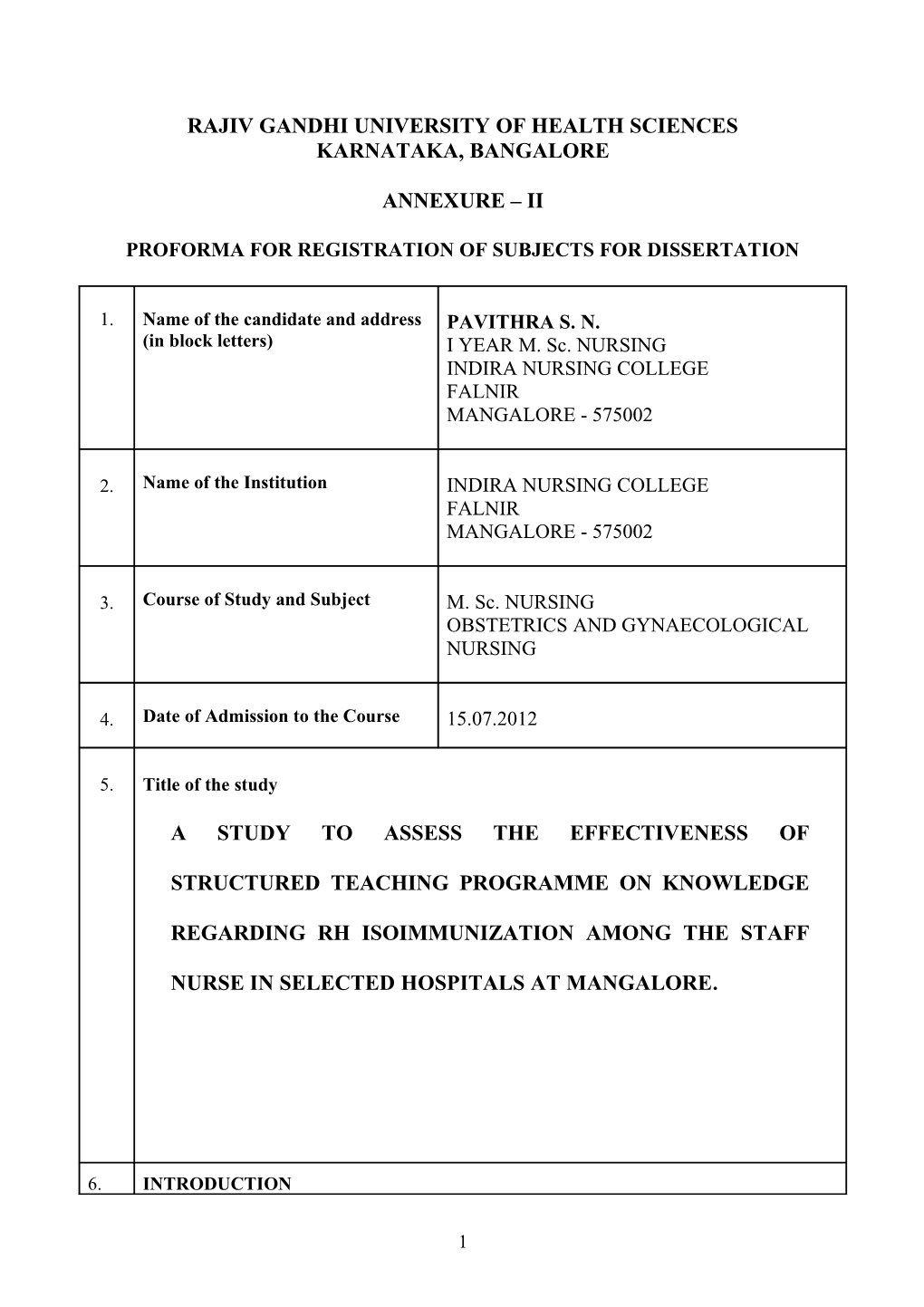
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES KARNATAKA, BANGALORE
ANNEXURE – II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. Name of the candidate and address PAVITHRA S. N. (in block letters) I YEAR M. Sc. NURSING INDIRA NURSING COLLEGE FALNIR MANGALORE - 575002
2. Name of the Institution INDIRA NURSING COLLEGE FALNIR MANGALORE - 575002
3. Course of Study and Subject M. Sc. NURSING OBSTETRICS AND GYNAECOLOGICAL NURSING
4. Date of Admission to the Course 15.07.2012
5. Title of the study
A STUDY TO ASSESS THE EFFECTIVENESS OF
STRUCTURED TEACHING PROGRAMME ON KNOWLEDGE
REGARDING RH ISOIMMUNIZATION AMONG THE STAFF
NURSE IN SELECTED HOSPITALS AT MANGALORE.
6. INTRODUCTION
1 The average woman who enters pregnancy in good health achieves a successful pregnancy and birth without complications. In a few women, however, for reasons that usually are unclear, unexpected deviations or complications from the course of normal pregnancy occur. When this happens, it can place a severe burden on a woman and her family. All families benefit from the support and skill of a professional nurse who helps them work through the tasks of pregnancy and prepare to become new parents. A complication that results in loss of the foetus can be devastating. Sometimes the complication of pregnancy puts the women’s life in danger and difficult treatment choices must be made, such as the risk to the foetus if she is delivered early.1
Brief resume of the intended work
6.1 Need for the study
Pregnancy is a unique and joyous time in a women’s life .The growing foetus depends entirely on its mother’s healthy body for needs. But some of the conditions make pregnancy and labour as high risk like Rh incompatibility, placenta previa etc. This can be prevented by administration of Rh (D) antibodies. Isoimmunization is defined as a production of immune antibodies in an individual in response to an antigens derived from another individual of the same species provided the first one takes the antigens.2
The Human red blood cells (RBC) membrane is complex and contains a variety of blood group antigens, the most clinically significant being , the ABO system and Rh system. The Rh system consist of two related proteins, RhD and R h CE, which express the D and CE antigens, respectively. People who have the D antigen on their RBCs are said to be Rh – D positive. Whereas those who do not have are said to be Rh –D negative. If the mother is Rh-D negative and foetus Rh-D positive the mother may react to foetal blood cells in her circulation by developing anti-D antibodies a process is known as Rh D sensitization.3
Rh isoimmunization is a process by which foetal Rh+ erythrocytes enter the circulation of an Rh mother causing her to produce immunoglobulin antibodies which can cross the placenta and destroy the erythrocytes of Rh + foetuses. Administration of a full
(300 llg) dose of Rh (D) immunoglobulin is recommended for all unsensitized Rh (D)
2 negative women after repeated antibody testing at 28-32 weeks gestation and another 1500 IU (300 mcg) with in 72 hours of birth of an Rh (D) positive baby, through IM or IV.4,2
If the mother forms these antibodies against Rh positive blood the antibodies cross from the mother in to the foetus and start destroying foetal blood cells. This lead to a serious condition in the foetus called erythroblastosis and destruction of the red blood cells various type of foetal haemolytic disease appear which may lead to anaemia, heart failure and even still birth. Rh antibodies can cause foetal heart problems, breathing difficulties, jaundice and erythroblastosis foetalis.2,5
The incidence of Rh negative in the European and American whites is about 15 -17 %. It is very much insignificant in china (1%) and almost nil in Japan. In India the incidence is about 5-10% [South India - 5%, North India - 10%] in hospital statistics; 5 to 10% of the black population are negative.2 Without prophylactic treatment the risk of foetal neonatal incompatibility is much higher. Without treatment 25-30% of those off spring will have some degree of haemolytic anaemia and hyperbilirubinemia and another 20-25 % will be hydropic and after will die either in utero or in neonatal anti-D prophylaxis. 1.6 % to 1.9 % Rh negative women at risk became sensitised. If Rh negative mother do not receive postpartum anti-D Ig G prophylaxis after an Rh positive baby the incidence of sensitization during the next pregnancy is 12% to 16% compared to 1.6 to 1.9 % in mother receiving post partum prophylaxis.6,7
A study conducted to assess the adequacy of knowledge on Rh immunoprophyxsis among obstetricians and trainees in obstetrics and gynaecology in Singapore. An anonymous questionnaire survey was conducted in their clinical setting. The results showed that the mean score achieved on the questionnaire was 75.9 % many obstetricians did not know that anti –D immunoglobulins (Ig) should be given within 72 hours of a sensitizing event for successful immunoprophylaxis. In clinical practice, all the obstetricians who participated in the questionnaire would offer anti-D Ig prophylaxis to Rh negative women both antenatally and postnatally. Only 12.7 % of them would routinely perform a Kleihauer test in Rh negative women following delivery. The study concluded that adequate teaching is needed on Rh isoimmunization among the obstetricians.8.
A study conducted to determine the incidence of rhesus (Rh) isoimmunization and the utilization rate of Rh – immunoprophylaxis in Nigeria. 77 Rh negative pregnant women
3 were included for this study. The study result showed that 15.4 and 38.2 % of women who received immune – prophylaxis following previous abortion and deliveries. The incidence of antenatal sensitization was 1.3%. Initial testing, at booking, for sensitization was not done in 36.5 % of the women, while 63.4% had no follow-up testing. The time of onset of neonatal jaundice was 26.5±14.6 hours in Rh positive infants, compared to 44.4±17.8 hours in Rh negative infants (p=0.07). The haematocrit of both groups of infants was similar [42.8±5.8 versus 44.5±5.3, p=0.6 ] the partner’s Rh status was determined in 59.7 % and the infant’s rhesus group in 71.6 . Immunoprophylaxsis rate was poor (44.8 %). The study concluded that the risk of haemolytic disease of the newborn with its attendant perinatal morbidity and mortality is real in our community, yet the rate of Rh isoimmunization remains quite low in this population.9
A descriptive retrospective study was conducted to assess the prevalence of Rh negative pregnant women in Rajavini Hospital in Bangkok. 147 Rh negative pregnant women were included for this study. The results showed the prevalence of Rh negative pregnant women who attended antenatal clinic was 0.31%. Foetal anaemia and neonatal jaundice were detected in 21.9% and 37.2%, respectively, and 68.14% of cases received antenatal anti-D immunoglobulin. Anti-D immunoglobulin prophylaxis significantly reduced the incidence of neonatal jaundice [p<0.05]. The study concluded that proper antenatal clinic and administration of anti-D prophylaxis will reduce incidence of jaundice and Rh negative pregnancy.10
The investigator found that many nurses were not having adequate knowledge about Rh isoimmunization. The investigator rightly justify that there was a need to bring awareness among the staff nurse regarding Rh isoimmunization. Review of literature and discussion with the experts also prompted the researcher to pursue the study.
6.2 Review of literature
A study was conducted on antenatal prophylaxis of Rh immunization with 250 llg anti-D immunoglobulin. 830 Rh negative primipravidae and multigravidae round the 32nd to 34th wks of gestation were included for this study. The results shows that 529 of women delivered Rh positive infants and received another injection of anti-D immunoglobulin (250 llg) within 72 hours of delivery, at the serological follow-up 8 months after delivery 2
4 women (0.4%) had weak anti-D antibodies by the Papain technique. No anti-D could be detected in these 2 women 14 and 20 months respectively. The study concluded that administration of Rh immunization with 250 llg anti-D immunoglobulin is necessary for antenatal mother.11
A retrospective study conducted on compliance with postpartum Rh isoimmunization prophylaxis in Alberta. Total 4528 women were selected for this study. The results found that the prevalence of Rh negativity was found to be 16% off the 710 Rh negative women 490(69%) were eligible to receive Rh immunoglobulin that is they had no anti-D antibodies and they baby/foetus was Rh positive or Rh unknown. The study concluded that administration of postpartum Rh isoimmunization will prevent the future baby to free from neonatal jaundice.12
A study was conducted on Rh isoimmunization during pregnancy in Manitoba. Total 3533 Rh negative pregnant women were selected for this study. The study result showed that 62 (1.8%) demonstrated evidence of Rh isoimmunization during pregnancy antenatal administration of Rh immunoglobulin initially 34 weeks and subsequently at 28 and 34 weeks gestation. In 1357 Rh negative pregnant women who were delivered of Rh positive babies. It was concluded that antenatal prophylaxsis with Rh immunoglobin is very necessary.13
A study conducted in Canada to qualify the magnitude of Rh disease reduction occurring secondary to Rh prophylaxsis. Outcomes considered included maternal Rh sensitization, neonatal Rh disease and perinatal deaths from Rh disease. The ecological analysis showed that changes in birth order and Rh prophylaxsis resulted in 24% (95% CI=1%,42%) and 69% (95% CI = 61% , 76%) decreases, respectively, in Rh sensitizations. Rh prophylaxis and non program factors were responsible for 83% (95%, CI=44%, 95%) and 78% (95% CI=42%, 91%) respectively, of the reduction in perinatal death from Rh disease. They study concluded that administration of Rh prophylaxsis is very effective in reduction of Rh disease.14
A conventional meta analysis study was conducted in Cambridge to estimate the effectiveness of routine antenatal anti-D prophylaxsis for preventing sensitization in
5 pregnant Rhesus negative women. In this study the pooled odds ratio for sensitization was estimated as 0.25 (95% CI 0.18, 0.36) comparing routine antenatal anti-D prophylaxsis to control with some heterogeneity (I2 =19%). The pooled odds ratio for sensitization was estimated as 0.31 (95% CI 0.17, 0.56) with no evidence of heterogeneity (I2=0%) a meta- regression analysis was performed which used the data available from the ten anti-D prophylaxsis studies to inform us about the relative effectiveness of three licensed treatment. This gave an 83% probability that a dose of 1250 IU at 28 and 34 weeks is most effective and a 76% probability that a single dose of 1500 IU at 28-30 weeks is least effective. The study concluded that effectiveness of routine antenatal anti-D prophylaxsis for prevention of sensitization in pregnant Rhesus negative women.15
A study was conducted assess the prenatal Rh immune prophylaxis with 300 micrograms immune globulin anti-D in the 28th wks of pregnancy in Kolding Hospital, Denmark. Six hundred and nine Rh negative women in the 28th week gestation were selected for the study. Three hundred 300 mg of immune globulin anti-D was administered to 609 Rh – negative women in the 28th gestational week. Three hundred and forty-six had Rh positive babies, and were given additionally 200 micrograms anti-D postpartum. Of these 291 had an antibody screen test done 10 months after delivery. The results shows that 354 women who did not receive prenatal immune globulin, in this group 322 had a screen test performed 10 months post partum or in their next pregnancy, when 1.8 % had anti-D antibodies the difference in immunization incidence between the group was significant (p less than 0.05). There was no difference between the groups regarding the number of women with foetal erythrocytes in serum after delivery, but the number of foetal erythrocytes found was significantly lower in the group receiving prenatal prophylaxis (p less than 0.01). The study concluded that prenatal Rh immune prophylaxis in the 28 wk of pregnancy was significantly effective.16
A retrospective study was conducted to determine the compliance rates for women being offered routine antenatal anti-D prophylaxsis in two obstetric units in William Harvey Hospital, UK. 207 Rh D negative women were selected for this study. The study results showed that routine women received the two doses of anti-D Ig G. The majority of women received their first and second doses within 1 week of 28 and 34 weeks gestation [87.0 and
86.0%, respectively]. The study concluded that level of patient compliance with the two dose regimen was high.17
6 The above studies shows that there is a need for bringing in awareness regarding the Rh isoimmunization among staff nurses, extensive research would help to improve the existing ones.
6.3 Statement of the problem
A study to assess the effectiveness of structured teaching programme on knowledge regarding Rh isoimmunization among the staff nurse in selected hospitals at Mangalore.
6.4 Objectives of the study
Objectives of the study are:
To assess the existing knowledge of staff nurses regarding Rh isoimmunization using structured knowledge questionnaire.
To evaluate the effectiveness of structured teaching programme on knowledge regarding Rh isoimmunization in terms of gain in the post-test knowledge score.
To find the association between mean pre-test knowledge scores regarding Rh isoimmunization among the staff nurse and selected demographic variables.
6.5 Operational definitions
Effectiveness: In the present study, effectiveness refers to the impact of structured teaching programme among the staff nurse regarding Rh isoimmunization.
Structured teaching programme: In the present study it refers to the educational programme for the staff nurse by using audio visual aids regarding Rh isoimmunization. The session includes administration of anti-D prophylaxsis, time of administration, dosage, route, incidence, and complications of Rh incompatibility.
Knowledge: In this study, it refers to the correct response from the staff nurse regarding Rh isoimmunization as elicited through structured knowledge questionnaire.
Rh isoimmunization: In the present study, it refers to the development of antibodies against the Rh antigens.
Staff nurse: In the study, it refers to the registered nurse either with B.Sc. nursing or diploma certificate programme in nursing and midwifery, working in maternity units of
7 selected hospital, Mangalore.
Hospital: In this study, hospital is an organized institution for the care of mothers who need maternity services.
6.6 Assumptions
Staff nurse may have some knowledge regarding Rh isoimmunization.
Structured teaching programme is an accepted strategy to improve knowledge.
Staff nurse will be interested to upgrade their knowledge on Rh isoimmunization.
6.7 Hypotheses
The hypothesis will be listed at 0.05 level of significance.
H1: The mean post-test knowledge score regarding Rh isoimmunization will be significantly higher than the mean pre- test knowledge score regarding Rh isoimmunization.
H2: There will be significant association between mean pre-test knowledge score regarding Rh isoimmunization among the staff nurse and selected demographic variables.
6.8 Delimitations
The study will be delimited to staff nurse:
Who are working in selected hospitals at Mangalore.
7. Material and methods
7.1 Source of data
Data will be collected from staff nurse who are attending selected hospitals at Mangalore.
8 7.1.1 Research design
Pre-experimental design will be used for the study. One group pre-test post-test will be selected for the study.
Subject Pre-test Treatment Post-test
Staff nurse attending selected O1 X O2 maternity hospital
R = O1 X O2
R: Sample
O1: Pre-test assessment of staff nurse concept regarding Rh isoimmunization.
X: Treatment (structured teaching programme regarding Rh isoimmunization).
O2: Post-test knowledge of staff nurse regarding Rh isoimmunization.
7.1.2 Setting
The study will be conducted at selected hospitals at Mangalore that provide maternity services.
7.1.3 Population
Staff nurses either B. Sc. nursing or diploma certified programme in nursing and midwives attending selected hospitals at Mangalore.
7.2 Method of data collection
7.2.1 Sampling procedure
Purposive sampling technique will be used to collect the sample.
7.2.2 Sample size
9 Sample size consists of 50 staff nurses.
7.2.3 Inclusion criteria for sampling
Staff nurse who are willing to participate in the study.
Staff nurse who are available during the period of data collection.
Staff nurse who are qualified in diploma and B. Sc. nursing.
7.2.4 Exclusion criteria for samplings
Staff nurse who are not willing to participate in study.
Staff nurse who are not available during the study.
Student nurses who are posted for clinical experience.
7.2.5 Instruments intended to be used
The following tool will be prepared and used for data collection:
Section A: Demographic variables.
Section B: Structured knowledge questionnaire regarding Rh isoimmunization.
7.2.6 Data collection method
Prior permission will be obtained from the higher authorities of the selected hospital. The purpose and need for the study will be explained to the staff nurse confidentially of the collected data will be assumed to the staff nurse and written consent will be obtained. A structured knowledge questionnaire regarding Rh isoimmunization will be distributed and requested to be filled by the respondents. The filled tool will be collected and structured teaching programme will be conducted for 30 minutes with the help of audio visual aids. After 7 days, post-test will be conducted to the same subject using the same structured knowledge questionnaire.
7.2.7 Plan for data analysis
The data will be analysed using both descriptive [mean, median, mean percentage,
10 and standard deviation] and inferential statistics (Chi-square test, paired ‘t’ test).
7.3 Does the study require any investigations or interventions to be conducted on patients, or other animals? If so please describe briefly.
Yes. In the present study the investigator plans to use structured knowledge questionnaire to evaluate the effectiveness of structured teaching programme regarding Rh isoimmunization.
7.4 Has ethical clearance been obtained from your institution in case of 7.3?
Yes, ethical clearance is obtained from the ethical committee of the institution.
8. References
1. Klossner J, Hatfield N. Introductory maternity and paediatric nursing. Philadelphia: Lippincott Williams & Wilkins Publications; 2006.
2. Dutta DC. Textbook of obstetrics including perinatology and contraception. 4th edition. Kolkata: Central Book Publication; 1998. P. 352-6.
3. Osaro E, Charles AT. Rh isoimmunization in Sub-Saharan Africa indicates need for universal access to anti-RhD immunoglobulin and effective management of D-
11 negative pregnancies. Int J Womens Health 2010 Dec 1;2:429-37.
4. Rh Isoimmunization. [online]. Available from: URL: http://www.reference.md/files/D012/mD012203.html
5. Rh incompatibility. [online]. Available from: URL: http:// www.mdguidelines.com/
6. http://odphp.osophs.dhhs.gov/pubs/guidecps/PDF/CH38.PDF.
7. Fung K, Fung K, Eason E. Prevention of Rh alloimmunization. Canada: SOGC Clinical Practice Guidelines 2003 Sep;133.
8. Kanagalingam D. the use of anti–D immunoglobulins for rhesus prophylaxis : audit on knowledge and practices among obstetricians. Singapore: Singapore Medical Journal 2009;11:1054-7.
9. Fawole AO. A review of Rhesus iso-immunization in a Nigerian obstetric population. Tropical Journal of Obstetrics and Gynaecology 2001;18(2):69-72.
10. Puangsricharern A, Suksawat S. Prevalence of Rh negative women who attended the antenatal clinic and delivered in Rajavithi Hospital, Thailand. Journal of the Medical Association of Thailand 2007;90(8):1491-4.
11. Hermann M, Kjellman H, Ljunggren C. Antenatal prophylaxis of Rh immunization with 250 micrograms anti-D immunoglobulin. Acta Obstet Gynecol Scand Suppl 1984;124:1-15.
12. Huchroft S, Gunton P, Bowen T. Compliance with postpartum Rh isoimmunization prophylaxis. Canadian Medical Journal 1985 Nov 1;133(9):871-5.
13. Bowman JM, Chown B, Lewis M, Pollock JM. Rh isoimunisation during pregnancy: antenatal prophylaxis. Can Med Asso J 1978 Mar 18;118(6):623- 627.
14. Joseph KS, Kramer MS. The decline in Rh haemolytic disease: should Rh prophylaxis get all the credit? American Journal of Public Health. 1998;88(2):209- 15.
15. Turner RT. Routine antenatal anti-D prophylaxis in women who are Rh (D) negative:
12 meta analyses adjusted for differences in study design and quality. [online]. Available from: URL:www.plosone.org.
16. Trolle B. Prenatal Rh-immune prophylaxis with 300 micrograms immune globulin anti-D in the 28th week of pregnancy. Acta Obstet Gynecol Scand 1989;68(1):45-7.
17. Chaffe B, Ford J, Bills V. Routine antenatal anti-D prophylaxis and patient compliance with the two-dose regimen. Transfus Med 2007 Oct;17(5):399-403.
13 9. Signature of the candidate
10. Remarks of the guide
11. Name and designation of (in block letters)
11.2 Guide MRS. LIZZIE D’COSTA PROFESSOR AND HOD OBSTETRICS AND GYNAECOLOGICAL NURSING INDIRA NURSING COLLEGE FALNIR, MANGALORE – 575 002.
11.2 Signature
11.3 Co-guide (if any)
11.4 Signature
12 12.1 Head of the department MRS. LIZZIE D’COSTA PROFESSOR AND HOD OBSTETRICS AND GYNAECOLOGICAL NURSING INDIRA NURSING COLLEGE FALNIR, MANGALORE – 575 002.
12.2 Signature
13. 13.1 Remarks of the Chairman and Principal
13.2 Signature
14