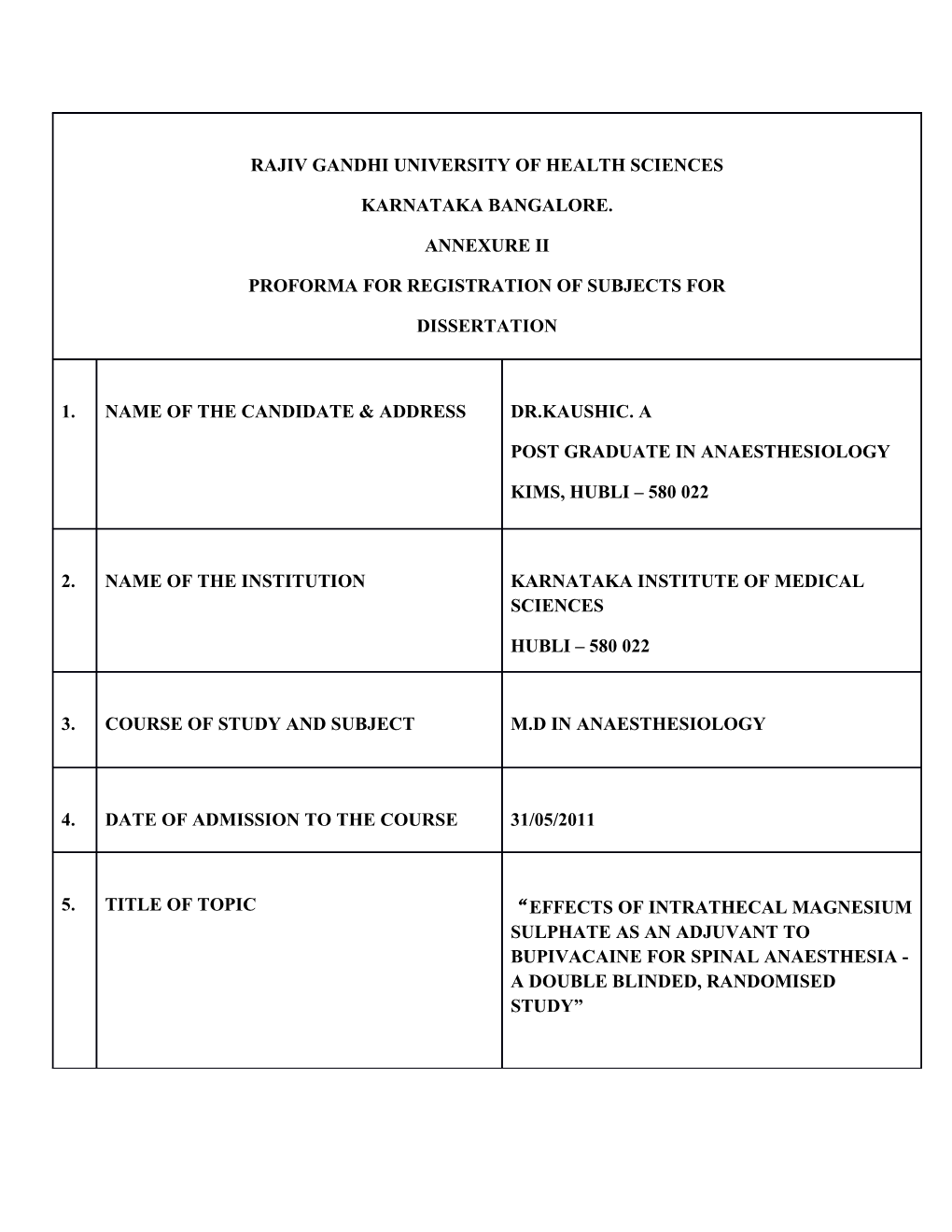
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
KARNATAKA BANGALORE.
ANNEXURE II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR
DISSERTATION
1. NAME OF THE CANDIDATE & ADDRESS DR.KAUSHIC. A
POST GRADUATE IN ANAESTHESIOLOGY
KIMS, HUBLI – 580 022
2. NAME OF THE INSTITUTION KARNATAKA INSTITUTE OF MEDICAL SCIENCES
HUBLI – 580 022
3. COURSE OF STUDY AND SUBJECT M.D IN ANAESTHESIOLOGY
4. DATE OF ADMISSION TO THE COURSE 31/05/2011
5. TITLE OF TOPIC “EFFECTS OF INTRATHECAL MAGNESIUM SULPHATE AS AN ADJUVANT TO BUPIVACAINE FOR SPINAL ANAESTHESIA - A DOUBLE BLINDED, RANDOMISED STUDY” 6. BRIEF RESUME OF INTENDED WORK : 6.1 NEED FOR STUDY
Duration of spinal analgesia can be prolonged by a number of additives1. New ways of decreasing post operative analgesic requirements are of special interest after major surgery2. Adequate analgesia following major surgery, decreases morbidity, hastens ambulation & improves patient outcome.
Magnesium blocks NMDA channels in a voltage dependent fashion & such NMDA antagonism can prevent the induction of central sensitisation from peripheral nociceptive stimulation3. However, intravenous magnesium even at higher doses has limited passage across blood brain barrier to act on NMDA channels4. Intrathecal administration of magnesium has been reported to potentiate opioid nociception2, 5&6 & prolong duration of anaesthesia6, 7&8. Intrathecal magnesium combined with opioids reduces postoperative opioid consumption2,5&6. But opioids given intrathecally may be associated with side effects. Intrathecal magnesium used as a sole anaesthetic adjuvant in single dose is also shown to strengthen analgesic effect of spinal local anaesthesia9.
This study is designed to investigate the effects of intrathecal magnesium as a sole anaesthetic adjuvant, and compare it with the well known adjuvant Buprenorphine and with a placebo, on onset, duration and quality of sensory and motor blockade, time to maximum dermatomal level of sensory block and duration of effective analgesia (calculated as time from intrathecal injection to first analgesic request).
6.2 REVIEW OF LITERATURE:
A randomized study on sixty women with mild pre-eclampsia undergoing cesarean section showed that the addition of magnesium sulphate 50mg to intrathecal combination of bupivacaine and fentanyl prolonged duration of analgesia and reduced postoperative analgesic requirements without additional side effects6. A randomized controlled trial on 52 patients requesting labour analgesia showed that intrathecal magnesium as magnesium sulphate 50mg prolonged fentanyl analgesia7.
A randomized, double blind study on sixty ASA 1 / 2 patients who received intrathecal magnesium as magnesium sulphate 50mg with low dose bupivacaine and fentanyl combination for knee arthroscopy revealed prolonged time for regression of two segments of maximum block height and prolonged time to first analgesic requirement8.
A study on sixty patients enrolled for Total Knee Replacement surgery receiving single dose of intrathecal magnesium sulphate with 0.5% tetracaine showed that intrathecal magnesium can be used as a local anaesthetic adjuvant to strengthen the analgesic effect of spinal local anaesthetic and to intensify the analgesic effect of epidural local anaesthetic for post operative pain9.
A systematic review of intrathecal magnesium given alone or in combination with local anaesthetic or opioids concluded that intrathecal magnesium prolonged duration of spinal analgesia and decreased post operative analgesic requirement but delayed the onset of block and time of maximal sensory block1.
A randomized, placebo controlled, double blind trial on 58 patients, undergoing pulmonary resection with posterolateral thoracotomy found that 50mg magnesium sulphate, when added to spinal morphine, reduced post operative morphine requirements and the number of patients requiring morphine titration without increasing opioid side effects5.
In a trial on 120 patients undergoing major lower limb orthopedic surgery supplementation of spinal anaesthesia with combined intrathecal and epidural magnesium sulphate significantly reduced patients’ postoperative analgesic requirements compared to intrathecal magnesium sulphate, epidural magnesium sulphate and spinal anaesthesia alone2.
6.4 OBJECTIVES OF STUDY
1. To evaluate the effects of intrathecal magnesium sulphate as an adjunct to bupivacaine on onset, duration, time for maximal sensory block and quality of sensory block and compare these with intrathecal buprenorphine.
2. To evaluate the effects of intrathecal magnesium sulphate as an adjunct to bupivacaine on onset, duration and quality of motor block and compare these with intrathecal buprenorphine.
3. To study the occurrence of adverse effects like hypotension, bradycardia, respiratory depression, drowsiness, nausea, vomiting and pruritis with intrathecal magnesium sulphate and compare these with intrathecal buprenorphine.
4. To determine the duration of effective analgesia when magnesium sulphate is added to intrathecal bupivacaine, to compare it with buprenorphine and thereby to study its role in postoperative analgesia. 7. MATERIALS AND METHODS
7.1 SOURCE OF DATA
Adult patients (18 – 55 years) of physical status I & II scheduled to undergo elective surgical procedures below the level of umbilicus under spinal anaesthesia at Karnataka Institute of Medical Sciences from 1st of January 2012 to 31st of December 2012.
7.2 METHOD OF COLLECTION OF DATA
A prospective, randomized, double blind, placebo controlled study is planned in 90 patients of physical status ASA I & II, aged between 18 to 55 years, scheduled to undergo elective surgery below the level of umbilicus and who satisfy all the inclusion criteria.
INCLUSION CRITERIA
1. ASA I & II.
2. Aged between 18 and 55 years.
3. Patients giving informed written consent.
4. Patients scheduled to undergo elective surgical procedures below the level of umbilicus under spinal anaesthesia
EXCLUSION CRITERIA
1. ASA III & IV.
2. Extremes of age <18 & >55 years.
3. Contraindication to regional anaesthesia.
4. History of allergy to magnesium sulphate, bupivacaine or buprenorphine.
5. History of opioid medication or magnesium treatment prior to surgery.
6. History of central or peripheral neuropathies. 7. Significant coexisting disease.
8. Parturients.
9. Unwillingness to regional anaesthesia
10. History of seizures
METHODS
All the patients satisfying the inclusion criteria will be assessed before the day of surgery and informed written consent will be obtained. Patients will be premedicated with tablet Diazepam 0.2mg/kg body weight orally on the night before surgery. Patients will be then randomly assigned into 3 equal groups, A,B & C (N = 30 per group), according to the computer generated list. The procedure will be double blinded and the randomisation list will be maintained by the pharmacist. In the operation theatre, baseline blood pressure and pulse rate will be recorded. Intravenous access will be obtained by cannulating a peripheral vein with an 18 gauge cannula and the patient will be preloaded with ringer’s lactate solution 10 ml/kg body weight.
With aseptic precautions, under local anaesthesia, sub arachnoid block will be given by
Midline / paramedian approach
Sitting / lateral position
25 gauge lumbar puncture needle
L3 – L4 inter vertebral space
o Patients in group A will receive 2.75 ml of 0.5% heavy bupivacaine + 0.1 ml of 50% magnesium sulphate(50mg) + 0.4 ml of sterile water.
o Patients in group B will receive 2.75 ml of 0.5 % heavy bupivacaine + 150 µg of buprenorphine(0.5ml).
o Patients in group C will receive 2.75 ml of 0.5 % heavy bupivacaine + 0.5 ml of sterile water(placebo).
The total drug volume of all 3 groups will be the same (3.25ml). All injections will be made at a rate of about 1ml in 4- 5sec and solutions will be at room temperature. The drugs will be loaded by an independent colleague & both the patient and the anaesthetist will be blinded to the procedure. After injection of the drug the patient will be made supine immediately and the parameters will be observed and recorded by the anaesthetist. In patients who develop hypotension, which is defined as, fall in BP>20% of basal value or < 90mmHg of systolic BP or in the presence of symptoms like nausea , vomiting and dizziness Inj. Ephedrine 6mg will be administered intravenously. If patients develop bradycardia (Heart rate <60beats/min), Inj. Atropine 0.3mg will be given intravenously. Rescue analgesia will be given using Inj. Diclofenac 75mg or Inj. Tramadol 100mg intra muscularly if visual analogue scale score for pain is greater than 4. After completion of the study, the drug solution will be revealed to the anaesthetist.
THE PARAMETERS OBSERVED WILL BE: 1) Time of intrathecal injection. 2) Sensory blockade a. Onset of analgesia (min): defined as ~Onset of analgesia to T10. b.Duration of analgesia / sensory block: defined as ~Time to 2-segment regression. ~Time to regression of sensory block to S2. c.The maximum level of sensory block. d.Time taken for maximal level of sensory block. e.Need for rescue analgesic during surgery. 3) Motor blockade i.Estimation using Modified Bromage Scale:- ‘0-3’ 0 – No paralysis, able to flex hip, knee and ankle. 1 – Able to flex knee, unable to raise extended leg. 2 – Able to flex ankle, unable to flex knee. 3 – Unable to flex ankle, knee and hip (no movement ) ii.Time of onset of complete motor block (min) iii.Time to recovery from complete motor block. 4) Subjective assessment of quality of anaesthesia a. Quality of intraoperative motor blockade as assessed by the surgeon. b. Quality of intraoperative analgesia as assessed by the patient. 5) Duration of effective analgesia (time of intrathecal administration to the time of first analgesic request). Assessment of post operative analgesia using Visual Analogue Scale.
6) Pulse rate, arterial blood pressure and respiratory rate will be recorded every 5min for the initial 30min, every 15min thereafter and every 30min during first 6 hours of postoperative period.
7) Any other adverse effects like hypotension, bradycardia, respiratory depression, drowsiness, nausea, vomiting and pruritis.
STATISTICAL ANALYSIS
Appropriate statistical analysis of data will be done using the following tests:
1. Student t test for parametric data. 2. Chi-square test for non parametric data.
P<0.05 will be considered statistically significant. Parametric data include – Pulse rate, blood pressure, respiratory rate, time to maximum sensory block, time to 2-segment regression, time of onset of complete motor block, time to recovery from complete motor block etc. Non-parametric data include – Nausea, vomiting, pruritis etc.
7.3 DOES THIS STUDY REQUIRE ANY INVESTIGATIONS OR INTERVENTIONS TO BE CONDUCTED ON PATIENTS OR ANIMALS – SPECIFY?
No specific test or investigations are required to collect data for achieving the objectives.
7.4 HAS ETHICAL CLEARANCE BEEN OBTAINED FROM THE ETHICAL COMMITTEE OF YOUR INSTITUTION IN THE CASE OF 7.3?
Yes, ethical clearance has been obtained from the ethical committee of KIMS, Hubli. 8. LIST OF REFERENCES
1. Morrrison AP, Banerjee A, Hunter J, Mackie C, Grassman C. Systematic review of intrathecal magnesium given alone or in combination with local anaesthetics and opioids. Eur J Anaesthesiol 2001;28:109.
2. R Arcioni, S Palmisani, S Tigano, C Santorsola, V Sauli, S Romanao, et al. Combined intrathecal and epidural magnesium sulphate supplementation of spinal anesthesia to reduce post- operative analgesic requirements: A prospective, randomized, double-blind, controlled trial in patients undergoing major orthopedic surgery. Acta Anaesthesiol Scand 2007;51:482-9.
3. Woolf CJ, Thompson SW. The induction and maintenance of central sensitization is dependent on N-methyl-D-aspartic acid receptor activation: implications for the treatment of post injury pain and hypersensitivity states. Pain 1991;44:293-9.
4. Thurnau GR, Kemp DB, Jarvis A. Cerebrospinal fluid levels of magnesium in patients with preeclampsia after treatment with intravenous magnesium sulphate: a preliminary report. Am J Obstet Gynaecol 1987;157:1435-8.
5. S Ouerghi, F Fnaeich, N Frikha, T Mestiri, A Merghli, MS Mebazaa, et al. The effect of adding intrathecal magnesium sulphate to morphine-fentanyl spinal analgesia after thoracic surgery. A prospective, double-blind, placebo controlled research study. Ann Fr Anesth Reanim 2011;30:25-30.
6. S Malleeswaran, N Panda, P Mathew, R Bagga. A randomized study of magnesium sulphate as an adjuvant to intrathecal bupivacaine in patients with mild preeclampsia undergoing caesarean section. International Journal of Obstetric Anesthesia 2010;19:161-6.
7. Buvanendran A, Mc Carthy RJ, Kroin JS, Leong W, Perry P, Tuman KJ. Intrathecal magnesium prolongs fentanyl analgesia: A prospective, randomized, controlled trial. Anesth Analg 2002;95:661 -6.
8. Dayioglu H, Baykara ZN, Salbes A, Solak M, Toker K. Effects of adding magnesium to bupivacaine and fentanyl for spinal anesthesia in knee arthroscopy. J Anesth 2009;23:19-25.
9. Jong Wha Lee, Mi Kyeong Kim, Yang-Sik Shin, Bon-Nyeo Koo. The analgesic effect of single dose of intrathecal magnesium sulphate. Korean J Anesthesiol 2007;52:72-6. 9. SIGNATURE OF CANDIDATE
10. REMARKS OF THE GUIDE “ MAGNESIUM HAS MULTIPLE PHYSIOLOGICAL AND PHARMACOLOGICAL ROLES. THIS STUDY WILL HELP TO ESTABLISH ITS ROLE INTRATHECALLY FOR SPINAL ANAESTHESIA”.
11. NAME & DESIGNATION DR. MADHURI. S. KURDI M.D. PROFESSOR,DEPARTMENT 11.1 GUIDE OF ANAESTHESIOLOGY, KIMS, HUBLI.
11.2 SIGNATURE
11.3 CO-GUIDE
11.4 SIGNATURE
11.5 HEAD OF THE DR.SAFIYA SHAIKH M.D. DEPARTMENT PROFESSOR & HEAD, DEPARTMENT OF ANAESTHESIOLOGY, KIMS, HUBLI.
11.6 SIGNATURE
12. 12.1 REMARKS OF CHAIRMAN AND PRINCIPAL 12.2 SIGNATURE