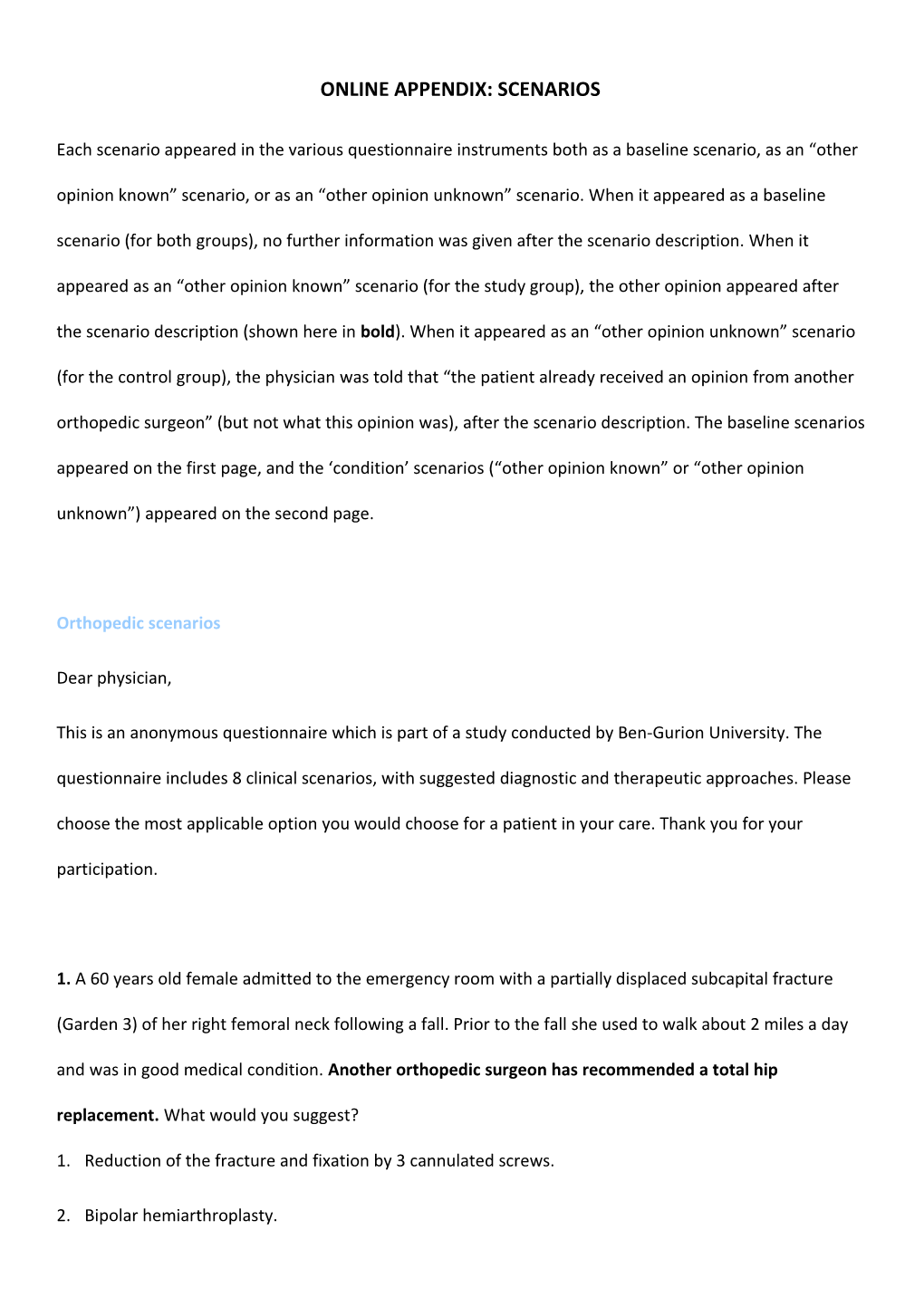
ONLINE APPENDIX: SCENARIOS
Each scenario appeared in the various questionnaire instruments both as a baseline scenario, as an “other opinion known” scenario, or as an “other opinion unknown” scenario. When it appeared as a baseline scenario (for both groups), no further information was given after the scenario description. When it appeared as an “other opinion known” scenario (for the study group), the other opinion appeared after the scenario description (shown here in bold). When it appeared as an “other opinion unknown” scenario
(for the control group), the physician was told that “the patient already received an opinion from another orthopedic surgeon” (but not what this opinion was), after the scenario description. The baseline scenarios appeared on the first page, and the ‘condition’ scenarios (“other opinion known” or “other opinion unknown”) appeared on the second page.
Orthopedic scenarios
Dear physician,
This is an anonymous questionnaire which is part of a study conducted by Ben-Gurion University. The questionnaire includes 8 clinical scenarios, with suggested diagnostic and therapeutic approaches. Please choose the most applicable option you would choose for a patient in your care. Thank you for your participation.
1. A 60 years old female admitted to the emergency room with a partially displaced subcapital fracture
(Garden 3) of her right femoral neck following a fall. Prior to the fall she used to walk about 2 miles a day and was in good medical condition. Another orthopedic surgeon has recommended a total hip replacement. What would you suggest?
1. Reduction of the fracture and fixation by 3 cannulated screws.
2. Bipolar hemiarthroplasty. 3. Unipolar hemiarthroplasty.
4. Total hip replacement.
2. A 52 years old female, has acute sciatica for the past 5 weeks that has partially resolved with physiotherapy and NSAIDs. She is neurologically intact. A CT demonstrates a L5-S1 herniated disc. She reports similar episodes 2-3 times a year in the past 3 years treated with NSAIDS. She works as a bank manager and has no medical co-morbidities. The patient is admitted to your care. Another orthopedic surgeon has recommended a L5-S1 disc replacement. What would you suggest?
1. L5-S1 disc replacement.
2. Conservative treatment and follow up in 3 weeks.
3. Discectomy.
3. A 17 years old teenager, a promising basketball player, dislocated his left shoulder a month ago. He denies prior dislocations. Another orthopedic surgeon has recommended an arthroscopic capsular shift.
What would you suggest?
1. Physiotherapy and follow-up.
2. Arthroscopic capsular shift.
4. A 53 years old taxi driver was injured in a car accident and suffered from a peritrochanteric fracture. He was treated by a Dynamic Hip Screw (DHS) and returned to full weight bearing. He complains of new pain around the hip that started several days after his surgery. Radiographs demonstrate a cut out of the DHS screw. His pain is controlled by Percocet 1-2 tabs every 6 hours. Another orthopedic surgeon has recommended Total Hip Arthroplasty (THA). What would you suggest?
1. Continue with pain control medications until fracture heals and re-evaluate in 2 months. 2. Removal of the failed DHS and a second attempt of Open Reduction Internal Fixation (ORIF) by a
cephalomedullary nail or fixed angle device.
3. Total Hip Arthroplasty (THA).
5. A construction worker fell from a height and has a displaced Pylon fracture (type C according to Rudi and
Allgower) with extensive metaphyseal comminution. He arrived to the ER on hour after the injury.
Another orthopedic surgeon has recommended Arthrodesis. What would you suggest?
1. Arthrodesis.
2. Calcaneal traction for 10-14 days until soft tissue recovers and then consider ORIF or an Ilizarov.
3. ORIF or Ilizarov within 12 hours from injury.
6. A 60 years old female arrived to the ER with a displaced bimalleolar (medial and lateral) fracture of the right ankle. A closed reduction was performed. Post reduction radiographs demonstrate well reduced medial malleoulus and a 1-2 mm displacement of the lateral malleolus on lateral view. AP and mortise view demonstrate well reduced malleoli. She is treated for osteoporosis after a distal radius fracture 1 year ago.
Another orthopedic surgeon recommended ORIF. What would you suggest?
1. Cast for 6 weeks.
2. ORIF of right ankle.
3. Follow up in 2 weeks in the fracture clinic. Only if a greater displacement is witnessed than ORIF.
7. A 60 years old kindergarten assistant with right shoulder pain. She has a rotator cuff tear of 2 cm demonstrated by ultrasound. The pain has not diminished despite 1 month of physiotherapy and NSAIDs.
Another orthopedic surgeon recommended arthroscopic decompression and rotator cuff repair. What would you suggest? 1. Arthroscopic decompression and rotator cuff repair.
2. Continue physiotherapy, NSAIDs for up to 3 months and then re-evaluate.
8. A 72 years old male 4 weeks post left knee cemented TKA. He complains of continuous pain around the knee even at rest. The knee has a mild effusion, without redness or secretion from the wound. Range of motion is 0-90 degrees. He had several episodes of fever up to 38.6 degrees. His blood count is
WBC=12,800 with 90% of neutrophilles. His CRP is 24 and his ESR 50. Two blood cultures grew Staph.
Epidermidis (not a contaminant) sensitive to Methicylin. Another orthopedic surgeon recommended two- stage revision of the knee with a 3 months interval. What would you suggest?
1. Two stage revision of the knee with a 3 months interval.
2. IV antibiotics for 3 weeks followed by 6 weeks of antibiotics PO.
3. Irrigation and debridement of the knee followed by the above antibiotics protocol. Responses of the orthopedic surgeons (n=172):
Scenario Original Ordinal Ordinal As a baseline scenario As a ‘condition’ scenario
response *classification classification (Other opinion is unknown (Control group (Other opinion is known (Study group for
cumulative
ordinal
regression
((GEE 1 1 1 Low (59.3%) 51 (54.2%) 32 (25.9%) 7 2 3 Medium (23.3%) 20 (27.1%) 16 (29.6%) 8 3 2 Medium (11.6%) 10 (11.9%) 7 (22.2%) 6 4 4 High (5.8%) 5 (6.8%) 4 (22.2%) 6 2 1 3 High (26.7%) 23 (25.4%) 15 (22.2%) 6 2 1 Low (60.5%) 52 (54.2%) 32 (25.9%) 7 3 2 Medium (12.8%) 11 (20.3%) 12 (51.9%) 14 3 1 1 Low (50.0%) 43 (40.7%) 24 (18.5%) 5 2 2 High (50.0%) 43 (59.3%) 35 (81.5%) 22 4 1 1 Low (19.8%) 17 (25.4%) 15 (44.4%) 12 2 2 Medium (39.5%) 34 (40.7%) 24 (18.5%) 5 3 3 High (40.7%) 35 (33.9%) 20 (37.0%) 10 n of physicians in Scenarios 1-4 86 59 27 5 1 3 High (61.6%) 53 (48.2%) 27 (70.0%) 21 2 1 Low (23.3%) 20 (28.6%) 16 (10.0%) 3 3 2 Medium (15.1%) 13 (23.2%) 13 (20.0%) 6 6 1 2 Medium (29.1%) 25 (33.9%) 19 (6.7%) 2 2 3 High (3.5%) 3 (14.3%) 8 (26.7%) 8 3 1 Low (67.4%) 58 (51.8%) 29 (66.7%) 20 7 1 2 High (41.9%) 36 (44.6%) 25 (36.7%) 11 2 1 Low (58.1%) 50 (55.4%) 31 (63.3%) 19 8 1 3 High (14.0%) 12 (7.1%) 4 (16.7%) 5 2 2 Medium (62.8%) 54 (71.4%) 40 (80.0%) 24 3 1 Low (23.3%) 20 (21.4%) 12 (3.3%) 1 n of physicians in Scenarios 5-8 86 56 30 * ‘1’ is the least interventional option. The greatest score (2, 3 or 4) is the most interventional option. Neurological scenarios
Dear physician,
This is an anonymous questionnaire which is part of a study conducted by Ben-Gurion
University. The questionnaire includes 8 clinical scenarios, with suggested diagnostic and therapeutic approaches. Please choose the most applicable option you would choose for a patient in your care. Thank you for your participation.
1. A 24 years old female, after hospitalization due to Optic Neuritis. MRI showed 9 Supra- and infera-tantorial lesions. Another neurologist has recommended an Immuno- modulatory treatment. What would you suggest?
1. Start an Immuno-modulatory treatment.
2. MRI follow-up in 6 months.
3. Clinical follow-up only.
2. A 72 years old female, complaining intermittent ptosis, especially during the evening.
Examination showed light symmetric ptosis with no response to Tensilon test. Another neurologist has recommended Mestinon therapeutic trial. What would you suggest?
1. Mestinon therapeutic trial.
2. No treatment. Blood AChR antibodies, TSH, and Repetitive stimulation. 3. Clinical follow-up in two months.
3. A 69 years old male after mild ischemic stroke. TEE showed Patent Foramen Ovale.
Another neurologist has recommended anticoagulant treatment and closing the PFO.
What would you suggest?
1. Long anticoagulant treatment.
2. Anticoagulant treatment and closing the PFO.
3. Aspirin therapy and clinical follow-up.
4. A 37 years old female with frequent migranous headache attacks for two years.
Neurological examination and brain CT with contrast material are normal. Does not respond to tryptan and to prophylaxis treatment with beta-blockers. Another neurologist has recommended MRI, MRV and LP. What would you suggest?
1. MRI.
2. MRI, MRV and LP.
3. Other prophylaxis treatment and clinical follow-up.
5. A 70 years old male, examined due to a change in handwriting. Examination showed mild hipomimia and rigidity in the upper right limb. Light tremor at rest in both hands. Another neurologist has explained to the patient that he has a Parkinson's disease, and began treatment with L-DOPA. What would you suggest? 1. I will explain to the patient that he has a Parkinson's disease, and begin treatment with L-
DOPA.
2. I will explain to the patient that he has a Parkinson's disease, and begin treatment with
Dopamine agonist.
3. I will explain to the patient that he has a Parkinson's disease, and will recommend
exercise and follow-up.
4. I will not tell to the patient that he has a Parkinson's disease, and do clinical follow-up.
6. A diabetic patient with right occulomotor palsy for 3 weeks without pupillary involvement.
Another neurologist has recommended CT and ANGIO of the brain. What would you suggest?
1. Brain CT.
2. CT and ANGIO of the brain.
3. Clinical follow-up and treatment with vitamins.
7. A 22 years old male after a loss of consciousness event with characteristics of Generalized
Tonic Clonic Seizure. Brain CT scan with contrast material and EEG were normal. Another neurologist has recommended anantiepileptic treatment. What would you suggest?
1. Begin antiepileptic treatment.
2. Brain MRI.
3. EEG in sleep deprivation. 4. Clinical follow-up only.
8. A 68 years old male complaining of minor cognitive impairment. Mini mental status exam
(MMSE) – 27. Known to have multiple cardiovascular risk factors. No additional findings.
VDRL, TSH and B12 are normal. Another neurologist has recommended brain MRI and lumbar puncture. What would you suggest?
1. Brain MRI and lumbar puncture.
2. Initiate treatment with central anticholinesterase drugs.
3. Clinical follow-up only. Responses of the neurologists (n=160):
Scenario Original Ordinal Ordinal As a baseline scenario As a ‘condition’ scenario
response *classification classification
for (Other opinion is unknown (Control group
cumulative
ordinal
regression
((GEE 1 1 3 High (7.9%) 6 (8.3%) 5 2 2 Medium (19.7%) 15 (16.7%) 10 3 1 Low (72.4%) 55 (75.0%) 45 2 1 3 High (2.6%) 2 (5.0%) 3 2 2 Medium (80.3%) 61 (90.0%) 54 3 1 Low (17.1%) 13 (5.0%) 3 3 1 2 Medium (56.6%) 43 (66.7%) 40 2 3 High (18.4%) 14 (6.7%) 4 3 1 Low (25.0%) 19 (26.7%) 16 4 1 2 Medium (55.3%) 42 (68.3%) 41 2 3 High (19.7%) 15 (16.7%) 10 3 1 Low (25.0%) 19 (15.0%) 9 n of physicians in Scenarios 1-4 76 60 5 1 4 High (4.8%) 4 (4.4%) 2 2 3 Medium (17.9%) 15 (20.0%) 9 3 2 Medium (53.6%) 45 (33.3%) 15 4 1 Low (23.8%) 20 (42.2%) 19 6 1 2 Medium (52.4%) 44 (37.8%) 17 2 3 High (25.0%) 21 (28.9%) 13 3 1 Low (22.6%) 19 (33.3%) 15 7 1 4 High (11.9%) 10 (15.6%) 7 2 3 Medium (38.1%) 32 (37.8%) 17 3 2 Medium (40.5%) 34 (42.2%) 19 4 1 Low (9.5%) 8 (4.4%) 2 8 1 3 High (66.7%) 56 (62.2%) 28 2 2 Medium (9.5%) 8 (8.9%) 4 3 1 Low (23.8%) 20 (28.9%) 13 n of physicians in Scenarios 5-8 84 45 * ‘1’ is the least interventional option. The greatest score (2, 3 or 4) is the most interventional option.