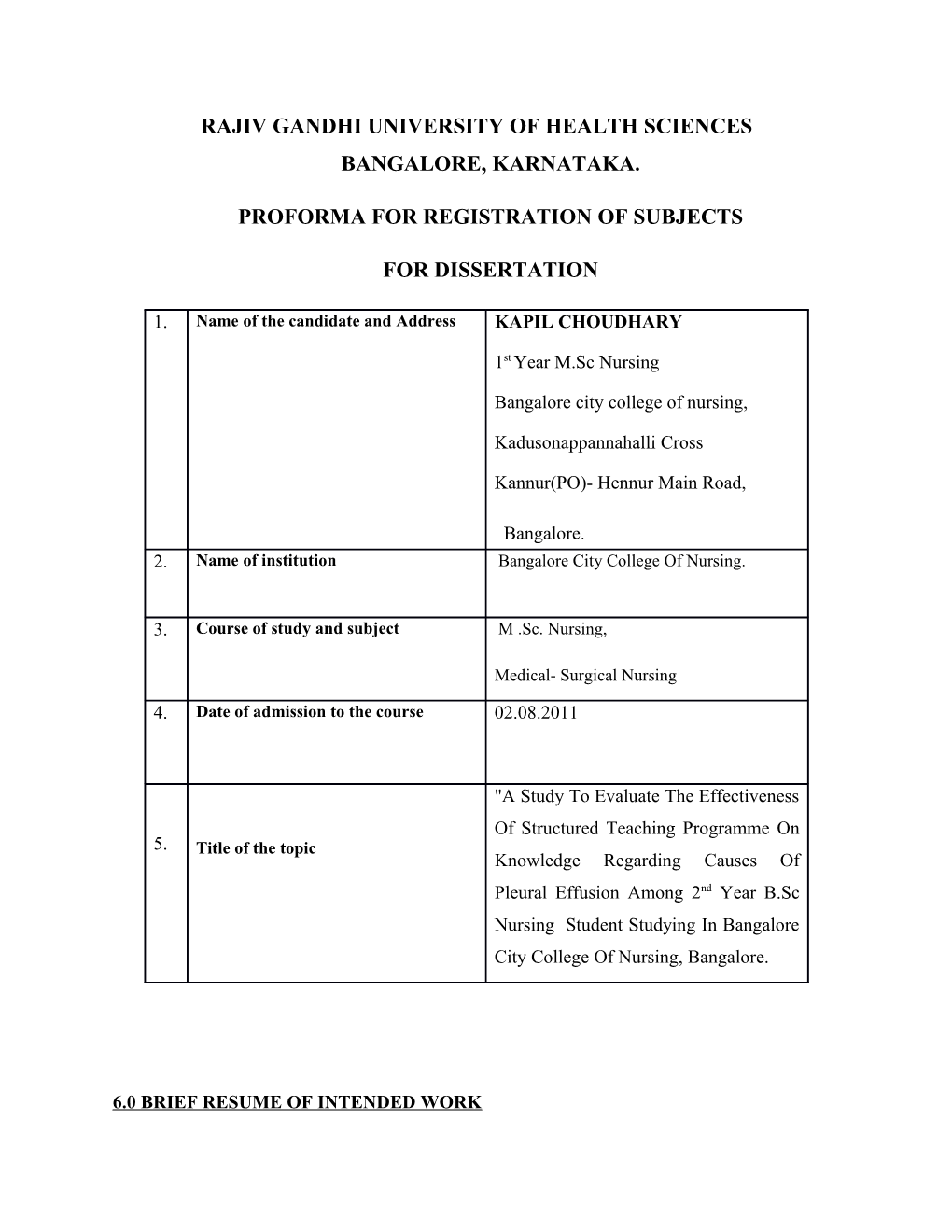
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE, KARNATAKA.
PROFORMA FOR REGISTRATION OF SUBJECTS
FOR DISSERTATION
1. Name of the candidate and Address KAPIL CHOUDHARY
1st Year M.Sc Nursing
Bangalore city college of nursing,
Kadusonappannahalli Cross
Kannur(PO)- Hennur Main Road,
Bangalore. 2. Name of institution Bangalore City College Of Nursing.
3. Course of study and subject M .Sc. Nursing,
Medical- Surgical Nursing
4. Date of admission to the course 02.08.2011
"A Study To Evaluate The Effectiveness Of Structured Teaching Programme On 5. Title of the topic Knowledge Regarding Causes Of Pleural Effusion Among 2nd Year B.Sc Nursing Student Studying In Bangalore City College Of Nursing, Bangalore.
6.0 BRIEF RESUME OF INTENDED WORK INTRODUCTION :-
"Pleural Effusion is an abnormal accumulation of fluid in the intra pleural spaces of the lungs. It is characterized by chest pain, dyspnea, adventitious lung sounds, and non productive cough."1
Pleural effusion, a collection of fluid in the pleural space, is rarely a primary disease process but is usually secondary to other diseases. Normally, the pleural space contains a small amount of fluid (5 to 15ml), which acts as lubricant that allows the pleural surfaces to move without friction. Pleural effusion may be a complication of heart failure, TB, pneumonia, pulmonary infections (particularly viral infections) nephrotic syndrome, connective tissue disease, pulmonary embolism and neoplastic tumors. Bronchogenic carcinoma is the most common malignancy associated with a pleural effusion.2
Normally 150ml fluid is produced in pleural space in 24 hrs at the rate of 0.1ml/kg 1hr.
More than 90-95% of the fluid is reabsorbed only 10-15ml fluid is left in pleural space; pleural fluid has a protein concentration of 1.06-1.30 grams per 100ml with 57-78% of albumin.3
Increased entry of fluid versus decreased exit of fluid. Increased fluid entry due to increased permeability (increased in fluid conductance or protein permeability), increased micro vascular pressure (usually increased venous outflow pressure arterial pressures usually not transmitted due to capillary resistance. Thought to be lungs interstitial fluid when hydrostatic pressure), decreased pleural pressure (significant at atelectasis reduces pressures around nearby vessels), decreased plasma oncotic pressure (hypoabluminemia alone not usually enough but can lower threshold for other factors). Decreased fluid exit due to reflects a reduction in lymphatic function, much of how is speculative, there are intrinsic and extrinsic factors. Intrinsic [prevent ability of lymphatic vessels to transport fluid product of inflammations endocrine problems
(Hypothyroidism), direct injury (chemotherapy, radiotherapy), infiltration with cancer]. Extrinsic
[Limitation of respiratory motion diaphragm paralysis, lung collapse), compressions of lymphatic’s (pleural malignancy) increased systemic venous pressure (only acutely because chronically lymphatic’s can adopt.), decreased liquid availability (after pneumothorax liquid contacts fewer lymphatic opening] common postoperative in patients undergoing cardiac surgical procedures, predominantly left sided: suggests underlying pericarditis is a causative factor.
Majority are small and not serious. Pathogenesis may relate to immunologic cause (respond to steroids and prolonged latent period from injury to onset).4
Pleural effusion is a common clinical finding with many potential causes. The first step in the evaluation of a pleural effusion is to determine whether the pleural fluid is a transudate or an exudate. The formation of a transudate usually result's from increased capillary hydrostatic pressure or from decreased colloid osmotic pressure. The main cause of transudates is usually congestive heart failure (CHF). The formation of an exudate usually results from an increased permeability of the micro vascular circulation, generally due to inflammatory or neoplastic processes.5
The two main tasks are involved in approaching the patient with pleural effusion. First, document the presence and size of the effusion, using history, physical examination and radiologic studies. Second determine the cause of the effusion.6
Light's criteria were used to distinguish exudates from transudates. Pleural effusion is the most common manifestation of disorders of the pleura. After routine and radiological investigation's, the diagnostic work up of patient with clinically significant. Pleural effusion usually begins with a thoracentesis.7 6.1 NEED FOR STUDY:-
Approximately, 1 million pleural effusion cases are diagnosed each year in India, the clinical importance of pleural effusions ranges from incidental manifestation of cardiopulmonary disease to symptomatic, inflammatory as malignant disease that require urgent evaluation and treatment.8
Pleural effusion affects more than 1.3 million people annually. Pleural effusion is a common diagnostic problem. It has got diverse etiologies, depending upon the age, sex, and socioeconomic background of the patient.9
Tuberculosis is a common cause of pleural effusion in India. Recent studies of population with a high prevalence of tuberculosis report that tuberculosis pleural effusion occurs in approximately 30% of patients with tuberculosis.10
Pleural effusion in MICU patients is common and most are detected by careful review of chest radiographs taken with the patient in erect or semi erect position. When clinical suspicion for infection is low, observation of these effusions is warranted initially, because most are caused by noninfectious processes that should improve with treatment of the underlying disease.11
Pleural effusion (PE) can occur as a complication of various diseases. The appropriate approach to a patient with pleural effusion requires knowledge of its incidence and prevalence.
The epidemiology of pleural effusion can be studied using different methods and approaches.
The annual incidence of pleural effusion and its types can be investigated in unselected population in a particular geographical area. Very limited information of the incidence of pleural effusion in a general unselected population is available. The etiological distribution of pleural effusion depends on the geographical region, the age of population and advances in the diagnosis and treatment of underlying causes.12
Primary pneumothorax remains a significant global problem occurring in healthy subjects with a reported incidence of 18.28/10,000 per year for man and 1.2 to 6/10,000 per year for women. However, pneumothorax seems to occur most often in males 25-40 years of age.8
Malignant pleural effusion is a common clinical manifestation of all type of lymphomas, but the exact frequency of pleural effusion varies. Most author estimate that 20-30% of patient with malignant lymphoma have either a pleural effusion or ascites during the clinical course of their disease. 13 6.2 REVIEW OF LITRATURE:
A study demonstrates that when the entire population is surveyed, PE is relatively common. There have only been a few studies on the incidence of PE in the general in the population. A study that covered all or nearly all the population in a particular geographical region was carried out in the Czech Republic 30 years ago. It is interesting to compare the results published in 1993 with the data published in 1962. At that time the most common cause of effusion was TB pleurisy. Which accounted for 146 of 400 (36.5%) patients sampled in the 4 yr period b/w 1956-60 in the Eastern Bohemian region? The second and third most common cause was malignant PE and infectious effusions (parapneumonic and empyema) both with 17%. The fourth most common cause was a transudate accompanying CHF (15%) followed by paraembolic effusion (4.5%) other causes of PE did not exceed 4%.14
In a study carried out in South Africa in 1993 Among 555 patients. The following types of PE were found. TB was the most common cause (27%) followed by infectious disease (23%),
CHF (18%) and malignant diseases (17%). The proportions of various types of effusion differed according to race and age. In the causation and African groups TB accounted for 27% and 49% respectively Infectious and Malignant diseases were the next most frequently observed causes. In
Caucasians, CHF accounted for 31%, followed by infectious conditions 23% and malignant disease (20%). T.B. accounted for 4%. These figures are similar to data from the USA and
Europe. 15
In a study from the kawaskai medical school in Okayama. Japan, 125 cases of PE admitted between 1985-1989 was analysed. The PE were caused by Carcinomatous pleurisy in
47 cases (37%), non TB infection in 34 cases (27%), TB pleurisy in 17 cases (14%), cardiac insufficiency in 11 cases, trauma and pneumothorax in nine cases, Collagen vascular disease in two cases and was of an unknown origin in five cases. 16
The prevalence and causes of PE in the medical intensive care unit (ICU) setting are shown in the study from the Medical University of South Carolina, Charleston, USA. In 100 ICU patients the PE prevalence was 62%, 41% of effusions were detected at the time of admission.
Fifty seven of 62 (92%) PE was small. The following were the cause of PE: CHF 35%, atelectasis 23%, uncomplicated parapneumonic effusion 11%, hepatic hydrothorax 8%, hypoalbuminaemia 8%, malignancy 3% and unknown 5%. 17
In a study from the City Hospital Centre in Elmhurst, 82 patients with acute pancreatitis were admitted during a 4year period. Eleven (13.4%) of them had an evidence of PE. Eight of 42 patients with alcoholic pancreatitis developed an effusion, compared with one of 33 Patients with biliary pancreatitis. These data suggest that alcoholic etiology could be a risk factor for PE. 18
In a study performed at the University of Western Ontario (London, Canada), PE was identified in 7% (four of 58) of the cohort of scleroderma patients and were more frequent in diffuse disease 10%. 19
A study was conducted in Foundation Hospital Alcorcon, Madrid Spain. To determine whether the incidence of pleural effusion secondary to pneumonia has increased in hospitalized patients. Patients aged less than 16 years old admitted to our hospital with a diagnosis of pneumonia between 1999 and 2005 were retrospectively reviewed. A total of 337 patients were analyzed of which 213 (63.2%) met the criteria for a diagnosis of probable bacterial pneumonia.
Pleural effusion was found in 34 patients (15.9%), and 13 of these effusions (38%) were complicated. No clear trend was detected in the annual incidence of probable bacterial pneumonia per 100 admitted patients, although the highest numbers were detected in the last two year of the study period. The percentage of complications (effusions) remained constant (mean:
16.28%). No difference were found in the effusion rate between vaccinated and unvaccinated patients (12.5 vs 18.6%). 20
On 113 cases of this entity in the Japanese literature and reviewed. The most common
(99%) underlying cause of this entity was chronic alcoholic pancreatitis in most cases the patients complained of chest symptoms (68%), and complained of abdominal symptoms lies frequently (24%). It is important to maintain suspicion for this entity in patients with chronic alcoholic pancreatitis who have unexplained pleural effusion.21
A retrospective study was performed on consecutive patients with exudative pleural effusion seen in University of Malaya Medical Center, Kuala Lumpur, Malaysia during a 4-year period. Of 186 patients with a mean age (+/- SD) of 51.2 (+/- 19.2) years with exudative pleural effusions, 131(70.4%) were males and 55(29.6%) were females. The most frequent cause of exudative pleural effusions was tuberculosis (44.1%), followed by malignancy (29.6%). The majority (94.5%) of malignant pleural effusion were due to lung cancer. Tuberculosis effusions were most frequent in the first five decades (60/82, 73.2%) and were the most common type of pleural effusion, accounting for 60 (69.8%) of 86 cases, In this age rang. Malignant effusions were more frequent among the older age groups, 74.5% (41/55) of patients with malignant effusion being older than 50 years. Most types of pleural effusion showed a preference for the right side. Of the 44 cases of large effusions, 28 (63.6%) were caused by malignancy. In our region with a high incidence of tuberculosis, the most frequent cause of pleural exudates in tuberculosis followed by malignancy particularly lung cancer.22 This study was conducted to assess the prevalence of eosinophilia in 358 consecutive samples of pleural fluid (all cases corresponded to first thoracentesis), to review the cause of eosinophilic pleural effusions and to determine whether the presence of eosinophils increases the likelihood of nonmalignant underlying disorders. Eosinophilic pleural effusions were identified in 45 patients (12.6%): malignant underlying conditions were diagnosed in 11 Patients (24.4% with eosinophilic effusions) and benign etiologies were found in 27 patients. Benign etiologies included uncomplicated paraneumonic effusion in 10 patients, tuberculosis in seven, complicated paraneumonic in five, liver cirrhosis in three, hydronephrosis in one and pulmonary thromboembolism in one. Seven pleural effusions were idiopathic.23 6.3 STATEMENT OF THE PROBLEM:
"A study to evaluate the effectiveness of structured teaching programme on knowledge regarding causes of pleural effusion among 2nd year B.Sc nursing students studying in Bangalore city college of nursing, Bangalore."
6.4 OBJECTIVES OF THE STUDY:
1. To assess the knowledge on causes of pleural effusion among 2nd year B.Sc nursing students
2. To assess the effectiveness of structured teaching programme on cause of pleural effusion
among 2nd year B.Sc nursing students.
3. To find out the association between knowledge scores of 2nd year B.Sc nursing students with
selected socio-demographic variables.
6.5 HYPOTHESIS:
H1 There will be a significant improvement in post-test knowledge scores compared to the pre-
test knowledge scores regarding causes for pleural effusion among 2nd year B.Sc nursing
students.
H2 There will be a significant association between knowledge scores with their selected socio-
demographic variables.
6.6 OPERATIONAL DEFINITION :
Evaluate: - It refers to analyze the effectiveness of structured teaching programme regarding causes of pleural effusion.
Effectiveness:- Refers to gain in knowledge as determined by the significant difference between pre-test and post test knowledge scores. Structured Teaching programmed:- It is systematically developed information and teaching aid, design for B.Sc nursing 2nd year Student to provide information about various causes of plural effusion at Bangalore city college of Nursing in Bangalore.
Knowledge: - It refers to awareness of patient regarding pleural effusion causes which is measured by structured questionnaire schedule.
Pleural effusion: - An abnormal accumulation of fluid in the intrapleural space of the lungs.
B.Sc Nursing Student: - A person who studying in degree course of the Nursing.
6.7 ASSUMPTION
1. B.Sc nursing 2nd year Students have inadequate knowledge regarding causes of pleural
effusion.
2. Structured teaching programme may improve the knowledge of the B.Sc nursing 2nd Year
student regarding causes of pleural effusion.
3. B.Sc.Nursing 2nd Year Student Knowledge may vary with the selected demographic
variables regarding causes of pleural effusion.
6.8 DELIMITATION OF THE STUDY
1. Prescribed data collection period is only 2-4 weeks.
2. Study is limited to 60 Students.
3. Study is delimited to B.Sc nursing 2nd year student only at Bangalore city
college of Nursing in Bangalore. 6.9 PROJECT OUT COME
The project will help to find out that how extent the B.Sc Nursing (2nd Year) student gain the knowledge about causes of pleural effusion at Bangalore city collage of nursing, Bangalore.
7.0 MATERIAL AND METHODS
7.1 SOURCE OF DATA:
The data will be collected from the B.Sc Nursing (2nd year) Students at Bangalore city collage of Nursing, Bangalore.
7.1.1 RESEARCH DESIGN:
As the researcher intended to assess the knowledge regarding causes of pleural effusion among B.Sc Nursing(2nd Year) Students, the questionnaire pre experimental design, one group pre and post test design will be used.
7.1.2 SETTING:
The Bangalore city collage of Nursing, Bangalore.
7.1.3 POPULATION:
Only 60 Students of B.Sc nursing 2nd year at the Bangalore city collage of Nursing,
Bangalore.
7.2 METHOD'S OF DATA COLLECTION:
Sample Size : 60 Students
Sample Technique : Simple Random Sampling
Duration of Study : 4 Week
7.3 INCLUSION AND EXCLUSION CRITERIA:
A. INCLUSION CRITERIA: B.Sc nursing 2nd Year Students who are willing to participate in the study and present at the time of data collection.
B. EXCLUSION CRITERIA :
B.Sc nursing 2nd Year Students who are not present at the time of data collection.
7.4 TOOL OF THE RESEARCH:
Structured questionnaire will be constructed into two parts:
A. Part A – Demographic Data
B. Part B – Knowledge questionnaire regarding causes of pleural effusion.
7.5 COLLECTION OF DATA:
After obtaining informed written consent from the participants, the investigator will collect date by using structured questionnaire to assess the knowledge before and after structure teaching programme.
PART – I
Deal with demographic characteristic of the B.Sc 2nd year students of Nursing.
PART – II
Structured knowledge questionnaire which consist of questions related to general information and causes of the pleural effusion. The score of one will be given for correct response and score of zero will be given for wrong response, the resulting score will be ranged as follows:
High Knowledge Score - 16-20 (76-100%)
Average Knowledge Score - 11-15 (51-75%) Low Knowledge Score - 1-10 (01-50%)
PLAN FOR DATA ANALYSIS:
The data collected will be analyzed by means fo descriptive and inferential statistics.
Descriptive Statistics is analyzed by mean, percentage distribution, and standard deviation. The comparison between knowledge and demographic variables will be analyzed by chi square and paired "T" test for correlation.
7.6 DOES THE STUDY REQUIRE ANY INVESTIGATION OR INTERVENTIONS TO
BE CONDUCTED ON PATIENTS OR OTHER HUMANS OR ANIMALS? IT SO
PLEASE DESCRIBE BRIEFLY.
yes, the Study will be conducted on B.Sc nursing 2nd Year students with causes of pleural effusion using structured teaching programme.
7.7 HAS ETHICAL CLEARANCE BEEN OBTAINED FROM YOUR INSTITUTION
CASE OF 7.3?
Yes, ethical clearance has been obtained from the concerned authority of institution.
Informed written consent will be obtained from the participants prior to the study.
Privacy, confidentiality and anonymity will be guarded.
Scientific objectivity of the study will be maintained with honesty and impartiality. 8.8 BIBLOGRAPHY:-
1. Mosby's pocket dictionary of medicine, Nursing Health professions, 5th edition, 2007.
P.1074.
2. SuzanneC. Smeltzer, Brenda G, Bare test book of medical surgical Nursing(Brunner &
Suddarth's) Editionh – 10th, 2004, 540, 541.
3. Marcel Dekker, The pleura in health and disease new York, 2010, 195-231.
4. C. Michael Gibson, m.s,. m.d website address:- "http://wikidoc.org/index.php?
title=plearal effusion pathophy siology + oldid = 601431."
5. Yigal Abramowitz, pleural effusion: characterization with ct attenuation values and CT
appearance, American journal of Roetgenology march 2009, vol – 192, 618-623.
6. stagner sw, compbell G.D. Pleural Effusion: What can you learn from the results at the a
"Top"? Postgrad med 2006; 91: 439-454.
7. Light Rw. 4th ed. Lippincort Williams and wilkings: 2008. Approach to the patient. In
pleural disease PP 42- 86.
8. Davies CWH, Gleeson FV, Davies RJO. BTS Guidelines. Management of pleural
infection. British medical Journal 2003; 58 (18) : 18-20
9. Kirasewitz GT, Fisherman AP, Influence of alteration in starling torces on visceral fluid
movement: a Appl Physiol (51), 617-677. 10. Bansal panky, department of medicine, sharda university greater noida, "tuberculosis
pleural effusion", Indian journal of medical science and research year 2010, volume -1,
issue – 2, print issn – 0976-5948.
11. Lalaine E-Mattison, Pleural effusion in medical ICU, April 1997 Vol.III, No-4, 1018-
1023.
12. Marel M. Zrustova m, stastny B, Light RW. The incidence of pleural effusion in a well-
defined region. Epidemiologic study in central Bahemia, chest 2004, 104: 1486-1489.
13. Seitzer D. Musche, Kuhn W. Local Treatment of malignant pleural effusion in
gynecologic tumors, zentralbl gynakol 2005, 112: 567-576.
14. Storey DD. Dines DE, Coles DT. Pleural effusion: a diagnostic dilemma, Jama 2007;
236; 2183-2186.
15. Burges LJ, Maritz FJ, Taljaard JJ. Epidemiology of pleural Effusion (Letter)/ S sfr Med J
2008, 86; 186.
16. Kimura M, Nakamura J, Tomizawa S, Adachi M., Tano Y, Matsushima T, The role of
thoracoscopy in pleural biopsy in cases with pleural effusion, nihon-kyobu-shikkan-
Gakkai-Zasshi 2009;28:882-888.
17. Mattison LE, Coppagel, Alderman DF, Herlong JO, Sahn SA. Pleural effusions in the
medical ICU: Prevalance, causes and clinical implications. Chest 20010:111:1018-1023.
18. Gumaste V, Singh V, dave P, Significance of Pleural effusion in patients with acute
pancreatitis. AMJ Gastroenterol 2011: 87: 871-874. 19. Thompson AE, Pope JE, A Study of the frequency of pericardial and pleural effusion in
scleroderma. Br. J. Rheumatol 2012; 37: 1320-1323
20. Bveno Campana M, Agunder Reigosa B, Jimeno Roiz S, Echavarri olavarria F, Martinez
Granero MA. "is the incidence of paraneumonic pleural effusion increasing? Feb 2008;
68 (2): 92-98.
21. Uchiyama T, Suzuki T, Adachi A, Hiraki S, Lizuka N, Second department of rugerym
yamaguchi university school of medicin, japan. "Pancreatic pleural effusion: case report
and review of 113 cases in japan, Mar 2005; 87 (3) : 387-91.
22. Liam CK, Lim KH, Wong KM, Department of medicine, university of Malaya medical
centre, kula lumpur, Malaysia. Causes of pleural exudates in a region with a high
incidence of tuberculosis. Mar 2005(1):33-38.
23. Martizer- Garcia, Cases-Viedma E, Cordero – Rodrigure PJ, Hidalgo – Ramirez M,
Perpina-Tordera M, Sanchis-Moret F, Sanchis-Aldar JL; Diagnostic utility of eosinophils
in the pleural fluid. 2000; 15(1):166
24. www.pubmed.gov
25. www.google.com 9 SIGNATURE OF CANDIDATE
10 REMARKS OF THE GUIDE RECOMENDED
11 NAME AND DESIGNATION
11 .1 GUIDE Mrs. SUDHA. S
11.2 SIGNATURE
11.3 CO –GUIDE
11.4 SIGNATURE 11. 5 HEAD OF THE DEPARTMENT Mrs. SUDHA. S
11. 6 SIGNATURE
12 12.1 REMARKS OF THE CHAIRMAN/ PRINCIPAL
12 .2 SIGNATURE