PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY/ PROCEDURE
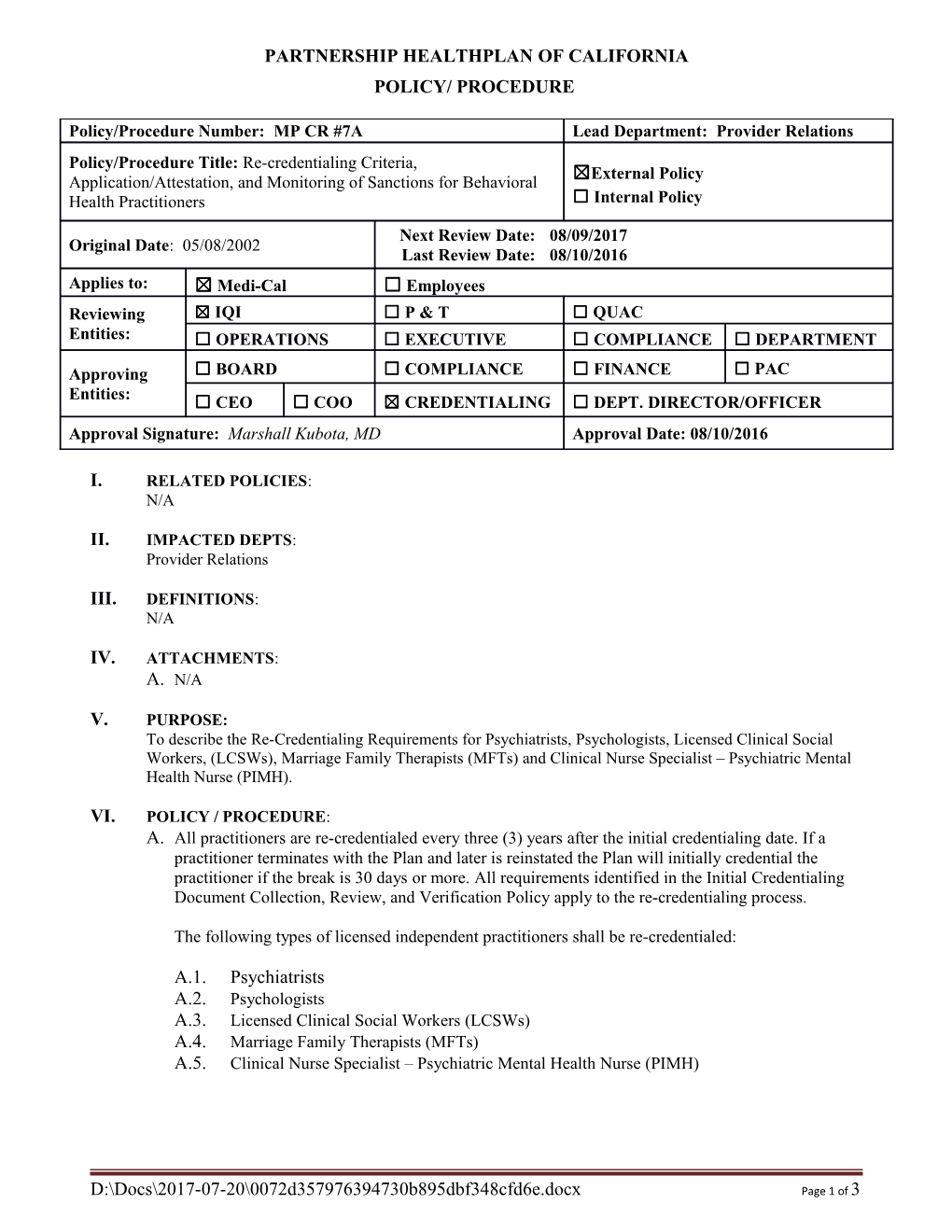
Policy/Procedure Number: MP CR #7A Lead Department: Provider Relations Policy/Procedure Title: Re-credentialing Criteria, ☒External Policy Application/Attestation, and Monitoring of Sanctions for Behavioral Health Practitioners ☐ Internal Policy Next Review Date: 08/09/2017 Original Date: 05/08/2002 Last Review Date: 08/10/2016 Applies to: ☒ Medi-Cal ☐ Employees Reviewing ☒ IQI ☐ P & T ☐ QUAC Entities: ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT
Approving ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☐ PAC Entities: ☐ CEO ☐ COO ☒ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER Approval Signature: Marshall Kubota, MD Approval Date: 08/10/2016
I. RELATED POLICIES: N/A
II. IMPACTED DEPTS: Provider Relations
III. DEFINITIONS: N/A
IV. ATTACHMENTS: A. N/A
V. PURPOSE: To describe the Re-Credentialing Requirements for Psychiatrists, Psychologists, Licensed Clinical Social Workers, (LCSWs), Marriage Family Therapists (MFTs) and Clinical Nurse Specialist – Psychiatric Mental Health Nurse (PIMH).
VI. POLICY / PROCEDURE: A. All practitioners are re-credentialed every three (3) years after the initial credentialing date. If a practitioner terminates with the Plan and later is reinstated the Plan will initially credential the practitioner if the break is 30 days or more. All requirements identified in the Initial Credentialing Document Collection, Review, and Verification Policy apply to the re-credentialing process.
The following types of licensed independent practitioners shall be re-credentialed:
A.1. Psychiatrists A.2. Psychologists A.3. Licensed Clinical Social Workers (LCSWs) A.4. Marriage Family Therapists (MFTs) A.5. Clinical Nurse Specialist – Psychiatric Mental Health Nurse (PIMH)
D:\Docs\2017-07-20\0072d357976394730b895dbf348cfd6e.docx Page 1 of 3 B. In addition to the re-credentialing requirements, relevant information regarding performance monitoring which includes: Quality Improvement Activities, Peer Review, and member complaints shall be part of the re-credentialing process for high volume practitioners. Site Reviews are not required for re-credentialing, however, if a site review is done, the procedure of the office site audits are described in the re-credentialing process for high volume practitioners as defined in the Initial Credentialing Site Review Policy.
C. All verification of documentation and information required may not be more than 180 days old at the time of Credentialing Committee decision.
D. Review issues identified during the re-credentialing process as defined in the Review Standards for Credentials, Re-credential Process, Policy MP CR #5.
E. Practitioners have the right to review any portion of their personal re-credentialing file related to information submitted in support of their re-credentialing application. Practitioners also have the right to correct any identified erroneous information.
F. Credentialing Committee shall review and evaluate the re-credentialing application and supporting documentation to determine if the practitioner meets the re-credentialing criteria.
G. If the Credentialing Committee does not approve a practitioner for re-credentialing, the practitioner will be notified of the decision in writing within ten (10) business days.
H. The practitioner may appeal the decision using the process as identified in the Fair Hearing Process for Adverse Decisions.
I. If a practitioner’s re-credentialing profile is denied based upon deficiencies in the practitioner’s professional competence, conduct or quality of care, PHC shall submit any and all required reports to the National Practitioner Data Bank and the State Medical Board.
J. Credentials files and all relevant credentialing and re-credentialing information are maintained as high level secured documents. Confidentiality is maintained via file storage in locked cabinets and access limited to the Chief Medical Officer or physician designee, Provider Relations Department Personnel, and the Quality Improvement Personnel. Practitioner information stored in an electronic database is confidential and secure, accessible only by personnel with a unique password.
K. The Provider Relations department performs ongoing monitoring of practitioner sanctions and complaints between re-credentialing cycles by reviewing the Medi-Cal Sanction Report, lists of parties excluded from Federal Procurement and Non-procurement program (Lists), Medi-Cal Participation Exclusion Report, State Boards “Hot Sheet” and member complaints.
VII. REFERENCES: - NCQA Policy/Procedure Number: MP CR #7A Lead Department: Provider Relations Policy/Procedure Title: Re-credentialing Criteria, Application/Attestation, and Monitoring of Sanctions for Behavioral Health Practitioners ☒ External Policy ☐ Internal Policy Original Date: 05/08/2002 Next Review Date: 08/09/2017 Last Review Date: 08/10/2016 Applies to: ☒ Medi-Cal ☐ Employees
VIII. DISTRIBUTION: - PHC Provider Manual
IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Credentialing Supervisor
X. REVISION DATES: 05/08/2002, 08/14/2002, 03/12/2003, 03/10/2004, 02/09/2005, 02/08/2006, 07/12/2006, 07/11/2007, 07/09/2008, 07/08/2009, 07/14/2010, 07/13/2011, 08/10/2012, 09/11/2013, 08/13/2014, 08/12/2015, 08/10/2016
PREVIOUSLY APPLIED TO: N/A
D:\Docs\2017-07-20\0072d357976394730b895dbf348cfd6e.docx Page 3 of 3