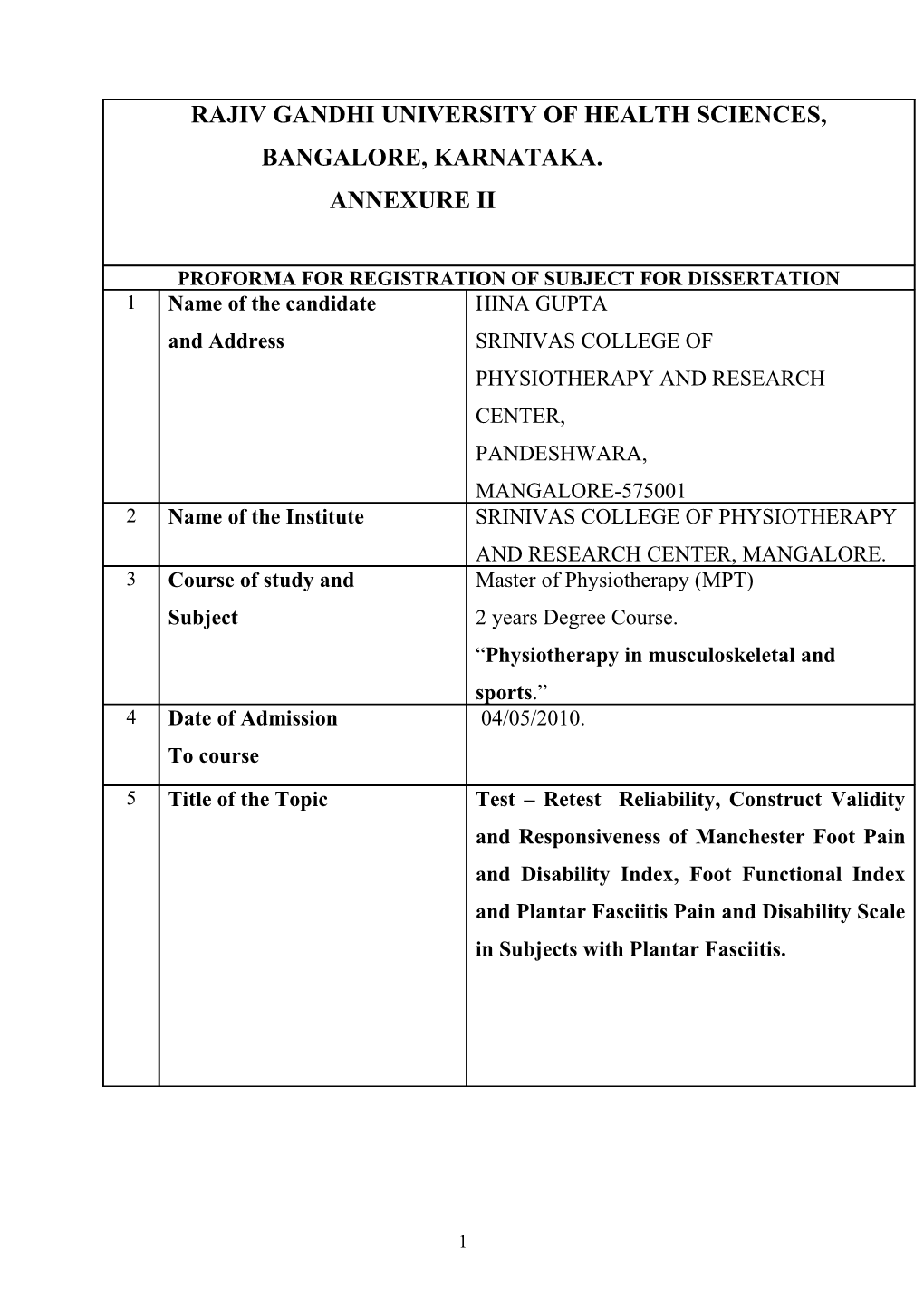
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA. ANNEXURE II
PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION 1 Name of the candidate HINA GUPTA and Address SRINIVAS COLLEGE OF PHYSIOTHERAPY AND RESEARCH CENTER, PANDESHWARA, MANGALORE-575001 2 Name of the Institute SRINIVAS COLLEGE OF PHYSIOTHERAPY AND RESEARCH CENTER, MANGALORE. 3 Course of study and Master of Physiotherapy (MPT) Subject 2 years Degree Course. “Physiotherapy in musculoskeletal and sports.” 4 Date of Admission 04/05/2010. To course 5 Title of the Topic Test – Retest Reliability, Construct Validity and Responsiveness of Manchester Foot Pain and Disability Index, Foot Functional Index and Plantar Fasciitis Pain and Disability Scale in Subjects with Plantar Fasciitis.
1 6. Brief resume of the intended work: 6.1 Need for the study The plantar fascia is an extremely strong connective tissue band spanning the bottom of the foot. One of the most common causes for heel pain is plantar fasciitis. Plantar fasciitis is the tearing and inflammation and subsequent degeneration of the fascia. This is a result of small micro tears in the fascia. A spur can develop as a result the traction force from the fascia, but the heel spur is rarely the cause of pain.1 The initial phases of plantar fasciitis are inflammatory, involving pain and swelling. As the condition progresses and becomes chronic, the inflammation slowly disappears and the plantar fascia starts to deteriorate, becoming a condition called plantar fasciosis.2 Classic descriptive terms for plantar fasciitis include burning, tearing sensations; sharp shooting pain and dull ache.1 Due to pain, this pathology leads to functional limitations in the daily living activity of people. Mostly, those people are more exposed to this condition are involved in prolong weight bearing activities, excess foot pronation, limited dorsiflexion and obesity.3-5 Prevalence of this condition is seen more in females, as they are more involved in prolong standing and people and are above the age of 45 yrs.6,7 Two types of treatment are available for this condition .i.e. conservative and surgical. In conservative treatment, drugs8 and physiotherapy along with orthotic management plays major role9,10 and when it fails then we switch for the surgical treatment i.e. release of the fascia.11 There are several scales devised to access the foot pain and disability for different conditions of foot.12 The common scale used to access foot pain and disability in plantar fasciitis is foot functional index (α=0.96 – 0.76).13, 14 But there is a Manchester foot pain and disability index 15 (α=0.89) and plantar fasciitis pain and disability scale16, which is newly devised scale specifically based on the symptoms of plantar fasciitis. Some of these scales have been used in the patients with rheumatoid arthritis,17, 18
2 for generalized foot pain and for elderly people and not in exclusive plantar fasciitis patients. Further, the test - retest reliability of plantar fasciitis foot pain and disability scale (PFPS) has not been done in subjects with plantar fasciitis. Even the construct validity of PFPS and MFPDI is also not found till now in the published research. The responsiveness of MFPDI, FFI and PFPS has also not been done in subjects with plantar fasciitis. So there is a need to draw conclusion that whether these scales have affinity to measures pain and disability in subjects with plantar fasciitis or not as these scales are specific to the symptoms of plantar fasciitis.
Hence, the purpose of this study is to find out the test – retest reliability, construct validity and responsiveness of Manchester foot pain and disability scale (MFPDI), Foot functional index (FFI) and Plantar fasciitis pain and disability scale (PFPS) for the subjects with plantar fasciitis and to access pain, function, foot wear and general foot health.
6.2 Review of Literature: 1. Willis et al. (2009) conducted a study to examine the plantar fasciitis pain and disability scale (PFPS) and its ability to discriminate between pain from PF and other heel pain. It is a 19 item scale with domains measuring foot pain and mobility/function and it was concluded that the existing pain scales are effective in gauging overall pain, but they lack the specific inclusion of symptomatic questions that will allow specific, objective, analytical measurement of change in symptoms unique to PF. The PFPS effectively showed the difference between PF patients vs. patients with other pathologies causing heel pain.16 2. Hill et al. (2008) conducted a study to determine the prevalence, correlates and
3 impact of foot pain in a population-based sample of people aged 18 years and over living. They concluded that foot pain is associated with increase in age, female sex, obesity and pain in other body parts which further affect the quality of life.6 3. Irving et al. (2007) examined the association between chronic plantar heel pain (CPHP) and a number of commonly hypothesized causative factors and found that obesity and pronated foot posture are associated with CPHP and may be the risk factors for the development of this condition. Further they confirmed that decreased ankle dorsiflexion, calf endurance and occupational lower limb stress may not play a role in CPHP. 4 4. Cook et al. (2007) conducted a study to calibrate the 17 items of MFPDI and to validate it. It was concluded that by reducing the MFPDI to 16 items, the Modified MFPDI is multidimensional and is associated with the underlying construct of activity related foot and ankle disability and pain and appearance. By reducing the MFPDI to 16 items, a clinician can be confident that the outcome instrument accurately represents the latent construct of disability and pain and appearance. 5. Menz et al. (2006) did a study to confirm the high prevalence of disabling foot pain in older people and to check the psychometric properties of MFPDI. It was concluded that MFPDI is a suitable tool for assessing foot pain in older population with high value of internal consistency i.e. α=0.89. 15 6. Lemont et al. (2003) reviewed histological findings from 50 cases of heel spur surgery for chronic plantar fasciitis. Their findings included myxoid degeneration with fragmentation and degeneration of the plantar fascia and bone marrow vascular ecstasies. Histological findings are presented to support the thesis that "plantar fasciitis" is a degenerative fasciosis without inflammation, not a fasciitis. These findings suggest that treatment regimens such as serial corticosteroid injections into the plantar fascia should be reevaluated in the absence of inflammation and in light of their potential to induce plantar fascia rupture. 1 7. Lynch et al. (1999) conducted a randomized, prospective study to compare the individual effectiveness of three types of conservative therapy in the treatment of plantar fasciitis. For the 85 patients who completed the study, a statistically
4 significant difference was noted between groups, with mechanical treatment with taping and orthoses proving to be more effective than either anti-inflammatory or accommodative modalities. 9 8. Budiman-Mak et al. (1991) conducted a study to check the reliability and validity of foot function index (FFI) and is one of the methods to measure the impact of foot pathology on function in terms of pain, disability and activity restriction and a strong correlation was found between the FFI total and sub-scale scores (α=0.96 – 0.73). Clinical measures of foot pathology supported the criterion validity of the index. Hence, FFI should prove useful for both clinical and research purposes.13 9. Jaeschke et al. (1989) conducted a study to overcome one of the challenges facing the investigator using such measures in determining the significance of any differences observed, and communicating that significance to clinicians who will be applying the trial results. Hence, authors have developed an approach to elucidate the significance of changes in score in quality of life instruments by comparing them to global ratings of change. Using this approach they have established a plausible range within which the minimal clinically important difference (MCID) falls.17
6.3 Objective of the study To evaluate the Construct Validity , test–retest reliability and to check the responsiveness of the following Clinical scales in subjects with plantar fasciitis :- 1) Manchester foot pain and disability scale(MFPDI).15 2) Foot functional index (FFI).13 3) Plantar fasciitis pain and disability scale(PFPS).16
6.4 Hypothesis: Experimental hypothesis: Based on GROC rating scale 19, the subjects rating between -2 to+2 are “stable” and above ≥+3 are “larger” clinically improved groups and subjects would have clinical significant changes in MFPDI, FFI and PFPS scores. Null hypothesis:
5 Based on GROC rating scale19, the subjects rating between -2to+2 are “stable” and above ≥+3 are “larger” clinically improved groups and subjects would not have clinical significant changes in MFPDI, FFI and PFPS scores .
Material and Methods: 7.1 Source of data: About 45 subjects will be participating in this study, who have been diagnosed as plantar fasciitis. Subjects will be taken from Srinivas college of physiotherapy. Sampling: - Convenient sampling.
7.2 Method of collection of data: 1.Subjects will be selected according to the inclusion criteria and consent form will be filled by the subjects stating the voluntary participation in this study. The subjects will be informed about the procedure. 2. Then 3 questionnaires i.e. MFPDI 15, FFI 13 and PFPS 16 will be given to the subject to fill as the baseline examination. 3. After the baseline examination, the subjects will be treated with the standardized treatment protocol for 10 days 20 which include ultrasound, contrast bath and exercises. 4. Then again, those 3 scales i.e. MFPDI, FFI and PFPS are given to the subject to fill, at the time of completion of the treatment or follow up along with GROC scale 19. 6. With the help of GROC scale 19, subjects will be graded into 4 groups i.e. unchanged, stable, smaller and moderately better depending upon the response to the treatment.
Inclusion Criteria 1. Age:-Above 45yrs. 2. Medically diagnosed plantar fasciitis subjects. 7. 3. Subjects should be actively participating in the study.
6 4. Subjects pain in the plantar aspect of the heel. 5. Pain in the heel on the first step in the morning. 6. No history of resting pain in plantar aspect of heel. 7. Subjects should not have any other neuromuscular problem. 8. Subject willing to take treatment. Exclusion Criteria 1. Age: - Below 45 yrs. 2. Subjects with other neuromuscular deficits. 3. Subjects with infective diseases of lowerlimb. 4. Subjects with impaired lower limb circulation. 5. Corticosteroid injection in heel, preceding 3 months. 6. Subjects with history of foot fractures. 7. Subjects with neuromuscular injuries of foot. 8. Subjects not willing to participate in study.
Statistical analysis Study design:- Single group repeated measure design.
TEST: 1. Test – retest reliability: - ICC 2. Construct validity : - 3 separate 2-way analysis of Variance. 3. Responsiveness : - Standard Responsiveness Mean and Standard Error.
7.3 Does the study require any investigations or interventions to be conducted on patients or other humans or animals? If so please describe briefly. YES. This study intends to use the scales to assess the treatment in subjects with plantar fasciitis.
7 7.4 Has ethical clearance been obtained from your institution in case of 7.3? YES. Consent has been taken from the institution ethical committee.
List of references:- 1. Paul Langer. Foot conditions and injuries. Chapter no. 4. Great Feet for Life: Foot care and Footwear for Healthy Aging, Edition 1. Fairview Press, 2007;62. 2. Harvey Lemont, Krista M. Ammirati and Nsima Usen. Plantar Fasciitis A Degenerative Process (Fasciosis) Without Inflammation. J Am Podiatr Med Assoc 2003;93(3):234-7. 3. Javier Pascual Huerta, Juan Maria Alarcon Garcia, Eva Cosin Matamoros, Julia Cosin Matamoros and Teresa Diaz Martinez. Relationship of Body Mass Index, Ankle Dorsiflexion, and Foot Pronation on Plantar Fascia Thickness in Healthy, Asymptomatic Subjects. J Am. Podiatr. Med Assoc. 2008;98(5):379– 85. 4. Damien B Irving, Jill L Cook, Mark A Young, Hylton B Menz. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskeletal Disorders. 2007;8:41. 5. Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003;85-A (7):1338. 6. Catherine L Hill, Tiffany K Gill, Hylton B Menz, Anee W Taylor. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. Journal of foot and ankle research. 2008 July;1:2. 7. Martin J. Thomas, George Peat and Edward Roddy. The population prevalence of foot and ankle pain over the age of 45 yrs: A Systematic review. Rheumatology. Oxfordjournals.org. 2010;49(1)147-52. 8. F. Crawford, D. Atkins, P. Young and J. Edwards. Steroid injection for heel pain: evidence of short term effectiveness. A randomized control trial. British
8 society of rheumatology. 1999; 38:974-7. 9. DM Lynch, WP Goforth, JE Martin et.al. Conservative treatment of plantar fasciitis. A prospective study. Journal of the American Podiatric Medical Association. 1998;88(8):375-80. 10. Stephen F. Conti, Deepek K. Jain. Managing plantar fasciitis and other 8. heel pain. Journal of Musculoskeletal Medicine 2009;26:106-12. 11. Craig C young, Darin S. Rutherford, Mark W. Niedfeldt. Treatment of plantar fasciitis. American family physician. 2001; 63(3):467-74. 12. Marike Van Der Leeden, Maitijn P.M. Steultjens, Caroline B. Terwee, Dieter Rosenbaum. A Systematic Review of Instruments Measuring Foot Function, Foot Pain, and Foot-Related Disability in Patients with Rheumatoid Arthritis. Arthritis & Rheumatism (Arthritis Care & Research). 2008 September; 59(9):1257–69. 13. Budiman-Mak E, Conrad KJ, Roach KE .The Foot Function Index: a measure of foot pain and disability. J Clin. Epidemiol. 1991;44(6):561-70. 14. Karl B. Landorf, Anne-Maree Keenan, Robert D. Herbert. Effectiveness of Foot Orthoses to Treat Plantar Fasciitis: A Randomized Trial. Arch Intern Med. 2006;166:1305-10. 15. H.B. Menz, A. Tiedemann, M.M.S. Kwan, K Plumb, SR Lord. Foot pain in community-dwelling older people: an evaluation of the Manchester Foot Pain and Disability Index. Rheumatology Advance Access publication. 2006;45:863–7. 16. Buck Willis, Angel Lopez, Andres Perez, Larry Sheridon, Stanley R Kalish. Pain Scale for Plantar Fasciitis. The Foot and Ankle Online Journal. 2009;2(5):3. 17. E. de. P. Magalhaes, M. Davitt, D.J Filho, L.R Battistella and M. B. Bertolo. The effect of foot orthoses in Rheumatoid Arthritis. Rheumatology. 2006;45(4):449-553. 18. Bowen J.C, Edwards J.C, Hooper L, Dewbury K, Sampson M, Sawyer S et al. Improvement in symptoms and signs in forefoot of patients with Rheumatoid
9 Arthritis treated with anti TNF therapy. Journal of Foot and Ankle research. 2010;3:1-9. 19. Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clinical Trials. 1989;407- 15. 20. Suman Kuhar, Khatri Subhash, Jeba Chitra. Effectiveness of Myofascial Release in Treatment of Plantar Fasciitis: A RCT. Indian Journal of Physiotherapy and Occupational Therapy. 2009;1(3).
10 9 Signature of the candidate
10 Remarks of the guide Study is feasible to conduct and innovative
11 Name & Designation of:
11.1 Guide Dr. KARTHIKEYAN G. Associate Professor in Physiotherapy
11.2 Signature
11.3 Co-Guide (If Any) DR. RAMPRASAD M. Professor in Physiotherapy
11.4 Signature
DR. T. JOSELEY SUNDERRAJ 11.5 Head of the Department PANDIAN Associate professor in Physiotherapy and PG coordinator 11.6 Signature
12 DR. RAM PRASAD 12.1 Remarks of Chairman and Principal and professor in physiotherapy. Principal Accepted by the scientific and ethical committee
12.2 Signature
11