RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA
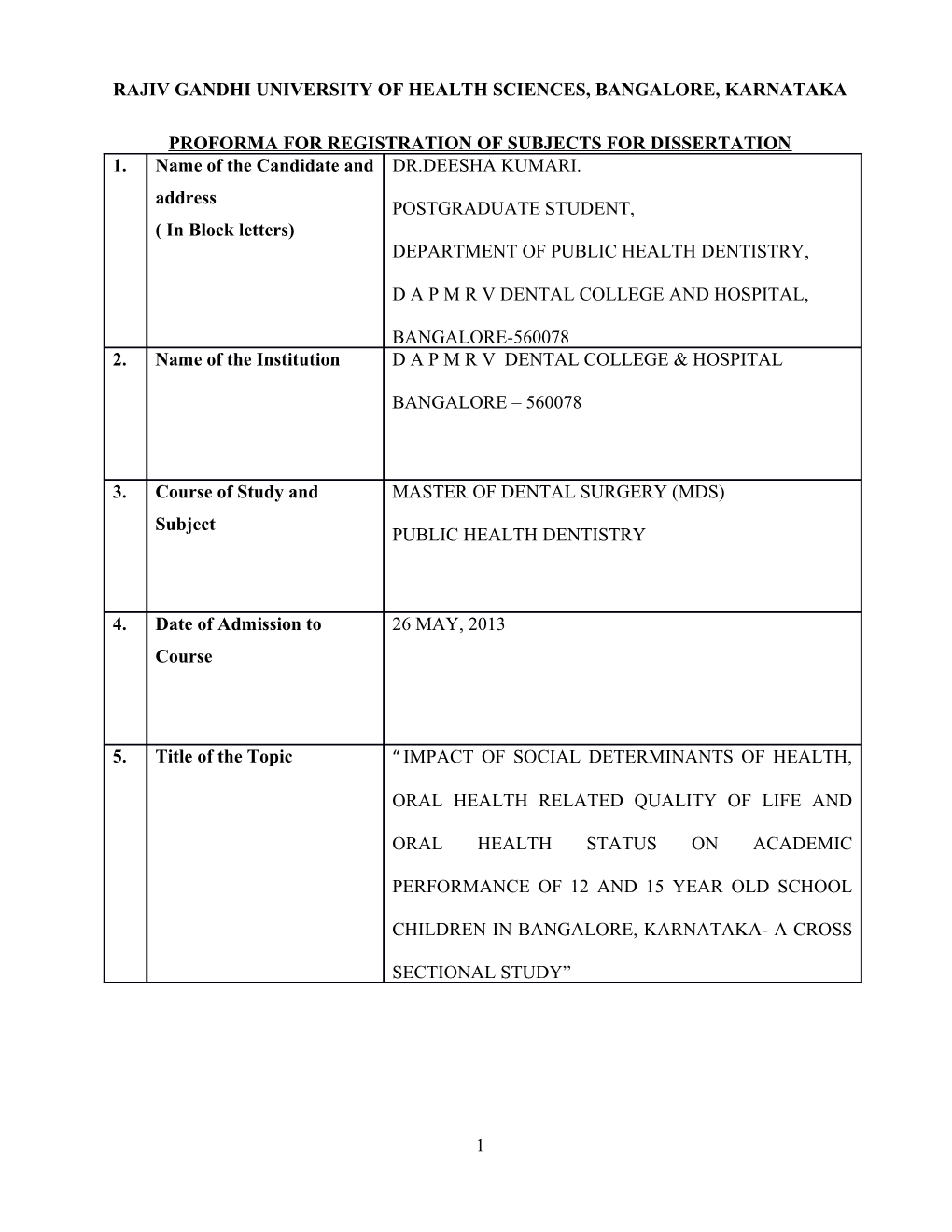
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION 1. Name of the Candidate and DR.DEESHA KUMARI. address POSTGRADUATE STUDENT, ( In Block letters) DEPARTMENT OF PUBLIC HEALTH DENTISTRY,
D A P M R V DENTAL COLLEGE AND HOSPITAL,
BANGALORE-560078 2. Name of the Institution D A P M R V DENTAL COLLEGE & HOSPITAL
BANGALORE – 560078
3. Course of Study and MASTER OF DENTAL SURGERY (MDS) Subject PUBLIC HEALTH DENTISTRY
4. Date of Admission to 26 MAY, 2013 Course
5. Title of the Topic “ IMPACT OF SOCIAL DETERMINANTS OF HEALTH,
ORAL HEALTH RELATED QUALITY OF LIFE AND
ORAL HEALTH STATUS ON ACADEMIC
PERFORMANCE OF 12 AND 15 YEAR OLD SCHOOL
CHILDREN IN BANGALORE, KARNATAKA- A CROSS
SECTIONAL STUDY”
1 TABLE OF CONTENTS 6. BRIEF RESUME OF THE INTENDED WORK………………………………………….1
6.1. Need for the Study………………….………………………………………………….....1
6.2. AIMS AND OBJECTIVES…………………………………………………………...….3
6.2.1. Aims……………………….……………………………………………………………3
6.2.2. Objectives……………………………………………………………………………….3
6.3. REVIEW OF LITERATURE…………………….…………………………………...... 4
7. MATERIALS AND METHOD……………………………………………………………7
7.1. Source of Data……………………………………………………………...…………… 7
7.2. Study Design…………………………………………..…………………………………7
7.3. Sample Size……………………………………….……………………………………. 8
7.4. Sampling Strategy…………………………….……………………………………… . ..8
7.5. Eligibility Criteria………………………………………………………………………..9
7.5.1. Inclusion Criteria………………………………………………………………….…...9
7.5.2. Exclusion Criteria……………………………………………………………….…… 10
7.6. Method of Data Collection………………………………………………………….…..10
7.6.1. Duration of study……………………………………………………………………..10
7.6.2. Data Collection Proforma……………………………………………………………..10
7.7. Data Recording and Statistical Analysis………………………………………………....12
8. REFERENCES……………………………………………………………………………13
9. ANNEXURES…………………………………………………………………………….16
6. BRIEF RESUME OF THE INTENDED WORK:
2 6.1. NEED FOR THE STUDY :
6.1.1. Oral health – an integral part of general health
The mouth is a window into the health of the body. Our oral health has an impact on our overall health, and neglecting one has a negative impact on the other1. The interrelationship between oral and general health is proven by evidence. Many general disease conditions have oral manifestations that increase the risk of oral disease which, in turn, is a risk factor for a number of general health conditions1,2.
6.1.2. Factors influencing oral health
Social disparities in health- and oral health outcomes as measured by social determinants such as place of residence, age, gender, family income, occupation, culture, access to health care systems, education and individual factors in terms of oral health behaviors constitute one of the main challenges for public health. A pattern of poorer health was demonstrated among populations for whom family material resources were distributed less evenly3,4.
6.1.3. Oral disease burden in children and adults
Dental diseases are a significant public health burden in India. A comprehensive National Health
Survey conducted in 2004 in India reported the percent prevalence of dental caries for various age groups examined, for both coronal and root surfaces:51.9% in 5 year-old children ,53.8% in 12 year-old children ,63.1% in 15 year-old teenagers, 80.2% in adults aged 35-44 years-old ,85.0% in adults aged 65-74 years-old5.
6.1.4. Children- oral health related quality of life
Oral diseases restrict activities in school, at work and at home causing millions of school and work
3 hours to be lost each year. The psychosocial impact of these diseases often significantly diminishes quality of life. Children experiencing pain are more likely to be distracted and unable to concentrate on school work. In addition, chewing difficulties due to dental problems often lead to limited choice of foods and poor nutrition with further impact on school performance. Missed school days are likely to be correlated with missed days of work for parents who have to take children for treatment or take care of them at home2.
6.1.5. Health and academics
Childhood chronic conditions have highly variable impacts on children's activities and use of health care. Nationally, 23.4% of children age 6-17 years missed 0 days, 58.4% missed 1-5 days,
12.3% missed 6-10 days and 5.8% missed 11 or more days of school in the past 12 months6.
6.1.6. Oral Health and academics
Poor oral health in children can lead to discomfort and pain which if neglected can cause the
problem to worsen leading to frequent absence and poor performance in schools. Meager
evidence is present in this context. More than 51million school hours are lost annually because
of oral problems6. Children and adolescents’ aged younger than18 years had approximately
5million restricted activity days, more than 1.6million days in bed, and more than 1.7 million
missed school days as a result of acute dental conditions. According to national longitudinal
study conducted by U.S department of education 39.9% children quit school due to failure in
academics7
6.1.7. Need for the study:
Limited research in the western countries has linked the importance of oral health and its impact on academic school performance of children8–11. There is limited infrastructure of the association
4 between oral health, social determinants and OHRQoL and its impact on academic performance in
Indian context where there is huge oral disease burden among school children12. This study will address to close the current gap in knowledge by establishing an association between oral health status, social determinants, OHRQoL and academic school performances. This study may have the following public health policy implications: a. Prove that oral health can be accelerated in all countries through a judicious mix of policy and
institutional reform. b. Strengthen health promoting school strategies in school setting. c. Convince policy makers to inculcate oral health information into the school curricula to make
students aware of the importance of good oral health. d. Provides research agenda to support acceleration toward the Health Millennium Development
Goals
6.2. AIMS AND OBJECTIVES OF THE STUDY:
6.2.1. Aim: The study aims to measure the impact of oral diseases on the academic performance of 12 and 15 year old school children by measuring their oral health status, oral health related quality of life and social determinants in Bangalore, Karnataka
6.2.2. Objectives: a. To assess social determinants affecting health of 12 and 15 year old school children. b. To evaluate the oral health status of 12 -15 yr old school children of Bangalore. c. To assess oral health related quality of life of these school children. d. To collect the secondary data on the academic performance of these children from their
schools e. To explore the association between social determinants of health, OHRQL, oral health status
and their academic performance.
5 6.3. REVIEW OF LITERATURE:
6.3.1. Children's school performance: impact of general and oral health
The study was conducted in North Carolina in 2008 on 2,817 0-17 year old school children which aimed to examine: a) the socio-demographic and health factors associated with poor school performance and b) the impact of poor oral health status on school performance while controlling for other health and socio-demographic factors. Data from the 2005 Child Health Assessment and
Monitoring Program, a follow-back telephone survey to the Behavioral Risk Factor Surveillance
System involving parents/guardians. Bi-variate analysis revealed that sex, race, parental education, low socioeconomic status, poor general health, poor oral health, and the interaction of poor oral health and general health were significantly related to school performance (P < 0.05). Children with both poor oral health and general health were 2.3 times more likely to report poor school performance. Children with either poor oral health or general health were only 1.4 times more likely to report poor school performance. The results showed that children who have both poor oral health and general health are more likely to have poor school performance8.
6.3.2. Influence of children's oral health-related quality of life on school performance and
school absenteeism
A longitudinal study was conducted in Thailand in 2008 on 1,211 9-13 year old Thai school children aiming to co-relate time absent from school due to dental conditions and dental care. It
6 assessed the number of school hours missed for dental reasons per 1,000 grade 5 primary school children in 1 school year and compare dentally related school absences with those related to medical and social reasons. Data on absence were collected from daily school attendance records for 1 year and from children and parents questionnaires and school dental clinic records. Clinical examinations were done. The children (22.5 percent) reported school absence for any dental reason. The mean number of hours of school absence per year for dental care was 434 hours per
1,000 children. Among those who actually missed school for dental reasons, the numbers of hours missed were 1,923 hours per 1,000 children. The study indicated that the level of school absence for dental-related conditions and care was low per child but cumulatively was considerable13.
6.3.3. Oral health and the impact of socio-behavioural factors in a cross sectional survey
A study was conducted in North Carolina, United States of America in 2011 on 2183 school children of 5-11 years old to examine school days missed for routine dental care versus dental pain or infection to determine the relationship between children’s oral health status and school attendance and performance. 2008 data from the North Carolina Child Health Assessment and
Monitoring Program was used. Variables assessed included school absences and performance, oral health status, parental education, health insurance coverage, race, and gender. Children with poor oral health status were nearly 3 times more likely than were their counterparts to miss school as a result of dental pain. Absences caused by pain were associated with poorer school performance
(P<.05), but absences for routine care were not. The study indicated that children with poor oral health status were more likely to experience dental pain, miss school, and perform poorly in school14.
6.3.4. The impact of oral health and socio-demographic determinants on the academic
performance of disadvantaged children
A study was conducted in Los Angeles in 2012 with 1495 children in the age groups of 2 to 5, 6 to
7 8, and 14 to 16 years to represent the 3 stages of dentition to assess the impact of oral health on the academic performance of disadvantaged children by socio-demographic characteristics and access to care determinants. A questionnaire was sent to the parents to collect information about their child’s socio-demographic determinants. Clinical dental examinations were performed .Obtained data was matched with academic achievement and attendance data provided by the school district and linked these to the child’s social determinants of oralhealth and the impact of oral health on the child’s school and the parents’ school or work absences. Students with toothaches were almost 4 times more likely to have a low grade point average. About 11% of students with inaccessible needed dental care missed school compared with 4% of those with access. Per 100 elementary and high school–aged children, 58 and 80 school hours, respectively, were missed annually. Parents averaged 2.5 absent days from work or school per year because of their children’s dental problems.
The study indicated that oral health affects students’ academic performance11.
6.3.5. Time absent from school due to dental conditions and dental care
A study was conducted in Brazil in February 2012 to assess the influence of children's oral health- related quality of life on school performance and school absenteeism. It was a cross-sectional design with a multistage random sample of 312, 12-year-old schoolchildren living in Brazil.
Clinical examinations of the children were conducted and a questionnaire was given to the parents to assess the socio-demographic characteristics. Data on school performance and school absenteeism were obtained from the school register. Multilevel linear regression was used. Low household income (P < 0.05), higher mean of CPQ (P < 0.05), and higher school days missed (P <
0.001) were identified as individual determinants of lower school performance. When the school- level covariates were included in the model, the association between subjects' level characteristics and school performance still persisted. The study indicated that Children's school performance and absence were influenced by psychological and socioeconomic conditions9
8 6.3.6. Association between oral health status and school performance
A cross-sectional study was done in 2009 among 600 primary and nursery school children of
Bangalore city, India to determine the influence of oral health status on academic performance of school children. Oral health status was assessed using df-t index. Academic performance was assessed based on the marks obtained in the previous academic year. The children were divided into 3 groups: excellent, average, below average. Comparison between categorical variables was performed using one-way-Anova using the SPSS software package. The mean df-t of the excellent group was 1.56+2.5, for average group was 2.05+2.8 and for below average group it was 4.47+2.7.
The below average group showed high caries index compared to other groups. The relation between mean df-t and school performance was found to be statistically significant. The study demonstrated that poor oral health has an impact on lowering school performance in children12.
7. Materials and methods
The objective of the study is to assess social determinants, oral health status, oral health related quality of life and to correlate it with the academic achievements and attendance of school children aged 12 and 15 years old of Bangalore, Karnataka.
7.1. Source of Data
Data for the above the above mentioned objective will be obtained from i. School children aged 12 and 15 years old of Bangalore, Karnataka, ii. Their parents and iii. The school authorities.
7.2. Study design: Cross –sectional study design
7.3. Sample size :
9 400 school children aged 12 and 15 year old. Sample size has been estimated based on the formula
Sample Size = Z 2 PQ
2
Z= 1.96 for 95 % Confidence level from Std. Normal Distribution
P = proportion of children with good oral health(0.5 used for sample size needed)
Q= P-1 = proportion of children with bad oral health=1-0.5=0.5
2 (Delta) = 0.05 (5% margin of error)
SS =(1.96) 2x0.5x0.5
(0.05)2
= We get 384, approximating to 400 as the sample size
The above sample size has been estimated by considering that i. Among the school going population in the relevant index age group, 50% of children have
good oral health and 50% children have bad oral health15.
7.4. Sampling strategy: Multi- stage cluster random sampling
Sample size: 400
10 Schools in Bangalore are grouped geographically as study districts into Bangalore North,
Bangalore South & Bangalore Rural.
A study district will be selected by simple random sampling.
Further study district is divided into study zones which are further divided into ranges. From
among these ranges, one range will be selected by simple random sampling.
Total number of wards in this range will be identified and a random selection of wards will be
done. Selection will be done based on the presence of minimum 2 clusters and the included
sector should include high school (each school represents a cluster).
Schools are randomly selected from the total number of schools listed in the area.
Cluster sampling is done and school children aged 12 and 15 years old are randomly selected.
Schools will be sent a letter from the Department of Education explaining the study and
inviting participation.
7.5. Eligibility criteria:
7.5.1. Inclusion criteria:
1. Children in the age group of 12 and 15 years
2. Children who are willing to participate
3. Children with parental consent
7.5.2. Exclusion criteria:
1. Children with mental and physical disability16
2. Children absent on the date of examination.
7.6. Method of collection of data
11 7.6.1. Duration of study: 1 year
7.6.2. Data collection Proforma:
Relevant annexures attached will be suitably modified and validated before its use in the study. a)Questionnaire for assessing the social determinants of health (Annexure 3)
b) Proforma for assessing oral health status- will include indices to record dentition status and
periodontal health (Annexure 4) c) Proforma to record oral health related quality of life (Annexure 5).
d) Proforma to collect academic achievements and attendance (Annexure 6)
7.6.3. Method of data collection:
The process of data collection will include the following a)Written permission will be obtained from the Department of education, and individual school
administration. b) Informed consent will be obtained from the school children, their parents and their teachers.
c) Ethical clearance obtained from the Institutional Review board.
12 d) A self structured questionnaire to assess social determinants will be handed over to these
children’s parents. e) Clinical examination will be performed to assess the oral health status of children.
f) Questionnaire will be administered to these children to assess their oral health related quality
of life. g)Updated attendance and academic performance of these children till the date of clinical examination will be obtained from the school authorities.
Study will be done in the following phases The study will be done in the following phases
Phase Plan of work Duration Phase 1 Development and validation of questionnaires to be used in the 2-3 months research Phase 2 Pilot testing of the Proforma 1 month Training and calibration of investigators Phase 3 Data collection 6 months Phase 4 Data analysis 3months
1)Phase 1: Development and validation of questionnaires to be used in the research:
Questionnaires will be developed based on review of literature. The developed questionnaires will
be evaluated for face validity, content validity and criterion validity. The questionnaires will be
developed to explore the i. Social determinants of health ii. Oral health related quality of life and an
13 iii. Oral health assessment form.
2)Phase 2: Pilot testing of the Proforma, Training and calibration of investigators:
The questionnaires developed will be validated and pilot tested prior to the actual implementation
in the field.
The investigator will involve a team of 2-4 house surgeons from the same college and will be
trained and calibrated to assist in data collection process.
3)Phase 3: Data collection: a. A questionnaire to explore the social determinants will be handed over to the children’s
parents. b. Oral health status of these children will be determined by clinical examination and oral health
assessment form. c. A self structured questionnaire to assess the oral health related quality of life will be
administered to the children d. Data regarding students’ academic achievements and attendance will be collected from the
school authorities.
4)Phase 4: Data analysis:
After examining descriptive statistics, statistical analysis will be done to test the relationship
between oral health status, oral health related quality of life, social determinants and academic
14 performance and attendance of school children.
7.6.4. DATA RECORDING AND STATISTICAL ANALYSIS:
The data will be analysed using Statistical Package for Social Sciences (version 18)
Descriptive statistics will be expressed in terms of percentage and frequency.
Inferential statistics will be dealt using Chi square test, co-relation and regression models and
any other relevant statistical tests.
7.7. Does the study need any intervention do be conducted on the patients or other humans or
animals? If so, please describe briefly.
Yes, the study requires administration of questionnaires regarding OHRQoL, social determinants and academic achievements of children to school children, their parents and school authorities respectively followed by clinical examination to record their oral health status
7.8. Has the ethical clearance been obtained from your institution in case of the above?
Yes, Ethical clearance obtained
8. References
1. Health NI of. Chapter 1: The Meaning of Oral Health [Internet]. [cited 2013 Oct 22]. Available from: http://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/sgr/chap1.htm
2. WHO | Oral health, general health and quality of life [Internet]. WHO. [cited 2013 Oct 22]. Available from: http://www.who.int/bulletin/volumes/83/9/editorial30905html/en/
3. Mashoto KO, Astrom AN, Skeie MS, Masalu JR. Socio-demographic disparity in oral health among the poor: a cross sectional study of early adolescents in Kilwa district, Tanzania. BMC Oral Health. 2010 Apr 20;10(1):7.
4. Finlayson T. evidence base for social determinants and oral health promotion. Available from: http://www.nationaloralhealthconference.com/docs/presentations/2005/0504/evidencebasefors ocialdeterminants.PDF
5. 661.pdf [Internet]. [cited 2013 Oct 22]. Available from: http://www.who.int/bulletin/volumes/83/9/661.pdf
15 6. NHIS - National Health Interview Survey Homepage [Internet]. [cited 2013 Oct 22]. Available from: http://www.cdc.gov/nchs/nhis.htm
7. causeshsdropout.doc [Internet]. [cited 2013 Oct 22]. Available from: http://www.gafcp.org/sys_gafcp/publications/BestPractices/causeshsdropout.doc
8. Blumenshine SL, Vann WF Jr, Gizlice Z, Lee JY. Children’s school performance: impact of general and oral health. J Public Health Dent. 2008;68(2):82–7.
9. Piovesan C, Antunes JLF, Mendes FM, Guedes RS, Ardenghi TM. Influence of children’s oral health-related quality of life on school performance and school absenteeism. J Public Health Dent. 2012;72(2):156–63.
10. Jürgensen N, Petersen PE. Oral health and the impact of socio-behavioural factors in a cross sectional survey of 12-year old school children in Laos. BMC Oral Health. 2009;9:29.
11. Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012 Sep;102(9):1729–34.
12. Garg N, Anandakrishna L. Is there association between oral health status and school performance? a preliminary study. international journal of clinical dentistry. 2012 Aug;5(2):132–5.
13. Pongpichit B, Sheiham A, Pikhart H, Tsakos G. Time absent from school due to dental conditions and dental care in Thai schoolchildren. J Public Health Dent. 2008;68(2):76–81.
14. Jackson SL, Vann WF, Kotch JB, Pahel BT, Lee JY. Impact of Poor Oral Health on Children’s School Attendance and Performance. Am J Public Health. 2011 Oct;101(10):1900–6.
15. Health NI of. Dental Caries (Tooth Decay) in Adolescents (Age 12 to 19) [Internet]. [cited 2013 Oct 30]. Available from: http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/DentalCaries/DentalCariesAdolesce nts12to19
16. Children with Special Health Care Needs A Profile of Key Issues in California [Internet]. California: The Child and Adolescent Health Measurement Initiative; 2010 Nov. Available from: www.Ipfch.org/specialneeds
17. Cole BL, Fielding JE. Health Impact Assessment: A Tool to Help Policy Makers Understand Health Beyond Health Care. Annual Review of Public Health. 2007 Apr;28(1):393–412.
18. WHO | The determinants of health [Internet]. WHO. [cited 2013 Oct 29]. Available from: http://www.who.int/hia/evidence/doh/en/index2.html
19. Yusuf H, Gherunpong S, Sheiham A, Tsakos G. Validation of an English version of the Child- OIDP index, an oral health-related quality of life measure for children. Health and Quality of Life Outcomes. 2006 Jul 1;4(1):38.
16 9. Signature of the Candidate
10. Remarks of the Guide
11. Name and designation of DR.A G HARIKIRAN, Guide PROFESSOR AND HEAD, (in block letters) DEPARTMENT OF PUBLIC HEALTH DENTISTRY, D A P M R V DENTAL COLLEGE AND HOSPITAL. BANGALORE 11.2 Signature of the Guide
11.3Name and designation of ------Co-Guide (in block letters) ---
11.4Signature of the Co------guide ---
11.5 Head of Department DR.A G HARIKIRAN, PROFESSOR AND HEAD, DEPARTMENT OF PUBLIC HEALTH DENTISTRY, D A P M R V DENTAL 17 COLLEGE AND HOSPITAL. BANGALORE
11.6 Signature of Head of the department 12. 12.1 Remarks of the Chairman and Principal
12.2 Signature of the Chairman and Principal
18