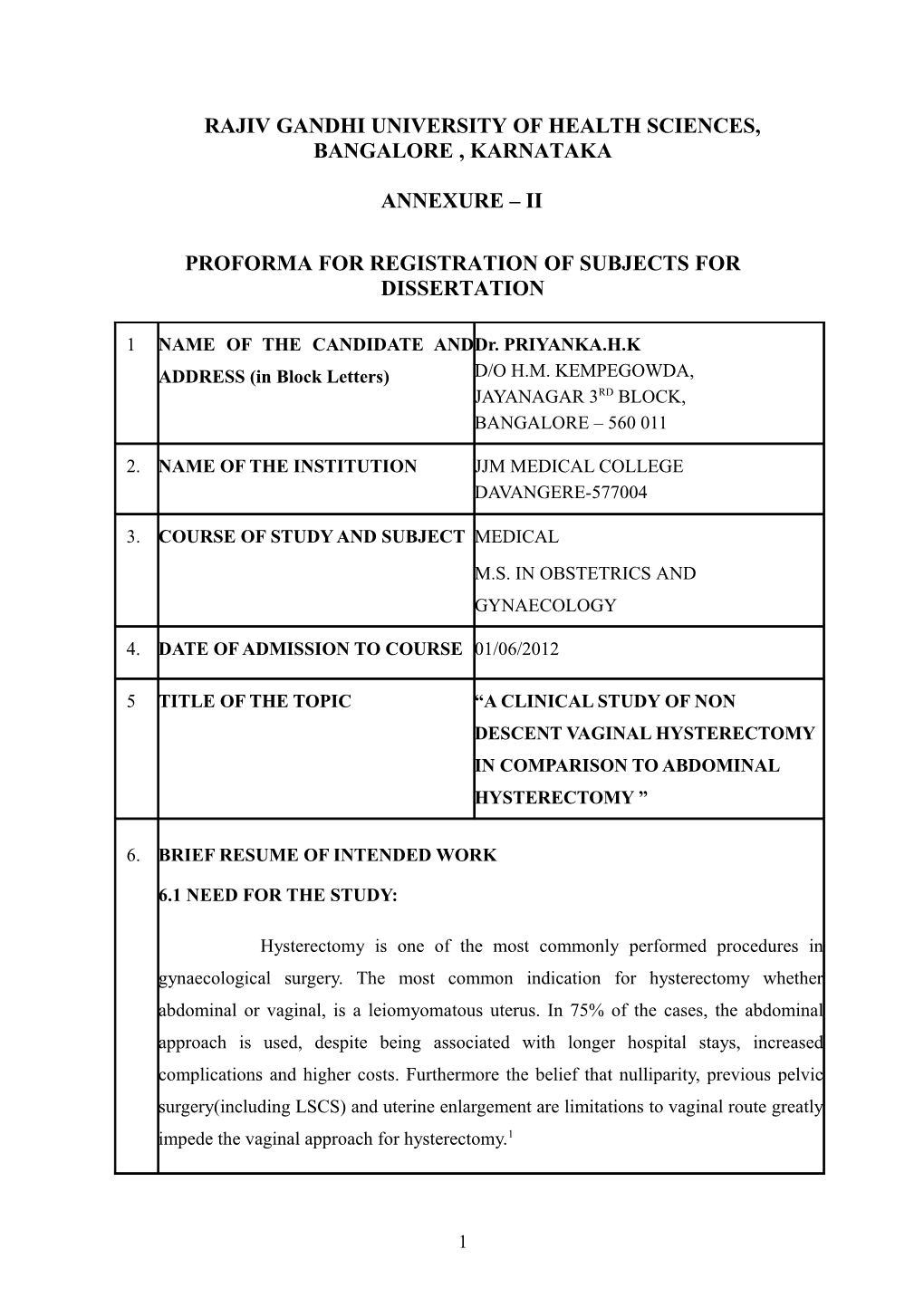
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE , KARNATAKA
ANNEXURE – II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1 NAME OF THE CANDIDATE ANDDr. PRIYANKA.H.K ADDRESS (in Block Letters) D/O H.M. KEMPEGOWDA, JAYANAGAR 3RD BLOCK, BANGALORE – 560 011
2. NAME OF THE INSTITUTION JJM MEDICAL COLLEGE DAVANGERE-577004
3. COURSE OF STUDY AND SUBJECT MEDICAL M.S. IN OBSTETRICS AND GYNAECOLOGY
4. DATE OF ADMISSION TO COURSE 01/06/2012
5 TITLE OF THE TOPIC “A CLINICAL STUDY OF NON DESCENT VAGINAL HYSTERECTOMY IN COMPARISON TO ABDOMINAL HYSTERECTOMY ”
6. BRIEF RESUME OF INTENDED WORK
6.1 NEED FOR THE STUDY:
Hysterectomy is one of the most commonly performed procedures in gynaecological surgery. The most common indication for hysterectomy whether abdominal or vaginal, is a leiomyomatous uterus. In 75% of the cases, the abdominal approach is used, despite being associated with longer hospital stays, increased complications and higher costs. Furthermore the belief that nulliparity, previous pelvic surgery(including LSCS) and uterine enlargement are limitations to vaginal route greatly impede the vaginal approach for hysterectomy.1
1 Therefore there is a need for expanding the use of vaginal hysterectomy rather than restricting it to the conventional indication of uterovaginal prolapse.
6.2 REVIEW OF LITERATURE:
1. Alokananda et al (2011) conducted a study to check the feasibility of the vaginal route as the primary route for all hysterectomies in the absence of uterine prolapse, for benign conditions. Patients were classified into 2 groups. Group 1 consisted of patients with uterine size upto 12 weeks with no risk factors and group 2 of patients with uterine size upto 12-18weeks or with confounding risk factors. The outcome was compared between the 2 groups and abdominal hysterectomies done for benign conditions and was measured in terms of operating time. peroperative blood loss, pain score, hospital stay and return to normal activity. The result was that vaginal approach is possible in most benign conditions requiring hysterectomy and is superior to the abdominal route with respect to recovery and complication rates.
2. Sunanda Bharatnur (2011) conducted a comparative study of abdominal versus vaginal hysterectomy in non descent cases and compared the risks in the intra operative and post operative period.25 patients were included in group A who underwent abdominal hysterectomy and 25 patients in group B who underwent vaginal hysterectomy. It was found that intra-operative blood loss and mean operating time was more in group A and post operative fever(28% & 16%),UTI(20% & 15%) and wound infection(8% & 0%)was more common again in group A. Hence it was concluded that patients requiring hysterectomy for benign non prolapsed cases be offered the option of vaginal route which is less invasive, minimal or no complications, more economical and effective.
3. Bhadra et al (2011) conducted a study wherein non descent vaginal hysterectomy was performed in 158 cases with prerequisites’ of uterine size not exceeding 20weeks gestation, mobile uterus and adequate vaginal access with no uterine prolapse. Volume reduction techniques were used during surgery. An observation of mean operating time of 55 minutes. mean blood loss of 100ml and average duration of hospital stay of 3 days with minimal complications was noted. It was concluded that vaginal hysterectomy for non descent large uterus was safe and feasible
2 provided one was familiar with debunking procedures.
4. Dr Abha Singh and Shweta Bansal (2006) compared the efficacy of vaginal hysterectomy with that of abdominal hysterectomy in non prolapsed uteri. It was a prospective study carried out on 100 women with group A consisting of 50 women operated by vaginal route and group B of 50 women operated by, the abdominal route. Outcomes measured were mean time taken, mean blood loss and mean hospital stay. It was found that there was a statistically highly significant difference in the mean time taken (P < 0.001), mean blood loss (P < 0.001) and mean hospital stay (P< 0.01) favoring vaginal hysterectomy. Study concluded that vaginal hysterectomy whenever feasible should be preferred over abdominal hysterectomy even when uterine size is >12 weeks size, cervix is flushed with vagina, subpubic angle is narrow and there is history of previous pelvic surgery.
5. Susan M Taylor et al(2003) compared the intra operative and postoperative complications of abdominal hysterectomy for the enlarged myomatous uterus with vaginal hysterectomy with morcellation. Medical records of 139 patients who underwent vaginal hysterectomy were compared with 244 patients of abdominal hysterectomy. It was found that the operating time was similar between the 2 groups whereas the length of hospital stay and perioperative complications were increased with the abdominal route. They concluded that, uterine morcellation at the time of vaginal hysterectomy is safe and facilitates the removal of moderately enlarged and well supported uteri and is associated with decreased hospital stay and perioperative morbidity compared with the abdominal route.
6. L.Benassi et al(2002) compared the advantages, disadvantages and outcomes in patients who undergo vaginal or abdominal hysterectomy for enlarged symptomatic uteri. A study group of 60 vaginal hysterectomies were compared with a control group of 59 abdominal hysterectomies. The evaluated parameters were patient age, weight, parity, uterine weight, operative time, blood loss, demand for analgesics, surgical complications, length of hospital stay and hospital charges. It was found that the operative time was significantly lower for the vaginal route and no intraoperative complications were noted in the study and control groups. Surgical bleeding was not significantly different between the 2 groups but there was a higher
3 demand for analgesics in the abdominal group whereas a reduction in hospital stay was noted in the vaginal group. The conclusion was that ,vaginal hysterectomy was a valid alternative to abdominal hysterectomy even for enlarged uteri.
6.3 OBJECTIVES OF STUDY:
To study the role of vaginal hysterectomy in non descent uterus and compare it with abdominal hysterectomy with respect to operative time, intra operative blood loss, intra operative complications and hospital stay.
7. MATERIALS AND METHODS
7.1 Source of data
Hospital attached to JJM medical college:
Bapuji Hospital,Davangere.
Chigateri General Hospital,Davangere.
Women and Child Hospital,Davangere.
Duration of study-Nov 2012 to Oct 2014
7.2 Methods of collecting data
Design-Prospective study
Number of cases-100
Vaginal hysterectomy(study group)-50
Abdominal hysterectomy(control group)-50
Inclusion Criteria
• Uterine size less than 16 weeks
• Previous pelvic surgery-including previous 1 or 2 LSCS.
• Good Uterine mobility
• Pathology confined to the uterus(no adnexal pathology)
4 Exclusion Criteria
• Uterine prolapse
• Malignancy-suspected or diagnosed
• Pelvic inflammatory disease
• Severe endometriosis
Procedure of study:
Patients are selected according to the inclusion criteria. They are then divided into vaginal group and abdominal group. Routine investigations including complete haemogram, urine analysis., blood grouping and Rh typing, random blood sugar, blood urea, serum creatinine, ECG, USG abdomen and pelvis, HIV,HBsAg will be carried out.
Operating time for vaginal hysterectomy will be calculated as time taken from the start of incision at cervico-vaginal junction to placement of vaginal pack and for abdominal hysterectomy it will be calculated as time taken from the start of skin incision to closure of skin incision.
Blood loss will be estimated by preoperative and post operative(day 2) haemoglobin and haematocrit measurement and by estimating the weight of mops pre-op and post operatively.
Intra operative complications such as injury to bowel/bladder or ureter and haemorrhage will be noted. Post operatively all patients will be followed up for early complications like fever, post operative pain, urinary tract infection and abdominal wound infection.
Duration of hospital stay will also be noted and calculated as number of days in hospital after the surgery including the day of surgery.
The patients will be reviewed in the outpatient department 4weeks following discharge for post operative follow up.
7.3 Does the study require any investigations or interventions to be conducted on patients or other humans or animals? If so describe briefly.
5 Investigations
Complete Hemogram
Urine Analysis
Blood Group and Rh Typing
RBS
Blood Urea, Serum Creatinine
ECG
USG – Abdomen and Pelvis
HIV – HBs Ag.
7.4 Has ethical clearance been obtained from your institution in case of 7.3?
Yes
8. LIST OF REFERNCES:
1) Paparella P. Sizzi O, Rossethi A et al . Vaginal hysterectomy in generally considered contraindications to vaginal surgery. Arch Gynecol Obstet 2004; 270:104-9.
2) Dr Abha singh and Shweta bansal:Vaginal hysterectomy for non prolapsed uterus.J Obstet Gynaecol India Vol 56,No 2:March/April 2006;152-15.
3) L.Benassi MD,T.Rossi,MD,C.T.Kaihura,MD,L.Ricci,MD,
4) L.Bedocchi,MD,B.Glanti,MD and E.Vadora,MD-Abdominal or vaginal hysterectomy for enlarged uteri-A randomized clinical trial.Am J Obstet Gynaecol December 2002:vol 187,Number 6;1561-1565
5) Alokananda ray,Pant Luna,Balsara Roshan,Chaudary Rashmi-Non descent Vaginal Hysterectomy: A Constantly Improving Surgical Art.J Obstet Gynaecol India March/April 2011:pg 182-188
6 6) Susan M Taylor, MD, Audrey A. Romero,MD, Dorothy N. Kammerer-Doak, MD, Clifford Qualls, PhD and Rebecca G. Rogers, MD-Abdominal hysterectomy for the enlarged myomatous uterus compared with vaginal hysterectomy with morcellation.Am J Obstet Gynaecol December 2003:Vol 189 Number 6;1579-1583
7) Sunanda Bharatnur: Comparative study of Abdominal versus Vaginal Hysterectomy in Non Descent cases: The Internet Journal of Gynaecology and Obstetrics 2011 Volume 115 Number 2.DOI:10.5580/293f
8) ACOG Committee opinion:Choosing the route of hysterectomy for benign disease.Number 444,November 2009
9) Banasree bhadra,Arun Paul Choudury,Amit Tolasaria and Nandi Nupur:Non Descent Vaginal Hysterectomy:Personal Experience in 158 cases.Al Ameen J Med Sci(2011)4(1)23-27.
7 9. SIGNATURE OF THE CANDIDATE
10. REMARKS OF THE GUIDE Very useful study to reduce the complications and is cost effective and helpful to learn the vaginal route of hysterectomy.
11. NAME & DESIGNATION
11.1 GUIDE Dr. T.G. SHASHIDHAR MD., DGO Professor & HOD, Dept. of Obstetrics and Gynaecology JJM Medical College, Davangere
11.2 SIGNATURE
11.3 CO-GUIDE (If any) Dr. LAKSHMIDEVI K. MD., Professor Dept. of Obstetrics and Gynaecology JJM Medical College, Davangere
11.4 SIGNATURE
11.5 HEAD OF THE DEPARTMENT Dr. T.G. SHASHIDHAR MD., DGO Professor & HOD Dept. of Obstetrics and Gynaecology JJM Medical College, Davangere 11.6 SIGNATURE
12 REMARKS OF THE CHAIRMAN & PRINCIPAL
12.1 SIGNATURE
8