2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test
1. The following are all physiologic changes that female patients experience during pregnancy:
a. Increased tidal volume, decreased blood volume and decreased heart rate
b. Increased tidal volume, increased blood volume and increased heart rate
c. Elevated diaphragm, decreased oxygen demand and increased heart rate
d. Elevated diaphragm, decreased oxygen consumption and decreased heart rate
2. The ______trimester of pregnancy is the most critical time for fetal organ development.
a. 1st
b. 2nd
c. 3rd
3. Hyperemesis gravidarum is associated with intractable nausea and vomiting for the pregnant patient, typically between 5-22 weeks gestation. Risks associated with this are:
a. Hyperkalemia
b. Hypernatremia
c. Excess fluid
d. B vitamin deficiencies
4. Symptoms associated with preeclampsia include all of the following EXCEPT:
a. Headache
b. Edema in the hands and face
c. Rapid weight loss
d. Hypertension
5. TRUE/FALSE – Eclampsia can occur up to six weeks post-partum and include presenting symptoms of pre-eclampsia, most commonly headache and then progress to seizures.
a. True
b. False 2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test
6. It can be estimated that a pregnant patient experiencing hemorrhage has had greater than ______ml of blood loss if her heart rate is greater than 140 with respirations greater than 35, hypotension, and altered mental status.
a. 1200
b. 1500
c. 1800
d. 2400
7. The leading cause of fetal death related to trauma during pregnancy is:
a. Abruptio Placenta
b. Placenta Previa
c. Supine Hypotensive Syndrome
d. Eclampsia
8. You, your partner, and an EMT student are returning from dropping a patient off at your local hospital when you witness a car crash into a light pole at an intersection. After calling it into dispatch, you assess the situation, the scene is safe, and there is a single driver in the vehicle that appears to be in her third trimester of pregnancy. She was restrained with airbag deployment, but appears to be unconscious. Carotid pulse is not palpable; C-collar applied and patient is properly extricated. With your call to dispatch setting other resources en route to you, your next action should be:
a. Attempt to intubate the patient as she is not protecting her airway.
b. Wait for back up.
c. Start chest compressions, while your partner opens her airway, delivering bag-valve mask ventilations at a 30:2 ratio, while also directing your student to manually displace the patient’s gravid abdomen to the left side of her body.
d. Load her into the ambulance and get back to the hospital as quickly as possible. 2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test
9. Which of the following is the cognitive (higher functions) region of the brain?
a. Cerebrum
b. Cerebellum
c. Brainstem
d. Parenchyma
10. Two types of Traumatic Brain Injury are:
a. Open and closed
b. Kinetic and hemorrhagic
c. Coup and closed
d. Cerebrum and cerebellum
e. ***BLS STOP HERE***
11. Which of the following is the term for the collection of white brain matter fibers that join the hemispheres?
a. Hemispheric scaffolding
b. Corpus Callosum
c. Medulla Oblongata
d. Circle of Willis
12. Which of the following would be the preferable (more discriminating) question regarding patient orientation (Maddocks Questions from the SCAT5 exam) for a patient with a sports-related TBI?
a. What day is it?
b. How many fingers am I holding up?
c. Who scored last in this game?
d. Do you feel like you can go back in the game? 2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test
13. Which of the following is the term that describes the extension and flexion of the arms following a significant head injury, often seen in athletes (and often preceding convulsions)?
a. Kehr’s Sign
b. Fencing Response
c. Beck’s Triad
d. Decerebrate Posturing
14. Factors that influence the pregnant patient’s increase in cardiac output by 40% are:
a. Increased stroke volume, increased heart rate and decreased systemic vascular resistance
b. Decreased stroke volume, increased heart rate and increased systemic vascular resistance
c. Increased stroke volume, decreased heart rate and increased progesterone levels
d. Decreased stroke volume, decreased heart rate and decreased progesterone levels
15. Changes in a pregnant patient’s 12-lead EKG from her normal are not uncommon due to uterine enlargement, pressing into the thoracic cavity. All of the following are common changes EXCEPT:
a. Left axis deviation
b. Premature ventricular contractions
c. Supraventricular tachycardia
d. Ventricular fibrillation
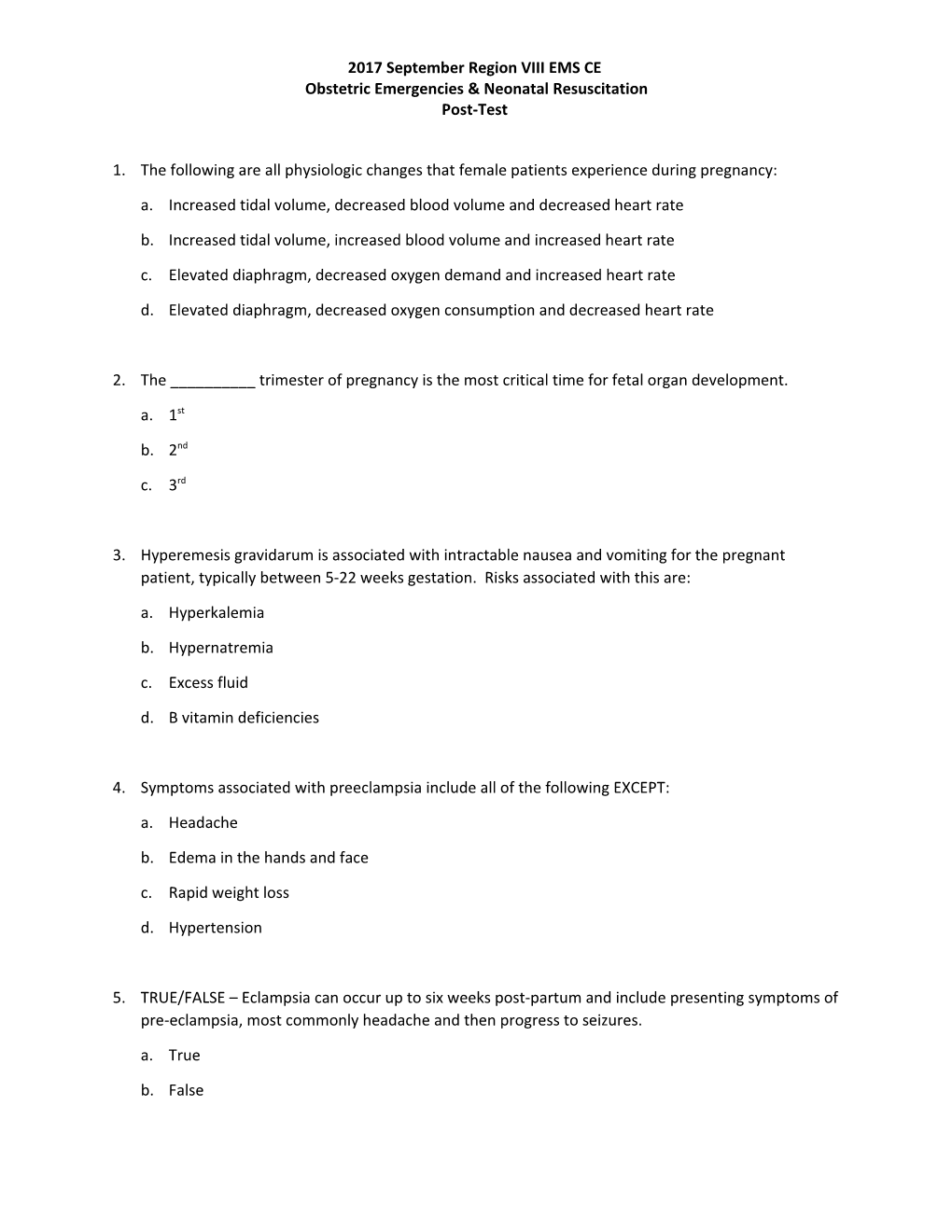
16. Which of the following waveforms would be considered a common/normal capnography finding in pregnancy?
a.
b. 2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test
c.
d.
17. ______is caused by a thiamin deficiency that is due to lack of nutrition, often displayed with a triad of symptoms: confusion, abnormal eye movements and unsteady gait.
a. Hyperemesis Gravidarum
b. Wernicke’s Encephalopathy
c. Pregnancy Induced Hypertension
d. HELLP Syndrome
18. You are dispatched for the 28 year old female that has complaints of vaginal bleeding during pregnancy. Upon arrival she states that she is 30 weeks pregnant with her first pregnancy. She has received prenatal care throughout her pregnancy. This morning, she noted bright red blood in her underwear when she woke up and called 911 right away. She denies any pain or discomfort. During your secondary assessment, her gravid abdomen remains soft, nontender. You suspect which of the following conditions:
a. Placenta previa
b. Abruptio placenta
c. TORCH Syndrome
d. HELLP Syndrome
19. You encounter a pregnant patient that has complaints of headache, nausea, joint pain and congestion. She appears to be poorly nourished and has not sought prenatal care. She is unsure how far along she is and admits to intravenous drug use. During your assessment, you keep in mind that this patient may be at high risk for:
a. Domestic violence
b. Gestational Diabetes 2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test c. Pregnancy Induced Hypertension
d. Supine Hypotensive Syndrome
20. Which of the following statements is TRUE in regards to pregnancy and motor vehicle crashes?
a. All pregnant patients involved in MVC’s should be backboarded and c-collared no matter the mechanism.
b. Major risk for adverse complications is often due to improper seatbelt use.
c. MVC’s are the leading cause of minor injury in pregnancy.
d. A pregnant patient involved in an MVC with rollover greater than 180 degrees is not a high risk patient for spinal motion restriction and c-collar consideration.
21. You are called to the home of a 36 year old female that dispatch says is 26 weeks pregnant with complaints of not feeling well. Upon arrival she states she has been having a headache for a few days that is similar to her migraines in the past, with nausea and blurry vision. She states that she noticed swelling in her hands and feet and has never experienced blurred vision with past migraines. Her vitals are as follows: 198/104, 100, 22, 99% on RA, 98.2. Reports positive fetal movement and denies any contractions or discomfort in her abdomen. Which of the following treatments/interventions would you choose for this patient?
a. Load her in the ambulance, and get her to the hospital as quickly as possible using lights and sirens
b. Load into the ambulance and perform head to toe assessment, including checking pupils
c. ALS IMC, initiating IV access and administering Versed 2mg q 2 minutes
d. Minimize CNS stimulation, avoid checking pupils, refrain from lights/siren use during transport, seizure precautions 2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test 22. Immediately following delivery of a newborn, all of the following assessments or interventions are crucial EXCEPT:
a. Is the newly born crying/breathing
b. Was the amniotic fluid clear?
c. Suction the nares, then the mouth, using a bulb syringe.
d. Dry, stimulate and provide warmth for newly born using a blanket.
23. TRUE/FALSE - A neonate born with a one minute APGAR score of 5 will require resuscitation, likely for airway, breathing and circulation.
a. True
b. False
24. Which of the following medications/dosing is approved for newly born resuscitation per Region VIII SOPs?
a. Epinephrine 0.1 ml/kg of 1mg/10ml IV/IO for HR < 60
b. Dextrose 2 ml/kg of 25% solution IV/IO for blood sugar less than or equal to 60 with medical control approval
c. Narcan 0.2 mg/kg IV/IO/IN with medical control approval
d. Normal Saline bolus at 20 ml/kg with medical control approval
25. You are called to a restaurant where a family member called for the pregnant patient who’s “water broke” and is having contractions every 2 minutes. Upon your arrival, staff directs you to the restroom where the patient is on the floor with her back up against the wall, hyperventilating and experiencing abdominal pain. She said she went to the restroom as she felt she needed to have a bowel movement but then her water broke while on the commode. She says this is her 3rd pregnancy and she is currently 36 weeks pregnant. She has not had any complications with this or previous pregnancies and carried previous ones to term. Upon exam, the patient’s lungs are clear, 2017 September Region VIII EMS CE Obstetric Emergencies & Neonatal Resuscitation Post-Test she is diaphoretic and you do not note any vaginal bleeding, but you see what appears to be umbilical cord bulging from the vaginal opening. What should you do next? a. Prepare your OB kit and drape the patient for immediate delivery of the fetus. b. Place patient on the cot in Trendelenburg position, insert gloved fingers into the vaginal canal creating gentle pressure against the fetus’s head to lift off the umbilical cord, maintain that position until the patient transfer to hospital staff is complete, cover the exposed cord with moist dressings and keep warm, all while encouraging the patient not to bear down with contractions as well as having your partner notify the hospital with patient information. c. Don gloves and push the umbilical cord back into the vaginal opening, encouraging the patient not to bear down. d. Load the patient in the ambulance and get to the hospital as quickly as possible using lights and sirens, coaching the patient with her breathing techniques.