Osteoporosis: Guidelines for Screening and Treatment
These guidelines are informational only and are not intended to substitute for the reasonable exercise of independent clinical judgment of the providers using the guideline. The guidelines are to be used in conjunction with the provider's clinical judgment in developing care and treatment that is designed for the individual needs of the patient.
Date: April 6, 2018
Title: Osteoporosis: Guidelines for Screening and Treatment
Rationale:
This is a consensus-based guideline. Although many studies have been published about osteoporosis treatment in postmenopausal women, no trials have evaluated the effectiveness of osteoporosis screening; therefore, no direct evidence that screening improves outcomes is available. Recommendation for screening is based on the following three points: 1) The risk of osteoporosis increases with advancing age; 2) Accurate screening tests for osteoporosis exist; 3) High quality trials have demonstrated the efficacy of bisphosphonates in preventing hip fractures and selective estrogen- receptor modulators (SERMS, e.g., raloxifene) in preventing vertebral fractures in women with osteoporosis.
Osteoporosis risk:
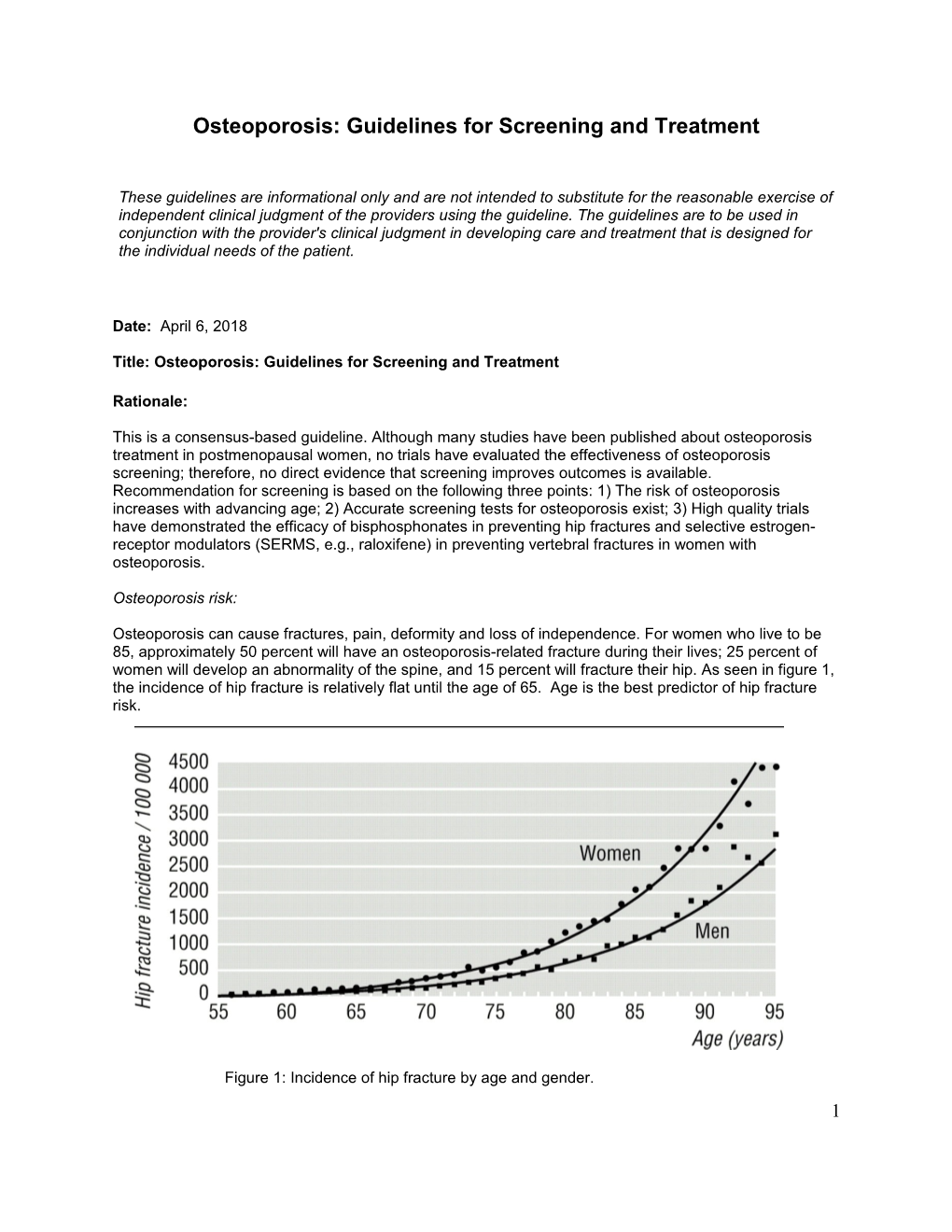
Osteoporosis can cause fractures, pain, deformity and loss of independence. For women who live to be 85, approximately 50 percent will have an osteoporosis-related fracture during their lives; 25 percent of women will develop an abnormality of the spine, and 15 percent will fracture their hip. As seen in figure 1, the incidence of hip fracture is relatively flat until the age of 65. Age is the best predictor of hip fracture risk.
Figure 1: Incidence of hip fracture by age and gender. 1 (De Laet CE, etal., BMJ 1997;315:221-225) Of the many risk factors associated with osteoporosis, age, weight and HRT use best predict fracture risk. Twelve to 28 percent of women 65 and older have osteoporosis; this proportion increases with age. Women age 60-64 that are in the lowest quartile of weight and not using HRT have a risk of fracture similar to that of women over age 65. Women age 65 who have been continuously on HRT since menopause have greater bone density values than women who have never been on HRT, yet still have a significant fracture risk: 20% of these women will have a nonvertebral fracture in the subsequent ten years (Nelson et al. 2002a).
There is less evidence to support the use of other individual risk factors (e.g., smoking, decreased physical activity or family history of fracture) in determining who should undergo bone mineral density (BMD) screening. Age, weight and HRT use has been shown to have greater sensitivity and specificity than models that include a greater number of risk factors (Cadarette et al. 2001).
Men also experience age related declines in BMD but at a much slower rate than do women. Fractures due to osteoporosis occur, on average, 10-15 years later in men. Most osteoporosis in men is due to secondary causes (30-60%), primarily hypogonadism, glucocorticoid use and alcoholism. Evaluation for osteoporosis should be considered in men with these conditions.
Persons on glucocorticoid therapy are at increased risk for bone density loss. There are few studies on the use of BMD screening or bisphosphonate therapy for patients on long-term glucocorticoid therapy. One randomized trial of alendronate therapy for men and women ages 17-83 taking ≥ 7.5 mg glucocorticoid for at least one year did find increased bone densities and reduced vertebral fractures associated with up to two years of alendronate use. Recommendations for patients using lower doses of glucocorticoids (i.e., 5-7.4 mg/day) for shorter periods (e.g., 3-6 months) are based on expert opinions; variation in practice exists across our own specialty groups (e.g., pulmonology, rheumatology, allergy, and endocrinology).
Re-review of multiple studies resulted in a black box warning for Depo-Provera. Studies suggest lower BMD scores after more than two years of use, however, the clinical significance is unknown. It is unclear if the bone mass repairs completely after discontinuation, or if these women are at increased risk of osteoporosis later in life after earlier Depo-Provera use. BMD testing is not useful in evaluating bone in young women and is not usually recommended.
Osteoporosis screening:
Dual-energy x-ray absorptiometry (DEXA), a non-invasive test, is the most accurate method for measuring bone density, and is the best predictor of hip fracture. The published trials of bisphosphonate efficacy were based on osteoporosis diagnoses made using the DEXA test. No trials of the effectiveness of screening have been published.
The World Health Organization defines osteoporosis as bone mineral density values 2.5 standard deviations (SDs) or more below the mean for healthy young adult women at the spine, hip, or wrist (corresponding to a T-score of < ‾2.5) or when patients have a history of an atraumatic fracture. Osteopenia is defined as a T-score between ‾1.0 and ‾2.5. By the World Health Organization definition, up to 70 percent of women older than 80 years of age have osteoporosis. Age is an important factor in the relationship between bone density and the absolute risk for fracture. Older women have a much higher fracture rate than younger women with the same bone density because of increasing risk from other factors, such as bone quality and tendency to fall.
Osteopenia:
Little is known about how best to manage patients with osteopenia (T-scores between ‾1.0 and ‾2.5). One randomized clinical trial enrolling women with T scores < ‾1.5 and no history of previous fracture has
2 been completed, testing the efficacy of alendronate in preventing fractures (FIT II). Only the subgroup of women with T scores less than ‾2.5 had a significant risk reduction for all clinical fractures. No reduction in fractures was seen in patients who had T-scores between ‾1.6 and ‾2.5.
Screening risks:
Several potential harms are associated with screening and treatment. A test result indicating osteoporosis could produce anxiety and perceived vulnerability that may be unwarranted. On a quality-of-life questionnaire, women with osteoporosis voiced significantly more fears than women who had normal bone density. The personal costs in time, effort, expense, and radiation exposure of repeated scans over a lifetime have not yet been determined.
Potential harms may also arise from inaccuracies and misinterpretations of bone density tests. The variation among techniques, along with the lack of methods to integrate bone density results with clinical predictors, makes it difficult for clinicians to provide accurate information to patients about test results. False-positive results could lead to inappropriate treatment, and false-negative results could lead to missed treatment opportunities.
Treatment with bisphosphonates is associated with GI upset and esophagitis (< 1%). In the bisphosphonate trials, in which women with known esophageal reflux were excluded, rates of GI side effects were the same (25%) in the treatment and control arms. This suggests that some of the GI upset seen among patients taking alendronate is a reflection of the high background rate of reflux in this population. In one study, 85% of patients rechallenged with alendronate 30+ days after discontinuation of the medication had no recurrence of these symptoms (Miller et al. 2000). The safety of long-term bisphosphonate therapy has not been studied; long-term adverse effects are unknown.
Screening frequency:
How frequently to screen has also not been specifically studied. Estimations can be made based on the age-specific prevalence of osteoporosis and the precision of bone density tests. Less frequent testing for younger women when prevalence is lower and more frequent testing for older women is reasonable. Screening intervals of less than 2 years is unwarranted because the precision error of densitometry would likely exceed the estimated bone loss in such a brief period (exception: patients initiating long-term glucocorticoids not on bisphosphonates). In general, most postmenopausal women not on treatment (e.g., HRT, bisphosphonates) lose about 0.5 T score units every 5 years (.1 unit annually).
After a woman is screened, determined to have osteoporosis, and treated, future testing with bone density testing is unnecessary, as BMD results would not change medical management. Since bisphosphonate therapy reduces fractures by 30-50% (not 100%), one should expect fractures to occur among some women taking bisphosphonates. Consider evaluation for secondary causes of osteoporosis among women who fracture while on bisphosphonate therapy (see below). Consideration of more aggressive medical management could prompt an endocrine referral.
Secondary causes of osteoporosis:
Osteoporosis due to secondary causes is rare. The Z score of the BMD test can be helpful in identifying a population for further evaluation for secondary causes of osteoporosis. The Z score is based on the standard deviation from the mean BMD of a reference population of the same sex, ethnicity and age. Consider looking for secondary causes in patients with Z scores less than or equal to ‾2.0. Steroid use (> 5 mg/day for 3 months or more) is associated with osteoporosis. Women with a history of anorexia nervosa are at increased risk of osteoporosis and fractures later in life; there have been no studies published on the use of bisphosphonates among women with a history of anorexia. A small clinical trial of 3 estrogen-progestin given to anorexic girls did not find an improvement in bone density. Other secondary causes of osteoporosis to consider include hyper-parathyroidism, renal calcium leak, malabsorbtion/celiac sprue, inadequate calcium intake, Vitamin D deficiency, multiple myeloma, hyperthyroidism, and Cushing syndrome. Such conditions may warrant consultation.
Number needed to screen (NNS) and number needed to treat (NNT):
The following estimates were made by the U.S. Preventive Services Task Force (USPSTF) in their recommendations for osteoporosis screening (Nelson HD, et al., 2002b) and assumes 5 years of therapy with alendronate; 37% reduction in hip fracture; 50% reduction in vertebral fracture; and 70% adherence to drug therapy. The model demonstrates the impact of age on the value of BMD screening and treatment: the benefits of screening are greater for older patients than for younger patients.
AGE IN YEARS 50-54 55-59 60-64 65-69 70-74 75-79 Hip Fx NNS 7446 4338 1856 731 254 143 NNT 227 193 121 88 51 41 Vert Fx NNS 1952 1338 458 248 105 75 NNT 60 60 30 30 21 21
NNS: Number needed to screen to prevent one hip or vertebral fracture over 5 years NNT: Number needed to treat for five years to prevent one hip or vertebral fracture
Target Population: Women greater than 65 years; women 60-64 years with risk factors for osteoporosis; men and women with conditions associated with osteoporosis (e.g., glucocorticoid use).
Responsible party: Sue-Jane Fox, Prevention, [email protected], 303-344-7256, Karin Kempe MD, 303-344-7662, [email protected].
Approval: Chief, Preventive Medicine
Review Date: April 6, 2018
Source of evidence:
Screening for osteoporosis in postmenopausal women: Recommendations and rational, U.S. Preventive Services Task Force, Ann Intern Med. 2002; 137:526-528, also see: http://www.preventiveservices.ahrq.gov Sept. 16, 2002
Screening for postmenopausal osteoporosis: summary of the evidence, U.S. Preventive Services Task Force, http://www.preventiveservices.ahrq.gov Sept. 16, 2002
Cadarette, SM, et al., Canadian Medical Association Journal, May 2, 2002;162 (9);1289-1294
Osteoporosis prevention, diagnosis, and therapy, NIH Consensus development panel on osteoporosis prevention, diagnosis and therapy, JAMA 2001;285:785-795
Management of postmenopausal osteoporosis: position statement of the North American Menopause Society, Menopause: The Journal of the North American Menopause Society, 2002, 9;(2):84-101
4 Cadarett SM, et al. Evaluation of decision rules for referring women for bone densitometry by dual- energy X-ray absorptiometry. JAMA. 2001;286:57-63
Miller PD, Woodson G, et al. Rechallenge of patients who had discontinued alendronate therapy because of upper gastrointestinal symptoms. Clin Ther. 2000;22:1433-1442
Nelson HD, et al. Osteoporosis and fractures in postmenopausal women using estrogen. Arch Intern Med. 2002a;162:2278-2284.
Nelson HD, et al. Screening for postmenopausal osteoporosis: a review of the Evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002b;137:529-541.
Settings for Application: Internal Medicine, OB/GYN, and Family Practice departments.
Methods for measuring compliance: The following will be monitored: the number of people (men or women) undergoing BMD screening; the number of people on bisphosphonate therapy; the number of women on HRT. Additional measurements could include monitoring referrals for BMD by age and relative to the guideline, HEDIS measurement and the penetration of BMD screening in women age 65+.
5 Osteoporosis: Guidelines for Screening and Treatment
Primary prevention
All women should be counseled to take 1000-1500 mg of elemental calcium and 400-800 IU of vitamin D per day. Regular weight bearing exercise and weight training will promote bone health. Smoking cessation will improve bone health. Women over age 65 should get more than the minimum amount of both calcium and vitamin D. All patients should be advised on the principals of fall prevention (e.g., appropriate lighting and handrails).
The US Preventive Services Task Force recommends against the routine use of HRT for the prevention of chronic diseases (including osteoporosis) in post-menopausal women. Women interested in using HRT for osteoporosis prevention should discuss the risks and benefits of HRT use with their provider. Please see the Hormone Replacement Guideline for details.
Although bisphosphonates have been shown to increase bone mass in osteoporotic patients, there have been no studies showing their usefulness in primary prevention. At the present time they are not considered cost effective for primary prevention.
Secondary Prevention
I. Screening Population:
Screening with DEXA of the hip is indicated only for patients willing to undergo therapy should osteoporosis be detected. Women currently on bisphosphonates for osteoporosis do not need BMD testing. Women who, based on their provider’s judgement, would be started on therapy regardless of BMD do not need to be screened. At any given age, African American women on average have higher BMDs than white women and are thus less likely to benefit from screening; these patients may decide to undergo screening at a later age after discussion with their provider.
BMD screening is appropriate for postmenopausal women meeting above criteria and:
age > 65yrs, regardless of HRT use
age 60-64 and weight < 60kg, (132 lbs.), regardless of HRT use
age 60-64, weight 60-69kg (132 – 154 lbs.), and no current use of HRT
There is fair evidence (strength: B) supporting these recommendations. Fractures from osteoporosis in women under age 60 are rare (see figure 1); the harms from screening may outweigh the benefits for young postmenopausal women.
Women meeting the above criteria who are stopping HRT will experience a more rapid bone loss in the subsequent 2-3 years. Consider waiting 24 months before performing a screening BMD among eligible women who have discontinued HRT.
BMD screening should be considered:
for postmenopausal women with a fragility fracture (e.g., hip, vertebra, wrist)
for men and women on ≥ 5 mg of glucocorticoid for 3 months or more
6 for men with multiple risk factors (e.g., age > 75, previous atraumatic fracture, loss of height, hypogonadism, long-term glucocorticoid use or alcoholism)
It is reasonable to forgo BMD screening in these patients if the results would not influence the decision to begin medical therapy for fracture prevention.
II. Screening Frequency
No studies have been published on the appropriate frequency of BMD screening. The USPSTF makes no specific recommendations on screening frequency. Because of limitations in the precision of testing, repeat screening should not be done more often than every two years. Given that most women lose about 0.5 standard deviations from the mean in T scores every 5 years, the following frequency of screening is suggested:
T Score Range Time to next BMD test ‾ 1.0 and ‾ 1.5 5-10 years ‾ 1.5 and ‾ 2.0 5 years ‾ 2.0 and ‾ 2.5 3 – 5 years
Repeat testing can be ordered when the T score would be predicted to fall below ‾2.5 given the baseline T score and assuming an average rate of bone loss of 0.1 T score units annually. There are no data to determine the appropriate age to stop screening and few data on osteoporosis treatment in women older than 85 years of age.
For patients on chronic steroids (> 1 year) and no current medical therapy, a repeat DEXA test should be done one year after the initial test. If the result on the follow-up DEXA test is stable (< 3% loss), DEXAs should be repeated every two years.
Recommendations for treatment
Treatment is recommended for:
1. Postmenopausal women ≥ 50 years of age with a BMD < -2.5.
2. Postmenopausal women with a history of a fracture typical of osteoporosis at age > 50 years, (e.g. vertebrae, hip), and an increased risk for future fracture, defined either by a BMD score < -1.5 or by provider judgement (e.g., advanced age, low weight, height loss).
3. Preventive therapy is recommended for patients on ≥ 7.5 mg of glucocorticoids for ≥ 6 months; BMD screening is not necessary prior to starting medical therapy.
4. Consider alendronate therapy for patients who will be taking 5-7.4 mg/day of glucocorticoid or if the patient has other risk factors for ־for 3 months or more if BMD T score is < 1 osteoporosis (e.g., advanced age, smoking, history of prior fracture, no HRT use).
The preferred treatment is:
1. Alendronate 10 mg daily or 70mg weekly. Safety of treatment with Alendronate sodium for longer than four years has not been studied (extension studies are ongoing). Take upon arising before first food, drink or medications. Take with 6-8 oz. of water. Do not lie down for at least 30 minutes.
7 If Alendronate is not tolerated, discontinue therapy for 30 days and symptoms have resolved and then try again with the weekly or daily dose. Research suggests that 85% of patients are able to tolerate alendronate when restarted in this manner.
If alendronate cannot be tolerated or is contraindicated,
2. Raloxifene 60-mg daily may be administered any time of day without regard to meals. Raloxifene has been shown to reduce the risk of vertebral fractures; there is no evidence, however that it protects against hip fractures. The effect of Raloxifene on BMD beyond two years of treatment is not known at this time, but is being evaluated in ongoing clinical trials. One quarter of women taking raloxifene experience hot flashes and there is a 1% risk of deep vein thrombosis.
3. Although etidronate has not been shown to be effective for average risk postmenopausal women, it has been shown to improve BMD among patients on high-dose glucocorticoids. Patients on glucocorticoids who cannot tolerate alendronate due to GI symptoms can be treated with etidronate, a bisphosphonate with fewer GI side effects. Etidronate is given as 400mg q day two hours before eating on an empty stomach for two weeks, repeated every 3 months.
If the above therapeutic measures fail (fracture or height loss > 1.5 inches), an endocrinology consultation is appropriate; calcitonin may be considered after consultation. While calcitonin has been shown to increase bone density in postmenopausal women, there are no studies that demonstrate the efficacy of calcitonin in reducing fractures.
Alendronate therapy for women taking HRT:
Bone mineral density screening is indicated for women ≥ 65 years of age taking HRT. An observational study found that such women have a 20% risk of fracture in the subsequent ten years. Women taking HRT and found to have osteoporosis by BMD testing can continue on HRT in combination with alendronate. While there is some evidence that the combination of HRT and alendronate increase BMD more than alendronate or HRT alone, there are no studies looking at combination therapy on fracture incidence. Women taking HRT for lifestyle issues may not be willing to stop HRT when beginning alendronate.
8