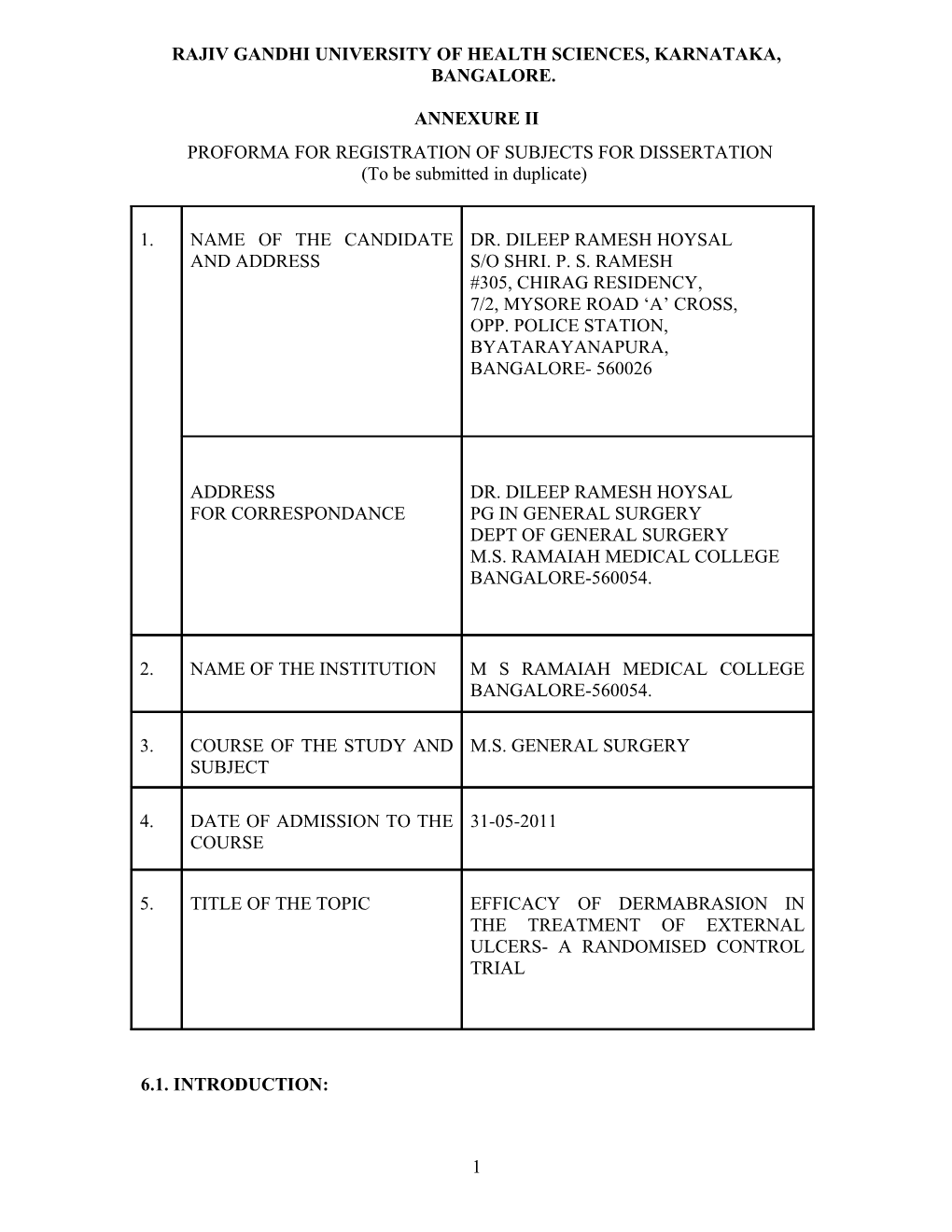
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA, BANGALORE.
ANNEXURE II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION (To be submitted in duplicate)
1. NAME OF THE CANDIDATE DR. DILEEP RAMESH HOYSAL AND ADDRESS S/O SHRI. P. S. RAMESH #305, CHIRAG RESIDENCY, 7/2, MYSORE ROAD ‘A’ CROSS, OPP. POLICE STATION, BYATARAYANAPURA, BANGALORE- 560026
ADDRESS DR. DILEEP RAMESH HOYSAL FOR CORRESPONDANCE PG IN GENERAL SURGERY DEPT OF GENERAL SURGERY M.S. RAMAIAH MEDICAL COLLEGE BANGALORE-560054.
2. NAME OF THE INSTITUTION M S RAMAIAH MEDICAL COLLEGE BANGALORE-560054.
3. COURSE OF THE STUDY AND M.S. GENERAL SURGERY SUBJECT
4. DATE OF ADMISSION TO THE 31-05-2011 COURSE
5. TITLE OF THE TOPIC EFFICACY OF DERMABRASION IN THE TREATMENT OF EXTERNAL ULCERS- A RANDOMISED CONTROL TRIAL
6.1. INTRODUCTION:
1 A wound is a microcosm of the patient. Most wounds will heal with minimal intervention in a healthy individual. Conversely, the incidence of nonhealing wounds is higher in patients with systemic diseases, particularly those who are hospitalized. Management of these ulcers is a topic of great interest. Some of the basic methods of managing ulcers can be summarized as Debridement of non-viable tissues, reduction of edema, appropriate dressing, Antibiotics if necessary, Control of co-morbidities, Close wounds surgically with grafts or flaps1.
Debridement prepares the wound for healing by reducing the bioburden. Without an adequate debridement, a wound is persistently exposed to cytotoxic stressors and competes with bacteria for scarce resources such as oxygen and nutrients.
Dermabrasion is a tool in the management of dermatological conditions like post-acne scarring, naevi, adenoma sebaceum and also in the management of burns2. In this study the use of dermabrasion as a debridement tool in the management of ulcers shall be evaluated.
6.2 REVIEW OF LITERATURE:
Microdermabrasion activates a dermal remodeling/wound healing cascade with minimal epidermal disruption3.
Microdermabrasion appears to be a procedure that can produce changes in dermal matrix constituents and result in improvement in skin contour irregularities4. thickening of the epidermis and dermis, flattening of the rete pegs, vascular ectasia and perivascular inflammation, and hyalinization of the papillary dermis with newly deposited collagen and elastic fibers were observed5.
Dermal thickness was increased by as much as 40% in the thinner skin and by 27% in the thicker skin. Similarly, the increase in collagen-bundle thickness was 22%, whereas the increase in the epidermal thickness was 9%6.
Similar tissue effects were seen with Low-energy shock wave therapy (SWT) improves healing of diabetic and vascular ulcers by over expression of vascular endothelial growth factor and down regulation of necrosis factor κB. Higher incidence of wound healing disorders necessitating antibiotic treatment in the control group 22% as compared with the SWT group 4% was observed7.
The ASEPSIS wound score is done to assess the progress of wound healing; Lower ASEPSIS scores were observed indicating improved wound healing in the SWT group 4.4 ± 5.3 compared with the control group 11.6 ± 87-9.
This principle of dermabrasion is to be used and evaluated in the management of ulcers.
6.3. OBJECTIVES OF THE STUDY:
To assess the usefulness and effects of dermabrasion in the management of ulcers.
2 To compare the outcome of dermabrasion with the conventional method. Assessment of Wound healing. No of days of Hospital stay. Pain during the procedure
7. MATERIALS AND METHODS:
7.1 METHOD OF COLLECTION OF DATA:
A. Source of patients: Patients attending surgical outpatient clinic or admitted into the hospital (MSR GROUP OF HOSPITALS) will be recruited into the study based on the inclusion and exclusion criteria mentioned below. The baseline demographic data which includes age, sex, occupation, education status, habits, socioeconomic status and treatment history will be taken. These patients will be divided using a random number table into 2 groups: Group 1 (Conventional group) receiving the standard conventional treatment for ulcers existing in our hospital setup i.e.; antibiotics, regular cotton gauze with betadine dressings, occasional debridement with scoop if required
Group 2 (Trial group) who will receive all the components of standard treatment except for conventional debridement which will be replaced by dermabrasion done on alternate days.
B. Device: Dermabrasion is done using high-speed rotating head dermabrader (Aesculap GA 415) with 4200 rpm.
C. Wound Healing Assessmen t: The wound healing will be assessed and quantified using the ASEPSIS score, which is a scoring method for postoperative wound infections. Based on the ASEPSIS score, wound healing was quantified by a blinded investigator from postoperative days 3, 7, 11 and 15.
The ASEPSIS wound score
Criterion Points Additional treatment Antibiotics for wound infection 10 Drainage of pus under local anaesthesia 5 Debridement of wound under general anaesthesia 10 Serous discharge Daily 0-5 Erythema Daily 0-5 Purulent exudate Daily 0-10 Separation of deep tissues Daily 0-10 Isolation of bacteria from wound 10 Stay as in-patient prolonged over 14 days as result of wound infection 5 3 D. Pain assessment: Visual analogue scale is used for the assessment of pain before and after the procedure and is compared to the conventional method. It is a 10 cm line grading pain from NO pain to WORST pain as experienced by the patient10.
STATISTICAL ANALYSIS:
Rational for sample size A study carried out by Dumfarth et al. has indicated that the incidence of wound healing disorders in the conventional treatment group was 22% as compared with the shock wave therapy group (4%) 7.
The above findings have been utilized for estimating sample size for the study in order to demonstrate a statistical significance between the incidence of above disorders it is estimated that 42 patients need to be included into the study at a power of 80% and α error of 10%.
The above sample size would be able to demonstrate statistical significance with regard to ASEPSIS scores also. Thus it is proposed to include 42 patients in each of the groups/categories namely conventional and dermabrasion method.
Although conventionally α error is taken as 5% in present study due to logistic consideration and time frame α error of 10% has been considered.
Statistical analysis of the data
Quantitative parameters such as age, duration of disease, ASEPSIS scores will be summarized in terms of mean and standard deviation (as a measure of variation). Differences in mean scores will be tested for significance by employing Student ‘t’ test or appropriate non parametric test of significance. Incidence of wound healing disorders will be estimated as proportion in each of the group and differences in the proportion will be tested for statistical significance by employing ‘Z’ test or Chi-square test of significance.
7.2 Inclusion criteria:
Age limit: 20-80years.
All subjects having ulcers in upper or lower extremities attending MSR GROUP OF HOSPITALS admitted to the wards with an ulcer.
7.3 Exclusion criteria:
Patients with less than two weeks of treatment period.
4 Patients suffering from anemia, hypoproteinemia, immunocompromised states like chronic steroid intake, malnourished, malignancy.
7.4 Does the study require any investigations or interventions to be conducted on patients or other humans or animals?
Yes.
7.5 Has ethical clearance been obtained from your institution?
Yes.
5 8. REFERENCES:
1. Robert D. Galiano, Thomas A. Mustoe. Wound Care In:Charles H. Thorne, Robert W. Beasley, Sherrell J. Aston,et al. editors: Grabb and Smith's Plastic Surgery, 6th ed. Philadelphia: Lippincott Williams&Wilkins, a Wolters Kluwer Business; 2007. p:23
2. J. S. Pegum, editor. Dermabrasion: Section of dermatology: 1957: Proceedings of the Royal Society of Medicine; 50:607.
3. Karimipour DJ, Kang S, Johnson TM, Orringer JS, Hamilton T, Hammerberg C, Voorhees JJ, Fisher G. Microdermabrasion: a molecular analysis following a single treatment. J Am Acad Dermatol. 2005 Feb; 52(2):215-23.
4. Karimipour DJ, Karimipour G, Orringer JS. Microdermabrasion: an evidence- based review. Plast Reconstr Surg. 2010 Jan; 125(1):372-7.
5. Freedman BM, Rueda-Pedraza E, Waddell SP. The epidermal and dermal changes associated with microdermabrasion. Dermatol Surg. 2001 Dec; 27(12):1031-3; discussion 1033-4.
6. Shehadi IE, Larson DL, Archer SM, Zhang LL. Evaluation of histologic changes after microdermabrasion in a porcine model. Aesthet Surg J. 2004 Mar-Apr; 24(2):136-41.
7. Julia Dumfarth, Daniel Zimpfer, Margit Vögele-Kadletz, et al. Prophylactic Low-Energy Shock Wave Therapy Improves Wound Healing After Vein Harvesting for Coronary Artery Bypass Graft Surgery: A Prospective, Randomized Trial. Ann Thorac Surg. 2008; 86:1909-1913.
8. David J. Leaper. Surgical infection. In: Norman S. Williams, Christopher J.K. Bulstrode, P. Ronan O’Connell. Editors. Bailey and love’s short practice of surgery. 25th ed. Edward Arnold (Publishers) Ltd; 2008. p.36
9. Wilson A, Treeasure T, Sturridge MF, et al. A scoring method (ASEPSIS) for postoperative wound infections for use in clinical trials of antibiotic prophylaxis. Lancet. 1986;8:311-313
10. Wewers. M.E, Lowe. N.K. A critical review of visual analogue scales in the measurement of clinical phenomena. Research in Nursing and Health. 1990;13: 227-236.
6 SIGNATURE OF THE 9 CANDIDATE
10 REMARKS OF THE GUIDE
11 NAME AND DESIGNATION OF
DR. VIJAYAKUMAR. H. M. M.B.B.S, M.S 11.1 GUIDE PROFESSOR, DEPARTMENT OF GENERAL SURGERY M.S.RAMAIAH MEDICAL COLLEGE BANGALORE-560054.
11.2 SIGNATURE
7 11.3 HEAD OF THE DEPARTMENT DR. M. R .SREEVATHSA. M.B.B.S, M.S PROFESSOR AND HEAD DEPARTMENT OF GENERAL SURGERY M.S.RAMAIAH MEDICAL COLLEGE BANGALORE-560054.
11.4 SIGNATURE
12.1 REMARKS OF DEAN AND PRINCIPAL
Dr. SARASWATHI.G.RAO M.D. PRINCIPAL AND DEAN M.S. RAMAIAH MEDICAL COLLEGE BANGALORE-560054.
12.2 SIGNATURE
8