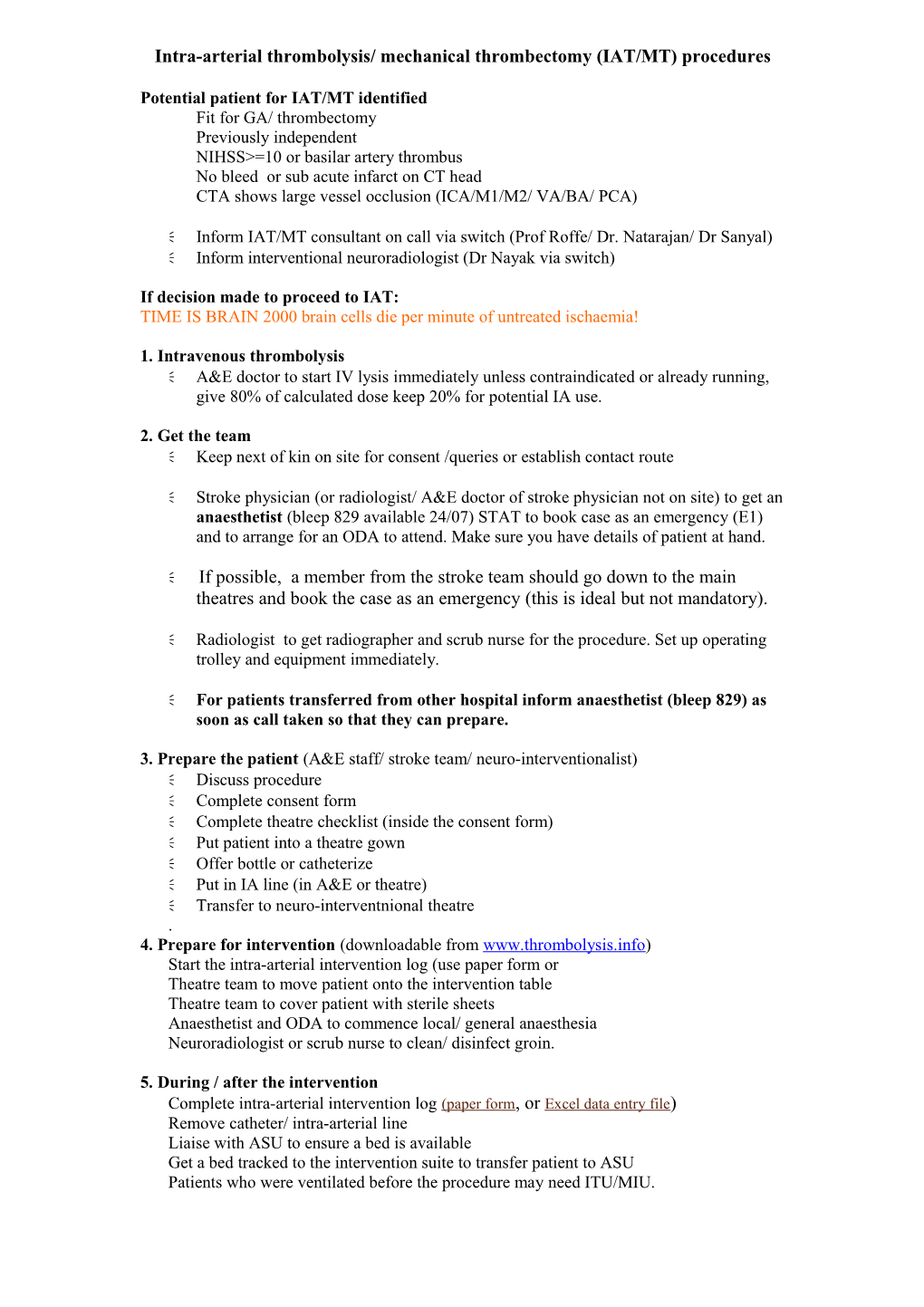
Intra-arterial thrombolysis/ mechanical thrombectomy (IAT/MT) procedures
Potential patient for IAT/MT identified Fit for GA/ thrombectomy Previously independent NIHSS>=10 or basilar artery thrombus No bleed or sub acute infarct on CT head CTA shows large vessel occlusion (ICA/M1/M2/ VA/BA/ PCA)
Inform IAT/MT consultant on call via switch (Prof Roffe/ Dr. Natarajan/ Dr Sanyal) Inform interventional neuroradiologist (Dr Nayak via switch)
If decision made to proceed to IAT: TIME IS BRAIN 2000 brain cells die per minute of untreated ischaemia!
1. Intravenous thrombolysis A&E doctor to start IV lysis immediately unless contraindicated or already running, give 80% of calculated dose keep 20% for potential IA use.
2. Get the team Keep next of kin on site for consent /queries or establish contact route
Stroke physician (or radiologist/ A&E doctor of stroke physician not on site) to get an anaesthetist (bleep 829 available 24/07) STAT to book case as an emergency (E1) and to arrange for an ODA to attend. Make sure you have details of patient at hand.
If possible, a member from the stroke team should go down to the main theatres and book the case as an emergency (this is ideal but not mandatory).
Radiologist to get radiographer and scrub nurse for the procedure. Set up operating trolley and equipment immediately.
For patients transferred from other hospital inform anaesthetist (bleep 829) as soon as call taken so that they can prepare.
3. Prepare the patient (A&E staff/ stroke team/ neuro-interventionalist) Discuss procedure Complete consent form Complete theatre checklist (inside the consent form) Put patient into a theatre gown Offer bottle or catheterize Put in IA line (in A&E or theatre) Transfer to neuro-interventnional theatre . 4. Prepare for intervention (downloadable from www.thrombolysis.info) Start the intra-arterial intervention log (use paper form or Theatre team to move patient onto the intervention table Theatre team to cover patient with sterile sheets Anaesthetist and ODA to commence local/ general anaesthesia Neuroradiologist or scrub nurse to clean/ disinfect groin.
5. During / after the intervention Complete intra-arterial intervention log (paper form, or Excel data entry file) Remove catheter/ intra-arterial line Liaise with ASU to ensure a bed is available Get a bed tracked to the intervention suite to transfer patient to ASU Patients who were ventilated before the procedure may need ITU/MIU.