a detailed description of the item is needed on the order. If the order or description changes in any way a new order is needed. d. POE Update Cindy White provided the update and it is attached to the minutes. 8. New Questions to Noridian 01/21/16 Can an update be provided to DAC members? Cindy explained that they a. Prior Authorization have to wait for CMS direction before any information can be released. She said the best option is to be sure members are signed up for the List Serv.
Cindy Coy asked Laurie Tan if there has been any education done to referral sources? We need to be able to provide information to them. Laurie asked that Cindy email her this and she will try to respond.
b. Fee Schedule 10/28/15 Paula Koenig asked if there is an update or info on changes to modifier Changes use with the 2016 fee schedule changes; specifically, the use of KE and KY modifiers; and any updates on the exclusion of applying the RSPAs to wheel chair options used w Group 2 power chairs
c. Update on SMRC 10/28/15 Can we get an update on SMRC activity? Kimberlie Rogers-Bowers Activity explained that you do a great job educating and working with the CERT contractor to keep everyone aligned with the same processes in looking at documentation. It is our hopes that this will be the same way. Cindy replied that this is a different contractor and they operate separately from Noridian.
Barb Stockert asked if they would be able to provide a contact name with Strategic Health Care so we could invite them to our meeting in Las Vegas. Noridian will check into this and if able provide the DAC this information.
d. TeleHealth 01/21/16 Mary Stoner presented: Telehealth Medicine is becoming more and Medicine more prevalent. Are there any products or product categories that would not be acceptable for telehealth orders? Example...orthotics...can a telehealth doctor that has never "seen" only "has spoken" to the patient order a brace? CMS has a number of publications regarding this but they are not real clear. Cindy said she will take this back to the POE Committee and see if training can be done in this area.
e. Transition to JA 01/21/16 Is this going to be handled in the same location/office that our JD Contract contract is? Is it the intention of CMS/Noridian to eventually make this a Combined Council? Cindy responded that there will be contact information released soon on this. Currently the one area they are considering is to have a shared List Serv. She emphasized that JD Suppliers would see no impact with this transition. She will provide more information as it becomes available.
9. Next Meeting The next Combined Meeting is set for Tuesday, March 1st from 10-12:00 pm at the Mandalay Bay Convention Center in Las Vegas. The room number will be forth coming.