Protocol No 7 – Hygiene, sanitation and isolation aspects of CTCs
Risks of not implementing hygiene, sanitation & isolation aspects
It is VERY important that basic hygiene, sanitation and isolation procedures are followed at ALL TIMES in health facilities where patients with AWD are being treated. Failure to follow these procedures could lead to cross-infection of other patients or infect people who come to the health centre who did not in fact have AWD.
Helping staff to improve their health facilities
Helping the staff to improve their facilities: Observing another well set up CTC centres / improved hygiene centre. Discussing what they saw and suggesting any improvements. Providing required equipment where not already available. Providing additional operational costs for guards, cleaners and medical helpers. Working with the staff to discuss and suggest and make the improvements together. Follow up visits after a few days to see how the procedures are being followed.
Minimum hygiene, sanitation and isolation activities
Essential principles that all health facilities and CTCs must follow: 1. Isolate severe cases 2. Contain all excreta (faeces and vomit) 3. Only one carer per patient 4. Wash hands with chlorinated water 5. Disinfect feet when leaving the centre 6. Disinfect clothes of infected people before leaving the centre 7. Provide hygienic and with privacy 8. Toilets and bathing areas for patients and carers 9. Follow up on the families and relatives of the patient, ensure there are no other cases and disinfect the house, give hygiene information. 10. If people arrive by public transport the cars should be disinfected.
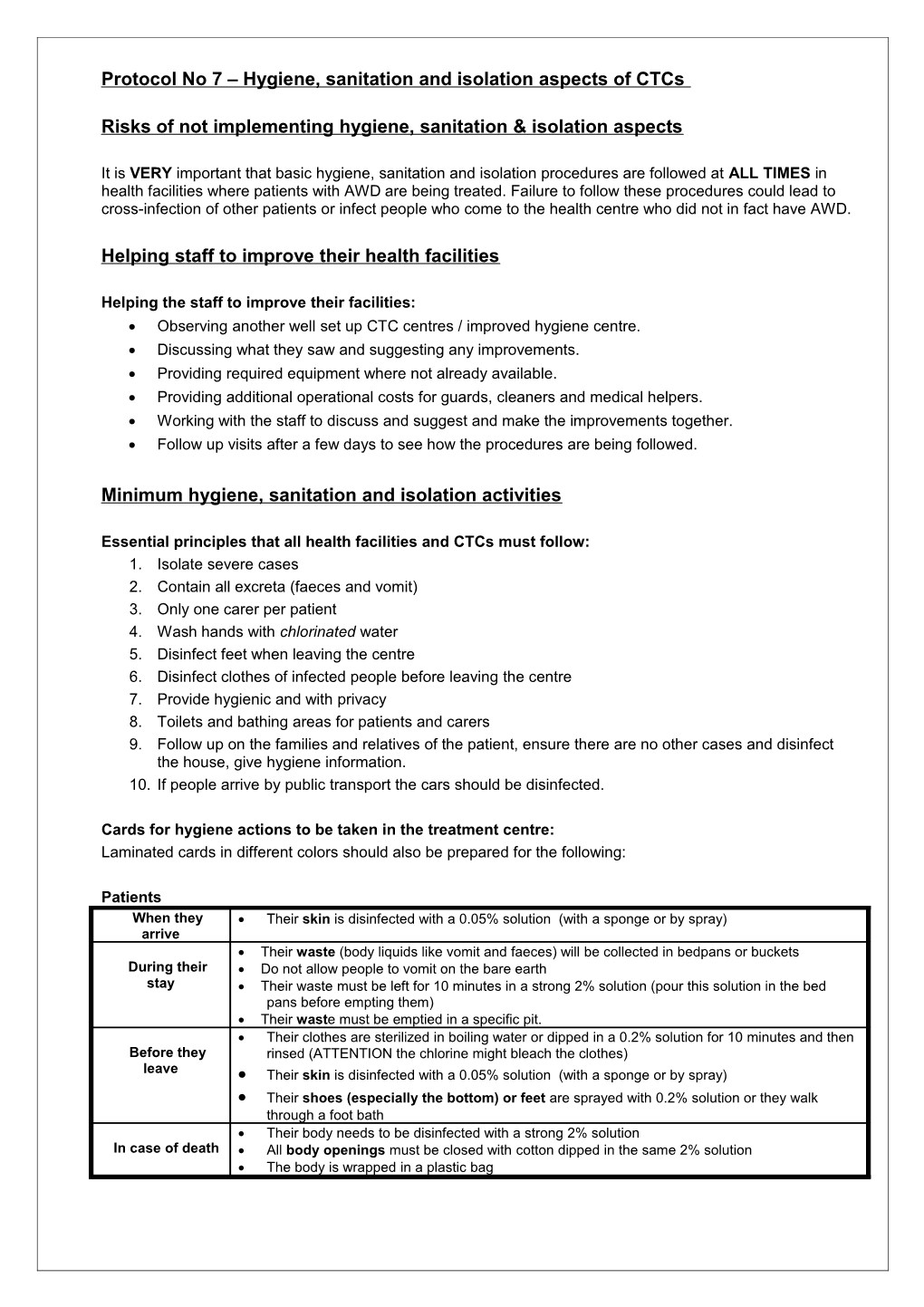
Cards for hygiene actions to be taken in the treatment centre: Laminated cards in different colors should also be prepared for the following:
Patients When they Their skin is disinfected with a 0.05% solution (with a sponge or by spray) arrive Their waste (body liquids like vomit and faeces) will be collected in bedpans or buckets During their Do not allow people to vomit on the bare earth stay Their waste must be left for 10 minutes in a strong 2% solution (pour this solution in the bed pans before empting them) Their waste must be emptied in a specific pit. Their clothes are sterilized in boiling water or dipped in a 0.2% solution for 10 minutes and then Before they rinsed (ATTENTION the chlorine might bleach the clothes) leave Their skin is disinfected with a 0.05% solution (with a sponge or by spray) Their shoes (especially the bottom) or feet are sprayed with 0.2% solution or they walk through a foot bath Their body needs to be disinfected with a strong 2% solution In case of death All body openings must be closed with cotton dipped in the same 2% solution The body is wrapped in a plastic bag Relatives When they Only 1 relative allowed (unless the others are also sick) arrive During their When possible, try to provide separate latrines and washing facilities for the relatives stay Every time they use the toilet they should wash their hands with a 0.05% disinfected water The relatives should try to minimize contacts with the patient’s waste Before they Every time they leave the camp they have to wash their hands in a 0.05% solution leave The sole of their shoes (especially the bottom) must be sprayed with a 0.2% solution or walk through a footbath If food has come from outside, the plates and everything should be washed in a 0.05% solution before being allowed from the camp If dirty, their clothes are sterilized in boiling water or dipped in a 0.2% solution for 10 minutes and then rinsed with clean water In case of death The relatives should be advised that funeral ceremonies are a risky practice All the people handling the dead body should wash their hands and not handle food Hygiene education should be given to the relatives before returning to the center
Staff When they arrive Staff should use gloves when treating patients During their stay Staff should try to use separate latrines and washing facilities, ideally in neutral area Staff should use gloves when treating patients Staff should wear gowns and special outfits which will be disinfected in the center After treating the patient the staff member should wash their hands with disinfected 0.05% solution (and their gloves if they are reusable )
What to do with dead bodies / instructions for funerals: Keep the body separate from the patients. Disinfection of corpses and plugging of orifices with cotton in a 2% chlorine solution (note – only effective for a short period). Bury as soon as possible. Wrap the body in a plastic sheet when transporting to catch any body fluids. Discourage funeral feasts until the end of the outbreak (or limit size). Undertake hygiene promotion at funerals.
Minimum key staff and job descriptions
Minimum key staff: As a minimum the CTCs or health centres which are dealing with AWD infected people, must have the following staff: 1. Medical and support staff (cleaners, guards etc) should work ONLY with the AWD infected patients – they must not switch between different groups as this will lead to infection. 2. There should be one nurse per shift, as the center has to be open 24 hours a day. 3. There should be 1 medical helper per shift that assists the nurse and prepares ORS if possible. 4. 1 Cleaner / sprayer per shift– who deal with all of the cleaning and disinfecting of people’s clothes, disposal of waste etc. 5. 1 guard per shift – to make sure that people follow the hand and foot washing procedures and ensuring that the isolation rules are followed. They need to be very strict about these rules! 6. Cook – to cook for the patients, carer, health and other staff who remain in the centres (where possible). Job descriptions for staff: The following simplified job descriptions have been developed from the MSF cholera guidelines. They have been simplified so that they can be realistically followed in all health posts and small CTCs run by any organisation. The cards should be prepared in different colors and laminated and in both the local language and English. They will be hung up in the centers for use by the staff on a daily basis.
Nurses / Medical helper Actions Remarks Case Management Follow training instructions Differentiate non AWD from AWD and severe cases The ‘differentiation area’ should be separated from the centre. Only from mild patients with AWD can enter the contagious area Preparing ORS every day Follow training instructions (This could be done by a medical helper if available) Supervise cleaners and ensure hygiene and Be familiar with their tasks and do some inspections sanitation rules are followed Use personal hygiene Use separate toilets. Wear gloves and boots in the center area. Wash hands after treating patients even when wearing gloves. Hygiene education when patients and relatives Focus on hand washing, safe water and funeral practice leave or die Hygiene education for community members When giving community education from the centre site, hold the training outside the centre itself. Put syringes / needles into syringe box Syringe box should be used until full and given to RHB for disposal
Cleaners Actions Remarks Cleaning bed pans every hour (soaking them in Pour a 2% solution for 10 minutes, then empty in a covered pit chlorine and emptying them into the pit) latrines Clean toilets and showers 2 to 4 times per day Use 0.2% solution Cleaning beds and floors 2 times a day or when they Clean or spray using 0.2% solution become dirty
Disinfecting patients when they arrive Spray them or use sponge with 0.05% solution (or this can be done by the guard) Prepare every day 2 types of disinfecting solutions Follow solution table (0.2% and 0.05% solutions) (This could be done by the Medical helper if available) Prepare every week the 2% solution Follow solution table Disinfecting patients when they leave Spray them or use sponge with 0.05% solution Cleaning clothes when people leave (patients, Boil them or soak them in 0.2% solution for 10 minutes then rinse relatives and staffs) with clean water
Refill hand washing containers when empty Use 0.05% solution Refill drinking water containers Use PUR or WaterMaker prepared by the nurses Refill sprayers and foot bath Use 0.2% solution Collect waste in bins with lids Burn in an open pit Dispose buckets with excreta Put half a cup 2% chlorine solution in the empty buckets Use personal hygiene Use separate toilets. Wear gloves, apron or overall and boots in the center area. Wash hands and gloves after work. Guard Actions Remarks Admitting only patients and 1 relative If relatives are sick then they can be admitted Making whoever exits the camp (patient, relatives, Make sure there is chlorinated water in the container staff) wash their hands every time Making whoever enters or exits the camp (patient, Spray the bottom of the shoes relatives, staff) disinfect feet or shoes Make sure there is chlorine solution (0,2%) in the sprayer or foot wash Use personal hygiene Use separate toilets. Wear gloves and boots in the center area. Wash hands and gloves after work.
Making chlorine mixes
Disinfecting solutions: Depending on the chlorine available, choose the table appropriate and provide this table only for making up the disinfectants: 5% liquid - local Birkina yellow bottle 10% liquid - provided by UNICEF 65-70% HTH powder – imported
2% solution 0.2% solution 0.05% solution Waste and Floor Hands Drinking water Excreta Objects / Beds Skin Dead Bodies Footbaths Clothes Yellow bottle 10 lt. chlorine 1 lt. chlorine 0.2 lt. chlorine 10 lt. water 19 lt. water 19.8 lt. water 5% solution (1:1) (1:25) (1:100) Blue container 5 lt. Chlorine 0.5 lt. chlorine 0.1 lt. chlorine 15 lt. water 19.5 lt. water 20 lt. water 10% solution (1:4) (1:50) (1:200) Waterguard 1 cap (only transparent water) Watermaker 1 sachet PUR 2 sachets NB: The solutions should be freshly prepared every day, since light and heat weaken the solution If there is no chlorine available, use normal bleach that is locally on the market available (5%).
2% solution 0.2% solution 0.05% solution Waste and Floor Hands Excreta Objects / Beds Skin Dead Bodies Footbaths Clothes HTH powder 65- 30g for 1 liter 3g for 1 liter 0.75g for 1 liter 70% 300g for 10 liter 30g for 10 liter 7.5g for 10 liter Never mix the solution with detergent! Disinfecting transport and the houses of the infected people
When people are transported to a health facility they may leave traces of AWD in the vehicle which may infect others. This needs to be disinfected to prevent cross-contamination. Disinfecting people’s houses can also lead to opportunities for undertaking hygiene promotion or surveillance activities where new cases are identified.
1. Disinfect immediately the car in which the patient was transported in (Ambulance or Taxi) on arrival before it leaves again. Use a 0.05 % Chlorine solution for the car.
2. It is important to go immediately to the house of the patient instead of waiting until the patient is discharged and going home.
3. Explain to the household that spraying of chlorine is done to disinfect and that is not poison.
4. Use a 0.2 Chlorine Solution to do house spraying.
5. Ask in which places the patient was vomiting and where has been stool.
6. Spray also latrine (if there is), clothes and kitchen area (after removing food items).
7. The visit of the affected household is a good opportunity to give extra Hygiene Promotion to the family members and the neighbors.
8. At the same time it is a way of surveillance, as you can detect new cases in the neighborhood.
Layouts of CTC / isolation areas in health facilities a) A simplified arrangement which can be used at a small health centre
The above layout is for a reasonably large CTC / treatment centre, but the principle of patient flow and isolation is the same for smaller centres. The patients under observations should not be mixed with the patients who are severely affected and except for the patient, staff and one carer, no other people should be allowed to be in the centre. Simple design guidelines for latrines for the CTCs
Siting: 1. The latrine should be between 5 to 10m from the tents where people are staying. This will hopefully be far enough away to prevent the smell becoming a problem and near enough that people can reach them for use. 2. Care must be taken that these latrines are a minimum 30m from any groundwater source. The safe distance is shorter than this but this allows for a margin of error. 3. The latrine should not be located in any channels where water flows during heavy rains. If it is in this location, then there is a risk of it flooding or collapsing from water entering down the sides of the pit. 4. Ideally therefore should be separate latrines for women and men which are located a small distance away from each other or separated by a screen. In the smaller centres a joint latrine for men and women can be considered after checking the local customs. 5. The patients and the staff should have different latrines. The carers will probably need to use the same latrines as the patients depending on the size of the centre. Particular effort will need to be focused on keeping the latrines clean for all users. 6. The entrance to the latrine should be facing away from the centre so that people are not seen entering or leaving the latrine for the privacy of the user.
Design: 1. All floor areas in the latrines should be cleanable and the cleaning water must be washed into the pit. 2. The walls of the latrine should ideally be close up to the sides of the latrine slab so that vomit or feaces are more likely to hit the plastic slab. Alternatively the space inside the latrine can be bigger, but all floor areas must be covered with plastic sheeting. 3. As some people using the latrine may need a carer the latrines could be made of double size (ie one plastic slab and an equivalent size area with plastic sheet for the carer to stand on) to allow the carer to also enter at the same time. This can be discussed by the team on site with the users and CTC staff. 4. The slab should be slightly above the ground level (i.e. should sit on the ground level or be slightly raised) so that rain water from the ground will not run into the latrine through the central hole. 5. A raised mound of soil (can be taken from the excavation) should be placed around the three sides of the latrine structure to prevent any run off from the ground to enter the pit or weaken the top of the pit and cause it to collapse. 6. The pit should be as deep as possible depending on the soil strength / stability. As most centres will be small the pits should not fill up too quickly. 7. The pit should be dug leaving 0.15-0.2m around all edges for the slab to rest on. As a minimum two strong pieces of wood or logs should be dug into the ground which will extend longer than the pit length or width, on which the slab will sit (or a frame constructed for the slab to sit on which has extending arms to provide more stability / support). 8. Thick plastic sheeting should be used to surround the latrine and nailed to the upright poles. A loose flap door should also be provided. A roof can also be added but will require additional bracings for the walls of the latrine. If there is enough wood then bracing pieces can be added to stabilise the walls.
Maintenance: 1. The latrine should be cleaned regularly with 0.2% disinfectant. 2. Latrines which fill up to 0.5m to the surface should be closed and filled in. If the pit becomes too full then it will be difficult to fill it in without spilling the contents on the surface. Another pit can be dug for continuation of use. Picture of a latrine to be inserted – side view and slab – provided by MSF
Simple guidance for bathing units for the CTCs
Siting 1. The bathing units for men and women should ideally be located some distance apart from each other to allow for privacy. 2. They can also be located relatively near to the latrine but care must be made to ensure that the waste water flows away from the latrine pit, so as not to damage the pit.
Design 1. The bathing unit is simply a screened unit which allows people privacy for washing / bathing. The door should be away from the CTC and should be formed using a flap of plastic. 2. It should allow enough space for both a patient and carer and for the person to move around while bathing. 3. The floor should be washable and on a slight slope falling in a direction towards a pit filled with stones to take the waste water (remember that the waste water will be contaminated and hence is dangerous). The slope can be formed either by digging slightly into the ground or using wood to raise up the base of the unit. 4. If wooden planks are used to form the floor of the bathing unit, then they should be covered with thick plastic sheeting nailed down to the wooden planks.
Maintenance: 1. The floor of the bathing unit should be washed regularly with 0.2% chlorine solution. List of minimum requirements for equipment for hygiene, sanitation & isolation of the CTCs (small centre at health centre)
Quantity Unit cost Cost for Cost for No. Item description required for 1 (USD) 1CTC 40 CTCs CTC Tents for patients 72 sq meter (10 patients, 10 1 1400 1400 56,000 carers, space between beds) Tents 24 sq meter 2 700 1400 56,000 CTC beds 10 50 500 20,000 Plastic mattresses – for staffs 10 18.2 182 7,280 Fencing rope (bright colours if possible) of 200m 200m 46 46 1,840 Plastic sheets 4 x 6 m (or equivalent) 20 pc 10 200 8,000 Blankets 15 8 120 4,800 Pillows 15 3 45 1,800 Bed pans 12 0.5 6 240 Safety box (syringes) 20 0.8 16 640 Hand torch (flash light) 5 1.2 6 240 Dry cell batteries (for hand torch) 20 0.3 6 240 Stretchers 2 110 220 8,800 Matches 1 pack of boxes 1 1 40 Candles 100 0.1 10 400 Large Dust bins with lids 5 15 75 3,000 Plastic buckets (with lids) – 10 L 10 1.5 7.5 300 Plastic buckets (with lids) – 30 L 5 1.75 7 280 Metal drum incinerator (or can use pit for burning) 1 25 25 1,000 Cleaning plastic brooms 4 1.50 6 240 Plastic apron (not disposable) 10 1 10 400 Medical gown/ Fabric 10 10 100 4,000 Sprayers – large (back pack type) 2 25 50 2,000 Trays for footbaths (large and wide) 2 1 2 80 Roto tanks, 2,000 litres 1 175 175 7,000 Blue water container (30-40litres) with tap for hand- 5 5 15 600 washing Powdered soap – for washing dishes, cartons of 20 0.2 4 160 100g Disinfectant – for cleaning, sterilizing etc (5% 60 bottles 30 60 2,400 chlorine solution, 1 litre bottles) Disinfectant with HTH 70% (1 kg/day) 30 kg Tissue paper, rolls – 100 pieces pack 3 34.5 103.5 4,140 Heavy duty rubber gloves (not disposable) 10 pr 1.8 18 720 Plastic table 3 42 126 5,040 Plastic chair 4 13 52 2,080 Plastic cup 50 0.3 15 600 Tea spoon 50 0.3 15 600 Plastic plates 50 0.3 15 600 Squatting slabs 4 Not available - - in local market Laundry soap 100 0.4 40 1,600 Body soap 100 0.25 25 1,000 Jerry cans of 20 liters 10 2.9 29 1,160 Gum boots – mixed sizes 10 pairs Kerosene lantern for light 8 Blue overalls (coveralls) 6 pair Cleaning items – 1 set to include – toilet brushes x 1 set 4, cloths x 20, mop & bucket x 3 Large plastic containers / baths for soaking clothes 3 Funds for buying wood poles for fences and $100 structures and minor local costs Total cost (USD)