06f294d2760d96a36a00a71d6946c15d.doc Page 1 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
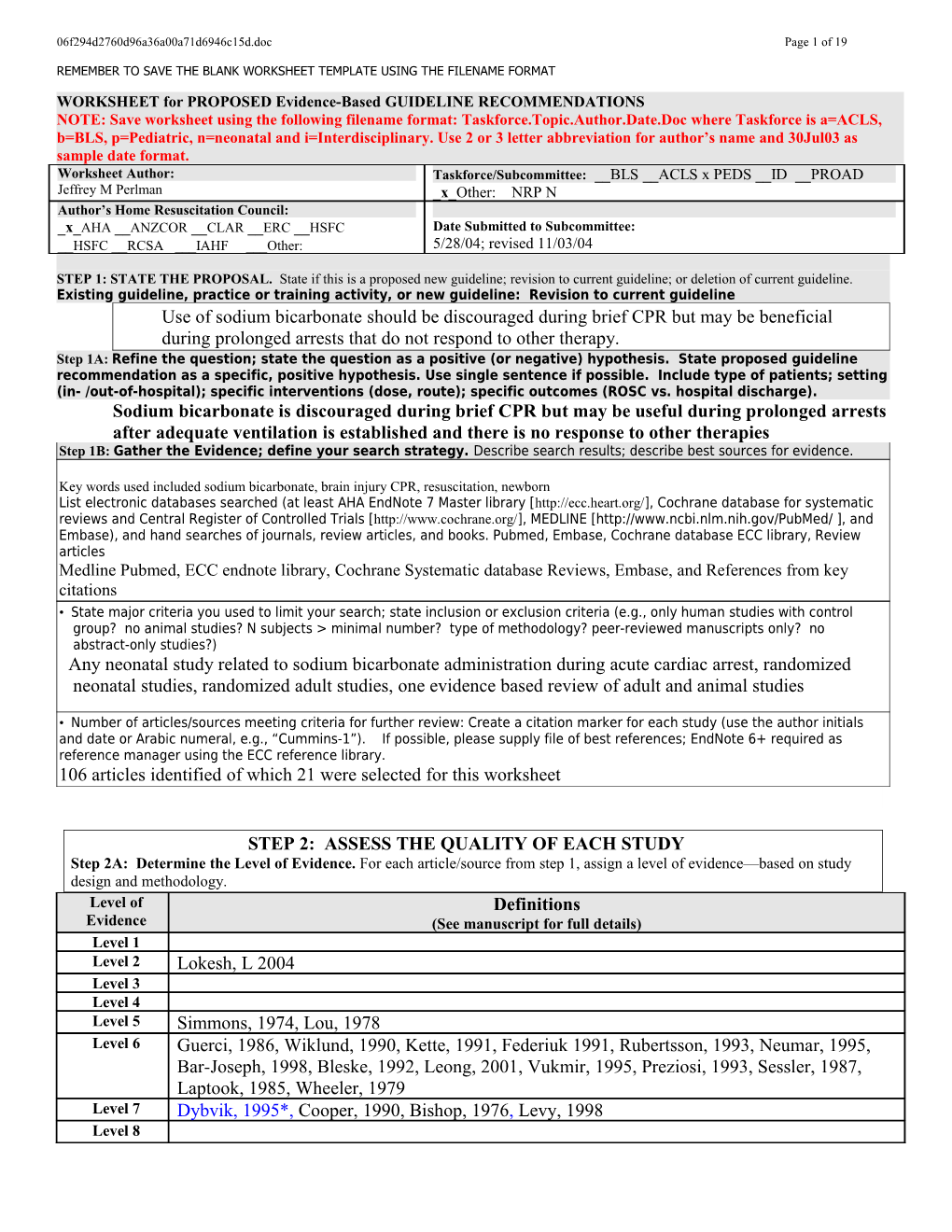
WORKSHEET for PROPOSED Evidence-Based GUIDELINE RECOMMENDATIONS NOTE: Save worksheet using the following filename format: Taskforce.Topic.Author.Date.Doc where Taskforce is a=ACLS, b=BLS, p=Pediatric, n=neonatal and i=Interdisciplinary. Use 2 or 3 letter abbreviation for author’s name and 30Jul03 as sample date format. Worksheet Author: Taskforce/Subcommittee: __BLS __ACLS x PEDS __ID __PROAD Jeffrey M Perlman _x_Other: NRP N Author’s Home Resuscitation Council: _x_AHA __ANZCOR __CLAR __ERC __HSFC Date Submitted to Subcommittee: __HSFC __RCSA ___IAHF ___Other: 5/28/04; revised 11/03/04
STEP 1: STATE THE PROPOSAL. State if this is a proposed new guideline; revision to current guideline; or deletion of current guideline. Existing guideline, practice or training activity, or new guideline: Revision to current guideline Use of sodium bicarbonate should be discouraged during brief CPR but may be beneficial during prolonged arrests that do not respond to other therapy. Step 1A: Refine the question; state the question as a positive (or negative) hypothesis. State proposed guideline recommendation as a specific, positive hypothesis. Use single sentence if possible. Include type of patients; setting (in- /out-of-hospital); specific interventions (dose, route); specific outcomes (ROSC vs. hospital discharge). Sodium bicarbonate is discouraged during brief CPR but may be useful during prolonged arrests after adequate ventilation is established and there is no response to other therapies Step 1B: Gather the Evidence; define your search strategy. Describe search results; describe best sources for evidence.
Key words used included sodium bicarbonate, brain injury CPR, resuscitation, newborn List electronic databases searched (at least AHA EndNote 7 Master library [http://ecc.heart.org/], Cochrane database for systematic reviews and Central Register of Controlled Trials [http://www.cochrane.org/], MEDLINE [http://www.ncbi.nlm.nih.gov/PubMed/ ], and Embase), and hand searches of journals, review articles, and books. Pubmed, Embase, Cochrane database ECC library, Review articles Medline Pubmed, ECC endnote library, Cochrane Systematic database Reviews, Embase, and References from key citations • State major criteria you used to limit your search; state inclusion or exclusion criteria (e.g., only human studies with control group? no animal studies? N subjects > minimal number? type of methodology? peer-reviewed manuscripts only? no abstract-only studies?) Any neonatal study related to sodium bicarbonate administration during acute cardiac arrest, randomized neonatal studies, randomized adult studies, one evidence based review of adult and animal studies
• Number of articles/sources meeting criteria for further review: Create a citation marker for each study (use the author initials and date or Arabic numeral, e.g., “Cummins-1”). . If possible, please supply file of best references; EndNote 6+ required as reference manager using the ECC reference library. 106 articles identified of which 21 were selected for this worksheet
STEP 2: ASSESS THE QUALITY OF EACH STUDY Step 2A: Determine the Level of Evidence. For each article/source from step 1, assign a level of evidence—based on study design and methodology. Level of Definitions Evidence (See manuscript for full details) Level 1 Level 2 Lokesh, L 2004 Level 3 Level 4 Level 5 Simmons, 1974, Lou, 1978 Level 6 Guerci, 1986, Wiklund, 1990, Kette, 1991, Federiuk 1991, Rubertsson, 1993, Neumar, 1995, Bar-Joseph, 1998, Bleske, 1992, Leong, 2001, Vukmir, 1995, Preziosi, 1993, Sessler, 1987, Laptook, 1985, Wheeler, 1979 Level 7 Dybvik, 1995*, Cooper, 1990, Bishop, 1976, Levy, 1998 Level 8 06f294d2760d96a36a00a71d6946c15d.doc Page 2 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT * Large Randomized study in adults
Step 2B: Critically assess each article/source in terms of research design and methods. Was the study well executed? Suggested criteria appear in the table below. Assess design and methods and provide an overall rating. Ratings apply within each Level; a Level 1 study can be excellent or poor as a clinical trial, just as a Level 6 study could be excellent or poor as an animal study. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. For more detailed explanations please see attached assessment form.
Component of Study and Rating Excellent Good Fair Poor Unsatisfactory Design & Highly appropriate Highly appropriate Adequate, Small or clearly Anecdotal, no sample or model, sample or model, design, but biased population controls, off randomized, proper randomized, proper possibly biased or model target end-points controls controls Methods AND OR OR OR OR Outstanding Outstanding accuracy, Adequate under Weakly defensible Not defensible in accuracy, precision, and data the in its class, limited its class, precision, and data collection in its class circumstances data or measures insufficient data collection in its or measures class
A = Return of spontaneous circulation C = Survival to hospital discharge E = Other endpoint B = Survival of event D = Intact neurological survival
Step 2C: Determine the direction of the results and the statistics: supportive? neutral? opposed?
DIRECTION of study by results & statistics: SUPPORT the proposal NEUTRAL OPPOSE the proposal Outcome of proposed guideline Outcome of proposed guideline Outcome of proposed guideline Results superior, to a clinically important no different from current inferior to current approach degree, to current approaches approach
Step 2D: Cross-tabulate assessed studies by a) level, b) quality and c) direction (ie, supporting or neutral/ opposing); combine and summarize. Exclude the Poor and Unsatisfactory studies. Sort the Excellent, Good, and Fair quality studies by both Level and Quality of evidence, and Direction of support in the summary grids below. Use citation marker (e.g. author/ date/source). In the Neutral or Opposing grid use bold font for Opposing studies to distinguish them from merely neutral studies. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. Supporting Evidence Sodium bicarbonate is discouraged during brief CPR but may be useful during prolonged arrests after adequate ventilation is established and there is no response to other therapies e c n e
d Excellent Dybvik, i BDE
v 1995* E
f o
y Lokesh, L Levy, t
i CDE
l 2004 1998 a Good u Q 06f294d2760d96a36a00a71d6946c15d.doc Page 3 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Guerci, 1986, Wiklund, 1990, Cooper, Fair Simmons Kette, 1991,E 1990,E 1974,E Federiuk 1991, E Bishop Lou, 1978E Rubertsson, 1976 E 1993 E, Neumar, 1995 E 1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation C = Survival to hospital discharge E = Other endpoint B = Survival of event D = Intact neurological survival Neutral or Opposing Evidence Sodium bicarbonate is discouraged during brief CPR but may be useful during prolonged arrests after adequate ventilation is established and there is no response to other therapies e c n e
d Excellent i v E
f o
y t i l Bar-Joseph, 1998A a Good ,A u Leong, 2001 AB Q Vukmir,1995
Bleske, 1992,E Preziosi, 1993,E Fair Sessler, 1987,E Laptook, 1985,E Wheeler, 1979 E 1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation C = Survival to hospital discharge E = Other endpoint B = Survival of event D = Intact neurological survival
STEP 3. DETERMINE THE CLASS OF RECOMMENDATION. Select from these summary definitions. CLASS CLINICAL DEFINITION REQUIRED LEVEL OF EVIDENCE Class I • Always acceptable, safe • One or more Level 1 studies are present (with rare Definitely recommended. Definitive, • Definitely useful exceptions) excellent evidence provides support. • Proven in both efficacy & effectiveness • Study results consistently positive and compelling • Must be used in the intended manner for proper clinical indications. Class II: • Safe, acceptable • Most evidence is positive Acceptable and useful • Clinically useful • Level 1 studies are absent, or inconsistent, or lack • Not yet confirmed definitively power • No evidence of harm • Class IIa: Acceptable and useful • Safe, acceptable • Generally higher levels of evidence Good evidence provides support • Clinically useful • Results are consistently positive • Considered treatments of choice • Class IIb: Acceptable and useful • Safe, acceptable • Generally lower or intermediate levels of evidence Fair evidence provides support • Clinically useful • Generally, but not consistently, positive results • Considered optional or alternative treatments Class III: • Unacceptable • No positive high level data Not acceptable, not useful, may be • Not useful clinically • Some studies suggest or confirm harm. harmful • May be harmful. 06f294d2760d96a36a00a71d6946c15d.doc Page 4 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
• Research just getting started. • Minimal evidence is available Indeterminate • Continuing area of research • Higher studies in progress • No recommendations until • Results inconsistent, contradictory further research • Results not compelling
STEP 3: DETERMINE THE CLASS OF RECOMMENDATION. State a Class of Recommendation for the Guideline Proposal. State either a) the intervention, and then the conditions under which the intervention is either Class I, Class IIA, IIB, etc.; or b) the condition, and then whether the intervention is Class I, Class IIA, IIB, etc. Indicate if this is a __Condition or x__Intervention Final Class of recommendation: __Class I-Definitely Recommended __Class IIa-Acceptable & Useful; good evidence _x_Class IIb-Acceptable & Useful; fair evidence __Class III – Not Useful; may be harmful __Indeterminate-minimal evidence or inconsistent
REVIEWER’S PERSPECTIVE AND POTENTIAL CONFLICTS OF INTEREST: Briefly summarize your professional background, clinical specialty, research training, AHA experience, or other relevant personal background that define your perspective on the guideline proposal. List any potential conflicts of interest involving consulting, compensation, or equity positions related to drugs, devices, or entities impacted by the guideline proposal. Disclose any research funding from involved companies or interest groups. State any relevant philosophical, religious, or cultural beliefs or longstanding disagreements with an individual. Neonatologist with 25 years of postgraduate experience. Research training in cerebral blood flow and metabolism. Have served on the Neonatal Resuscitation Program (NRP) for six years, and on the pediatric subcommittee of the AHA. I have a no potential conflict of interest.
REVIEWER’S FINAL COMMENTS AND ASSESSMENT OF BENEFIT / RISK: Summarize your final evidence integration and the rationale for the class of recommendation. Describe any mismatches between the evidence and your final Class of Recommendation. “Mismatches” refer to selection of a class of recommendation that is heavily influenced by other factors than just the evidence. For example, the evidence is strong, but implementation is difficult or expensive; evidence weak, but future definitive evidence is unlikely to be obtained. Comment on contribution of animal or mechanical model studies to your final recommendation. Are results within animal studies homogeneous? Are animal results consistent with results from human studies? What is the frequency of adverse events? What is the possibility of harm? Describe any value or utility judgments you may have made, separate from the evidence. For example, you believe evidence-supported interventions should be limited to in-hospital use because you think proper use is too difficult for pre-hospital providers. Please include relevant key figures or tables to support your assessment. The role of sodium bicarbonate during resuscitation remains controversial. There are concerns that in the absence of adequate ventilation, sodium bicarbonate administration can exacerbate intracellular hypercarbia and worsen intracellular acidosis. Moreover as a secondary consequence either directly or indirectly, there may be impaired myocardial function. In the premature infant infusion of sodium bicarbonate may result in the development of intraventricular hemorrhage (Simmons, 1974)(LOE 5). There is a small-randomized neonatal study in “asphyxiated “ term infants (low five minute Apgar score and requiring bag/mask positive pressure ventilation that failed to demonstrate any beneficial effect of sodium bicarbonate administration on neurologic outcome or survival (Lokesh, 2004)(LOE 2). There are no neonatal animal studies that have addressed the specific role of bicarbonate in achieving recovery of spontaneous circulation or survival following CPR. Tangential neonatal animal studies have noted attenuated hemodynamic responses to resuscitation with epinephrine and oxygen when concomitant acidosis was present (Preziosi, 1993)(LOE 6). However this model used a pure metabolic acidosis that is distinct from the mixed acidosis noted in the delivery room. In addition, acidosis was produced by the infusion of exogenous lactate, which may not adequately simulate acidosis derived from intracellular acid production as a result of cellular hypoxia. Additional neonatal studies suggest that bicarbonate administration increases arterial pH, brain intracellular pH and PaCO2 without producing concomitant paradoxical brain intracellular acidosis provided adequate cardiac output is maintained (Sessler, 1987 Laptook, 1985)(LOE 6). However one neonatal human study reported significant reduction in cerebral blood flow (up to 50%) following bicarbonate infusion (Lou, 1978)(LOE 5). An evidence-based review of adult human and animal studies 06f294d2760d96a36a00a71d6946c15d.doc Page 5 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT indicates that no human study has demonstrated a beneficial impact on survival and that several adult human studies (level of evidence 3 and 4) demonstrated deleterious effects on physiologic endpoints from the administration of bicarbonate during CPR (Levy, 1998). While several animal studies demonstrated impaired cardiac function in response to bicarbonate administration during CPR (Guerci, 1986, Wiklund, 1990, {Kette, 1991, Federiuk, 1991, Rubertsson, 1993, Neumar, 1995)(LOE 6) others have demonstrated survival benefit from the administration of bicarbonate during CPR (Bar Joseph 1998, Bleske, 1992 Leong, 2001Vukmir, 1995)(LOE 6). In summarizing the clinical and animal observations, given the known and potential side effects of sodium bicarbonate infusions including depression of myocardial function from the osmolar load with severe acidosis, paradoxical intracellular acidosis, reduction in cerebral blood flow and the risk for intraventricular hemorrhage, the use of sodium bicarbonate infusion should be discouraged during brief CPR, but sodium bicarbonate may be of some benefit in an infant with prolonged CPR unresponsive to other therapy including adequate ventilation.
Preliminary draft/outline/bullet points of Guidelines revision: Include points you think are important for inclusion by the person assigned to write this section. Use extra pages if necessary.
Publication: Chapter: Pages:
Topic and subheading: In one neonatal study there was no survival benefit or improvement in neurologic outcome following the use of sodium bicarbonate infusion during brief CPR (LOE 2). The administration of sodium bicarbonate has been associated with intraventricular hemorrhage and a reduction in cerebral blood flow in premature infants. (LOE 5) Sodium bicarbonate administration should be discouraged during brief CPR but may be useful during prolonged arrests after establishing adequate ventilation and there is no response to other therapies (LOE 2, 5,6,7)
Attachments: . Bibliography in electronic form using the Endnote Master Library. It is recommended that the bibliography be provided in annotated format. This will include the article abstract (if available) and any notes you would like to make providing specific comments on the quality, methodology and/or conclusions of the study. 06f294d2760d96a36a00a71d6946c15d.doc Page 6 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT Citation List
Citation Marker Full Citation* {Lokesh, 2004 #207} Lokesh L, Kumar P, Murkai S et al A randomized controlled trial of sodium bicarbonate in neonatal resuscitation-effect on immediate outcome. Resuscitation 2004 60(2): 219-23.
{Lou, 1978 #39} Lou, H. C., N. A. Lassen, et al. Decreased cerebral blood flow after administration of sodium bicarbonate in the distressed newborn infant. Acta Neurol Scand 1978 57(3): 239-47.
Simmons, M. A., E. W. Adcock, 3rd, et al. (1974). "Hypernatremia and intracranial hemorrhage in {Simmons, 1974 #44} neonates." N Engl J Med 291(1): 6-10.
Laptook, A. R. The effects of sodium bicarbonate on brain blood flow and O2 delivery during {Laptook, 1985 #37} hypoxemia and acidemia in the piglet .Pediatr Res 1985; 19(8): 815-9.
{Preziosi, 1993 #203} Preziosi, M. P., J. C. Roig, et al Metabolic acidemia with hypoxia attenuates the hemodynamic responses to epinephrine during resuscitation in lambs. Crit Care Med 1993; 21(12): 1901-7.
{Sessler, 1987 #38} Sessler, D., P. Mills, et al. Effects of bicarbonate on arterial and brain intracellular pH in neonatal rabbits recovering from hypoxic lactic acidosis. J Pediatr 1987; 111(6 Pt 1): 817-23.
{Wheeler, 1979 #201} Wheeler, A. S., S. Sadri, et al. Intracranial hemorrhage following intravenous administration of sodium bicarbonate or saline solution in the newborn lamb asphyxiated in utero Anesthesiology 1979 ; 51(6): 517-521.
{Bishop, 1976 #31 Bishop, R. L. and M. L. Weisfeldt . Sodium bicarbonate administration during cardiac arrest. Effect on arterial pH PCO2, and osmolality. Jama 1976; 235(5): 506-9.
Cooper, D. J., K. R. Walley, et al. Bicarbonate does not improve hemodynamics in critically ill {Cooper, 1990 #41} patients who have lactic acidosis. A prospective, controlled clinical study. Ann Intern Med 1990;112(7): 492-8.
{Dybvik, 1995 #204} Dybvik, T., T. Strand, et al. Buffer therapy during out-of-hospital cardiopulmonary resuscitation. Resuscitation 1995;29(2): 89-95.
{Levy, 1998 #206} Levy, M. M. An evidence-based evaluation of the use of sodium bicarbonate during cardiopulmonary resuscitation. Crit Care Clin 1998; 14(3): 457-83.
{Bar-Joseph, 1998 #36} Bar-Joseph, G., T. Weinberger, et al Comparison of sodium bicarbonate, Carbicarb, and THAM during cardiopulmonary resuscitation in dogs.Crit Care Med 1998; 26(8): 1397-408.
{Bleske, 1992 #200} Bleske, B. E., M. S. S. Chow, et al. Effects of different dosages and modes of sodium bicarbonate administration during cardiopulmonary resuscitation. American Journal of Emergency Medicine 1992;10(6): 525-532.
{Guerci, 1986 #32} Guerci, A. D., N. Chandra, et al. Failure of sodium bicarbonate to improve resuscitation from ventricular fibrillation in dogs. Circulation 1986 ; 74(6 Pt 2): IV75-9.
{Federiuk, 1991 #40} Federiuk, C. S., A. B. Sanders, et al. The effect of bicarbonate on resuscitation from cardiac arrest. Ann Emerg Med 1991; 20(11): 1173-7.
{Kette, 1991 #33} Kette, F., M. H. Weil, et al. Buffer solutions may compromise cardiac resuscitation by reducing coronary perfusion pressure. Jama 1991; 266(15): 2121-6. 06f294d2760d96a36a00a71d6946c15d.doc Page 7 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
{Leong, 2001 #197} Leong, E. C. M., J. C. Bendall, et al. Sodium bicarbonate improves the chance of resuscitation after 10 minutes of cardiac arrest in dogs. Resuscitation 2001; 51(3): 309-315.
{Neumar, 1995 #35} Neumar, R. W., N. G. Bircher, et al. Epinephrine and sodium bicarbonate during CPR following asphyxial cardiac arrest in rats. Resuscitation 1995; 29(3): 249-63.
{Rubertsson, 1993 #34} Rubertsson, S. and L. Wiklund . Hemodynamic effects of epinephrine in combination with different alkaline buffers during experimental, open-chest, cardiopulmonary resuscitation. Crit Care Med1993;21(7): 1051-7.
Vukmir, R. B., N. G. Bircher, et al. Sodium bicarbonate may improve outcome in dogs with brief or {Vukmir, 1995 #199} prolonged cardiac arrest. Critical Care Medicine 1995; 23(3): 515-522.
Wiklund, L., G. Ronquist, et al. Effects of alkaline buffer administration on survival and {Wiklund, 1990 #43} myocardial energy metabolism in pigs subjected to ventricular fibrillation and closed chest CPR. Acta Anaesthesiol Scand 1990;34(6): 430-9.
*Type the citation marker in the first field and then paste the full citation into the second field. You can copy the full citation from EndNote by selecting the citation, then copying the FORMATTED citation using the short cut, Ctrl-K. After you copy the citation, go back to this document and position the cursor in the field, then paste the citation into the document (use Ctrl-V). For each new citation press Tab to move down to start a new field. 06f294d2760d96a36a00a71d6946c15d.doc Page 8 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT Neonatal Clinical Studies
* Lokesh, L.Kumar, P.Murki, S.Narang, A. A randomized controlled trial of sodium bicarbonate in neonatal resuscitation--effect on immediate outcome. Resuscitation 2004;60:219-223
Very little evidence is available that supports or disproves the use of medications in neonatal resuscitation. In this randomized controlled trial, we evaluated the effect of sodium bicarbonate given during neonatal resuscitation, on survival and neurological outcome at discharge. Subjects and methods: Consecutively born asphyxiated neonates continuing to need positive pressure ventilation at 5 min of life received either sodium bicarbonate or 5% dextrose. The study group was given intravenous sodium bicarbonate solution 4 ml/kg (1.8 meq/kg) over 3–5 min. This solution was prepared by diluting 7.5% sodium bicarbonate (0.9 meq/ml) with distilled water in a 1:1 ratio. The placebo group received 4 ml/kg of undiluted 5% dextrose at a similar rate. The surviving neonates were evaluated for their neurological status at discharge. Primary outcome variable: Death or abnormal neurological examination at discharge. Secondary outcome variables: Encephalopathy, multi-organ dysfunction, intraventricular haemorrhage (IVH) and arterial pH at 6 h. Results: Twenty-seven babies were randomized to receive sodium bicarbonate (bicarb group) and 28 to receive 5% dextrose. Eighteen of the 27 (66.7%) babies in the bicarb group and 19 of the 28 babies (68%) in the dextrose group survived to discharge (P=0.84). Twenty-eight percent of the survivors in the bicarb group and 32% of the survivors in the dextrose group were neurologically abnormal at discharge (P=0.10). The composite primary outcome of death or abnormal neurological examination at discharge was similar in both groups (52% versus 54%, P=0.88). The incidence of encephalopathy (74% versus 63%), cerebral oedema (52% versus 30%), need for inotropic support (44% versus 29%), intraventricular haemorrhage (IVH) and the mean arterial pH at 6hrs were similar between the two groups. Conclusion: Administration of sodium bicarbonate during neonatal resuscitation did not help to improve survival or immediate neurological outcome
Comment Small randomized study that shows no benefit to the administration of sodium bicarbonate during resuscitation of the largely premature infant. Level of Evidence 2 Quality Good Evidence- supportive
Lou, H. C. Lassen, N. A. Fris-Hansen, B Decreased cerebral blood flow after administration of sodium bicarbonate in the distressed newborn infant Acta Neurol Scand 1978; 57:239-247
Contents Methods In the course of studies on cerebral blood flow in newborn infants the effect of sodium bicarbonate infusion on cerebral blood flow was noted. Cerebral blood flow was measured utilizing the 133 Xe clearance technique before and after the treatment with 1 to 8 meqs of sodium bicarbonate in seven distressed newborn infants. Results In six of the seven cases a decrease in cerebral blood flow was noted , which in most cases range of reduction was 14 to 22 ml/100 g/min, which is about half the value prior to the bicarbonate infusion. In one case an extreme reduction occurred: cerebral blood flow was reduced to 3 ml/100 g/min, well below the level compatible with tissue survival. Comments. The reduction in CBF may be secondary to bicarbonate induced cerebral vasoconstriction. No blood pressure values were provided pre and post infusion. The clinical implications of these observations are unclear since alkalosis may cause systemic vasodilation and reduce ionized calcium concentrations, which may adversely affect cardiac contractility. Level of Evidence 5 06f294d2760d96a36a00a71d6946c15d.doc Page 9 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT Quality Fair Evidence - Supportive
Simmons, M. A.Adcock, E. W., 3rd Bard, H. Battaglia, F. C. Hypernatremia and intracranial hemorrhage in neonates N Engl J Med 1974;291: 6-10
Methods Retrospective chart review. The charts of infants admitted over 4 years to a neonatal intensive care unit were reviewed. The diagnosis of intracranial hemorrhage was made at autopsy in all but one case. Intracranial hemorrhage was associated with hypernatremia or excessive sodium administration in 25(81%) of the 32 cases. Following restrictive use of sodium bicarbonate, the incidence of hypernatremia decreased from 8.8 to 0.6% and the frequency of IVH declined from 13.4% to 2.6%.
Comments: The retrospective nature of the study in addition to establishing a diagnosis at autopsy precludes any definitive conclusions to be inferred from this data other than the association between two events. Level of Evidence 5 Quality Fair Evidence- supportive
Neonatal Animal Studies
Laptook, A. R. The effects of sodium bicarbonate on brain blood flow and O2 delivery during hypoxemia and acidemia in the piglet Pediatr Res 1985;19: 815-9
Metabolic acidosis in the neonate is often secondary to hypoxemia and cardiopulmonary disturbances. Sodium bicarbonate, an agent used to treat metabolic acidemia in newborns, is often administered during hypoxemia. In the absence of acid-base alterations, during hypoxemia a reciprocal relationship exists between arterial O2 content (CaO2) and brain blood flow (BBF). However, when hypoxemia is compounded by acidemia it is unclear whether the increase in arterial pH achieved by infusions of sodium bicarbonate alters BBF. Methods BBF (microsphere technique), arterial blood gases, and CaO2 were measured in 14 ventilated piglets. Variables were assessed during a control period, a period of hypoxemia (50 min) associated with metabolic acidemia (hypoxemia + acidemia), and after infusions of either saline (n = 6) or NaHCO3 (n = 8, 2 mEq/kg) during continued hypoxemia. Results Arterial pH was similar in both groups at control, and hypoxemia + acidemia resulted in comparable reductions of pH in both saline- and NaHCO3-treated piglets (7.21 +/- 0.02 versus 7.21 +/- 0.03, respectively). NaHCO3 infusions produced a significant rise in pH, 7.30 +/- 0.03 versus 7.15 +/- 0.03, p less than 0.05. In each group CaO2 paralleled changes in pH but did not differ between groups. In all animals BBF increased more than 2-fold during hypoxemia + acidemia and was unaltered by infusions of either saline or NaHCO3. Brain O2 delivery decreased in both groups during hypoxemia + acidemia and was unchanged by infusions of saline or NaHCO3. Conclusion During hypoxemia + acidemia the change in arterial pH induced by NaHCO3 (2 mEq/kg) does not alter BBF or brain O2 delivery.
Comment- Correction of metabolic acidosis does not appear to alter brain blood flow or oxygen delivery Level of Evidence 6 Quality Good Evidence -supportive
Preziosi, M. P.Roig, J. C.Hargrove, N. Burchfield, D. J. Metabolic acidemia with hypoxia attenuates the hemodynamic responses to epinephrine during resuscitation in lambs Crit Care Med 1993;21:1901-1907 06f294d2760d96a36a00a71d6946c15d.doc Page 10 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT OBJECTIVE: To examine the effects of metabolic acidemia and hypoxia on the hemodynamic responses to epinephrine in an intact neonatal animal model. Methods Multi-experiment, randomized, controlled trial. Sixteen lambs, ranging in age from 2 to 14 days were chronically catheterized; the ductus arteriosus was ligated; and a pulmonary arterial flow probe was inserted to measure cardiac output, blood pressure (BP), and heart rate. In the first protocol, hemodynamic responses to epinephrine during pure metabolic acidemia or metabolic alkalosis were studied in eight lambs. Each lamb was studied on four different days at a different arterial pH: 6.9, 7.1, 7.4, and 7.6. Ventilation was controlled to maintain PCO2 at 35 to 45 torr (4.66 to 5.99 kPa). Acidemia was induced by the infusion of lactic acid and alkalosis by the infusion of sodium bicarbonate. When the appropriate arterial pH was achieved, 10 micrograms/kg of epinephrine was administered intravenously. In a second protocol, hemodynamic responses to epinephrine during metabolic acidemia or alkalosis plus hypoxia were studied in eight lambs. When the appropriate arterial pH was achieved, hypoxia was induced until cardiac output decreased to 40% of baseline. Epinephrine bolus was given, and after 90 secs, lambs were resuscitated with O2 . RESULTS: Epinephrine administered during uncompromised hemodynamics led to hypertension, bradycardia, and decreased cardiac output that were unaffected by arterial pH values between 6.9 and 7.6. Acidemia with hypoxia compromised hemodynamics with decreases in heart rate and cardiac output. Epinephrine administered during this compromised condition did not improve cardiac output, heart rate, or BP before resuscitation with oxygen at any arterial pH studied. Resuscitation with epinephrine and oxygen during hemodynamically compromised states led to increases in heart rate, BP, and cardiac output with significant attenuation of these hemodynamic responses during metabolic acidemia at pH values of 6.9 and 7.1. CONCLUSIONS: During the physiologic conditions associated with neonatal resuscitation, that is, hypoxia with a compromised hemodynamic state, metabolic acidemia significantly attenuates the hemodynamic responses to resuscitation with epinephrine and oxygen. Correction of metabolic acidosis may be warranted in newborn resuscitation Comment Positive effect of correcting acidosis demonstrated on cardiovascular status. Note the PCO2 was maintained 35 to 45mmHg and acidosis induced with lactic acid infusion which may not simulate the physiology of lactic acidosis derived from hypoxic/ischemic cells. . Level of Evidence 6 Quality Fair Evidence- Neutral to opposing
Sessler, D.Mills, P.Gregory, G.Litt, L.James, T. Effects of bicarbonate on arterial and brain intracellular pH in neonatal rabbits recovering from hypoxic lactic acidosis J Pediatr 1987;111:817-823
Objective To determine whether administration of a neutralizing dose of bicarbonate in rabbits with lactic acidosis caused a paradoxical brain intracellular acidosis as measured by 31P spectroscopy. Methods Ten 10- to 16-day-old rabbits were anesthetized with 0.75% halothane/oxygen and their lungs mechanically ventilated. Metabolic acidosis was induced by decreasing PaO2 to 25 to 35 mm Hg for 1 to 2 hours until the base deficit was 10 to 15 mEq/L. Cerebral ischemia was prevented by maintaining arterial blood pressure at +/- 20% of control value with a venous infusion of epinephrine. Hypoxia was then terminated by administration of 100% oxygen, which was continued for the remainder of the study. After 15 minutes 100% oxygen, 5 mEq/kg 4.2% bicarbonate was administered to five animals; 5 minutes later the same dose was repeated. Control rabbits were given equal volumes of saline solution. Results In all animals, arterial pH decreased from 7.43 +/- 0.06 to 7.25 +/- 0.08 (SE) during hypoxia, and brain intracellular pH from 7.22 +/- 0.06 to 7.09 +/- 0.09 (SE). Both pH values remained low during reoxygenation. Bicarbonate administration normalized arterial pH (7.41 +/- 0.03), whereas 06f294d2760d96a36a00a71d6946c15d.doc Page 11 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT treatment with saline solution did not (7.23 +/- 0.01, P less than 0.05). PaCO2 rapidly increased by 10 mm Hg in the bicarbonate group, and remained elevated; it was unaffected by saline solution administration. Brain intracellular pH in the bicarbonate group increased by 0.12 U over 40 minutes, but intracellular pH in the saline solution group decreased 0.05 pH U (P less than 0.05) over the same period. Comments Sodium bicarbonate infusion increased control pH, PCO2, as well as increasing brain intracellular pH. The so called “paradoxical intracellular acidosis did not occur, however bicarbonate was infused while maintaining adequate perfusion and ventilation. Level of Evidence 6- Quality Good Evidence- Neutral to opposing
Wheeler, A. S. Sadri, S. Gutsche, B. B. et al. Intracranial hemorrhage following intravenous administration of sodium bicarbonate or saline solution in the newborn lamb asphyxiated in utero Anesthesiology 1979;51: 517-521
Background The effects of intravenously administered sodium bicarbonate was studied in near-term neonatal lambs asphyxiated in utero induced by maternal hypotension. Methods Following tracheal intubation and manual ventilation with 100 per cent oxygen, the extracellular base deficits of ten neonates were corrected with sodium bicarbonate, 4.2 per cent, in 5 per cent dextrose (964 mOsm/l). Nine neonates alternatively received an isovolumic infusion of physiologic saline solution, 0.5 per cent, in 2.5 per cent dextrose (314 mOsm/l). Results Following sodium bicarbonate infusion (mean dose 6.7 mEq/kg), serum sodium and osmolality immediately increased to 160 mEq/l and 335 mOsm/l, respectively. However, sodium values were similar in the two groups by 15 min after infusion. Although significant differences in PA(O2) values were not found between groups after infusion, sodium bicarbonate therapy was associated with a significantly higher PA(O2) value (175 +/- 60 torr) than was treatment with saline solution (51 +/- 8 torr) in neonates with pH(a)<7.00 before resuscitation. Significant disparities in pH(a) and base excess values occurred between bicarbonate- and saline-treated groups after infusion; two saline-treated lambs died, while all bicarbonate treated lambs survived the study period. Intracranial subarchnoid hemorrhage occurred in three bicarbonate- and in two saline-treated lambs and was apparently related to severe asphyxia and not to the tonicity of the solutions. Conclusion Treatment of neonatal metabolic acidosis with appropriate doses of sodium bicarbonate is not associated with intracranial hemorrhage or sustained hypernatremia in the term neonatal lamb.
Comments Neonatal animal study that does not demonstrate a relationship to IVH. However the sheep model is distinctly different from the premature infant with a germinal matrix. Level of Evidence 6 Quality Good Evidence - Neutral
Adult Clinical Studies
Bishop, R. L.Weisfeldt, M. L Sodium bicarbonate administration during cardiac arrest. Effect on arterial pH, PCO2, and osmolality JAMA 1976;235:506-509 Contents Both adult and animal data Methods Adult patient (n=6) received sodium bicarbonate infusion infusion and the blood was sampled. 06f294d2760d96a36a00a71d6946c15d.doc Page 12 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT Results: The administration of sodium bicarbonate was associated with an increase in pH from 7.38 0.05 to 7.480.06, an increase in PaCO2 from 272.7 to 4910mmHg and an increase in serum osmolarity from 309 mOsm/kg to 349 mOsm/kg (all p <0.01) within two minutes. In control animals the pH decreased from 7.470.02 to 7.220.02 and the PCO2 decreased from 323.9 to 226mmHg Methods 16 mongrel dogs subjected to VF and chest compressions initiated within three minutes were resuscitated with sodium bicarbonate 1mg/kg (n=9) and without (n=7) administered over 15 minutes. Results Sodium bicarbonate infusion was associated with an increase in pH from 7.23 0.07 to 7.480.07, an increase in PaCO2 from 241.8 to 38.82.9mmHg and an increase in serum osmolarity from 308 mOsm/kg to 343 mOsm/kg Comments These studies demonstrate that (1) in the absence of preexisting acidosis, severe acidosis can be prevented by adequate ventilation alone; (2) sodium bicarbonate administration results in a significant rise in arterial PCO2, which parallels the rise in pH despite adequate ventilation; (3) during prolonged cardiac resuscitation, there is a rise in arterial osmolality that is accentuated by sodium bicarbonate. Furthermore these studies suggest that sodium bicarbonate should not be used during resuscitation (1) in the absence of effective hyperventilation or where carbon dioxide removal is inadequate despite adequate ventilation, (2) in repeated doses, without confirmation of substantial acidosis, or (3) when cardiac arrest has been of brief duration and preexisting acidosis is unlikely. Level of Evidence 7- Quality Fair Evidence- supportive
Cooper, D. J.Walley, K. R.Wiggs, B. R.Russell, J. A. Bicarbonate does not improve hemodynamics in critically ill patients who have lactic acidosis. A prospective, controlled clinical study Ann Intern Med 1990;42:492-498
Methods Prospective, randomized, blinded, crossover study. Fourteen adult patients who had metabolic acidosis (bicarbonate less than 17 mmol/L and base excess less than -10) and increased arterial lactate (mean, 7.8 mmol/L) received equimolar sodium bicarbonate and sodium chloride. . All had pulmonary artery catheters and 13 were receiving catecholamines. Results: Sodium bicarbonate (2 mmol/kg body weight over 15 minutes) increased arterial pH (7.22 to 7.36, P < 0.001), serum bicarbonate (12 to 18 mmol/L, P < 0.001), and partial pressure of CO2 in arterial blood (PaCO2) (35 to 40 mm Hg, P < 0.001) and decreased plasma ionized calcium (0.95 to 0.87 mmol/L, P < 0.001). Comparable changes in pulmonary capillary wedge pressure and cardia output was noted following infusion of both solutions. Conclusions: Correction of acidemia using sodium bicarbonate does not improve hemodynamics in critically ill patients who have metabolic acidosis and increased blood lactate. Moreover, sodium bicarbonate administration did not improve the cardiovascular response to infused catecholamines in these patients. Sodium bicarbonate increased PaCO2
Comments: Small study. Strengths include randomized blinded and crossover. Level of Evidence 7 Quality Good Evidence - supportive
* Dybvik, T.Strand, T.Steen, P. A Buffer therapy during out-of-hospital cardiopulmonary resuscitation. Resuscitation 1995;29:89-95 06f294d2760d96a36a00a71d6946c15d.doc Page 13 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT Background The effects of infusing a buffer solution on successful resuscitation and outcome was tested in patients during out-of-hospital cardiac arrest. Methods A number (502) of adults with asystole or ventricular fibrillation with failure of first defibrillation attempt were entered into a prospective, randomized, double-blind, controlled trial. Of these, 245 patients received 250 ml of sodium bicarbonate-trometamol- phosphate mixture with buffering capacity 500 mmol/l and 257 patients received 250 ml 0.9% saline. Except for the investigational infusion, all patients were resuscitated according to international guidelines. Results Eighty-seven patients (36%) receiving buffer were admitted to hospital ICU and 24 (10%) were discharged from hospital alive, vs. 92 (36%) and 35 (14%) receiving saline (95% confidence interval (CI) for difference between groups: -6%-6% for rate of admission and -1%-9% for rate of discharge). Using a logistic regression analysis, ventricular fibrillation as initial rhythm (odds ratio 8.06, CI 3.70-17.56) improved the outcome, whereas buffer therapy had no effect (odds ratio 0.77, CI 0.43-1.41). Mean base excess at hospital admission was -9 after Tribonat vs. -11 after saline (P = 0.04, CI for difference 0.2-3.8). Only 16 of the 502 patients had arterial alkalosis on arrival in the hospital and no patient had a positive base excess. Conclusion Patients resuscitated after out-of-hospital cardiac arrest had metabolic acidosis, but buffer therapy did not improve the outcome
Comments Randomized adult study of bicarbonate versus saline in asystolic out of hospital patient of whom one third in both groups were admitted to the ICU. Logistic modeling showed no improvement in outcome with buffer therapy. This is the only human randomized study addressing this specific question.
Level of Evidence 7- Quality Excellent Evidence -supportive
Evidenced Based Review of Adult Clinical and Experimental Studies
* Levy, M. M. An evidence-based evaluation of the use of sodium bicarbonate during cardiopulmonary resuscitation. Crit Care Clin 14(3): 457-83.
This was an evidence based review that addressed the following question: what evidence supports the use of sodium bicarbonate in the therapy of acidosis associated with cardiac arrest during CPR Human studies (n=21) Only one study Dybvik, T., T et al was prospective. As noted above, this study did not demonstrate a beneficial effect of buffer on ROSC or outcome after out of hospital cardiac arrest. (It was suggested that the study was underpowered and that it would take 4200 patients to show a difference.) None of the retrospective studies showed any benefit, eight studies suggested a deleterious effect and 12 studies showed no difference in outcome following cardiac arrest.
There were 38 adult animal studies. With regard to outcome 4 showed improved survival and 7 showed no difference. Regarding myocardial performance, none showed benefit, 12 were deleterious and 2 showed no difference.
The author’s conclusions included the following: 1) No human study has demonstrated a beneficial impact of sodium bicarbonate on survival 2) Several adult human studies (level 3 and 4) have demonstrated deleterious effects on physiologic end points from the administration of bicarbonate during CPR 06f294d2760d96a36a00a71d6946c15d.doc Page 14 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT 3) Several animal studies have demonstrated impaired function in response to bicarbonate administration during CPR 4) Several animal studies (n=4) have demonstrated survival benefit from the administration of bicarbonate during CPR
Level of Evidence 8 Quality Excellent Evidence- supportive
Adult Animal Studies Bar-Joseph, G., T. Weinberger, et al. Comparison of sodium bicarbonate, Carbicab and THAM during cardiopulmonary resuscitation in dogs. 1998 Crit Care Med 26: 1397-408.
Objectives: To evaluate the effects of CO2 producing and non-CO2 producing buffers in a canine model of prolonged ventricular fibrillation followed by effective CPR. Methods Prospective, randomized, controlled, blinded trial involving adult dogs (n=38). VF was electrically induced, and after 10 mins, CPR was initiated, including ventilation with an FIO2 of 1.0, manual chest compressions, administration of epinephrine (0.1 mg/kg every 5 mins), and defibrillation. A dose of buffer, equivalent to 1 mmol/kg of NaHCO3, was administered every 10 mins from start of CPR. Animals were randomized to receive either NaHCO3, Carbicarb, THAM, or 0.9% sodium chloride (NaCl). CPR was continued for up to 40 mins or until return of spontaneous circulation. Results; Buffer-treated animals had a higher resuscitability rate compared with NaCl controls. Spontaneous circulation returned earlier and at a significantly higher rate after NaHCO3 (7/9 dogs), and after Carbicarb (6/10 dogs) compared with NaCl controls (2/10 dogs). Spontaneous circulation was achieved twice as fast after NaHCO3 compared with NaCl (14.6 vs. 28 mins, respectively). Hydrogen ion (H+) concentration and base excess, obtained 2 mins after the first buffer dose, were the best predictors of resuscitability. Arterial and mixed venous Pco2 did not increase after NaHCO3 or Carbicarb compared with NaCl. Comments Buffer therapy promoted successful resuscitation after prolonged cardiac arrest, regardless of coronary perfusion pressure. NaHCO3, and to a lesser degree, Carbicarb, was beneficial in promoting early return of spontaneous circulation. When epinephrine was used to promote tissue perfusion, there was no evidence for hypercarbic venous acidosis associated with the use of these CO2 generating buffers. This study demonstrated a positive benefit of sodium bicarbonate therapy
Level of Evidence 6 Quality Very Good Evidence -opposing
Bleske, B. E., M. S. S. Chow, et al. Effects of different dosages and modes of sodium bicarbonate administration during cardiopulmonary resuscitation. American Journal of Emergency Medicine 1992 10: 525-532.
Objectives To investigate the effect of different modes of sodium bicarbonate administration on blood gas parameters during CPR. Methods Adults dogs (n=36) were subjected to unassisted VF followed 10 minutes of CPR. Following 1 minute of CPR, the animals received one of four treatments in a randomized and blinded manner: normal saline (NS) (n=11), sodium bicarbonate bolus dose 1 mEq/kg (n=8) , sodium 06f294d2760d96a36a00a71d6946c15d.doc Page 15 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT bicarbonate continuous infusion 0.1 mEq/kg/min (n=8)(I), and sodium bicarbonate bolus dose (0.5 mEq/kg) plus continuous infusion 0.1 mEq/kg/min (n=9)(L + I). Results Following NS infusion, both arterial and venous pH declined consistently over time. Bolus NAHCO3 infusion had an elevated venous PCO2 (mm Hg) concentration following 6 minutes of ventricular fibrillation compared with NS, bolus and continuous NAHCO3 and continuous NAHCO3 groups (81 +/- 14 versus 69 +/- 10 versus 68 +/- 10 versus 71 +/- 8, respectively, (P = .07). Arterial pH and PCO2 values showed a similar trend as the venous data Comments These observations suggest that if administration of sodium bicarbonate was contemplated a continuous infusion may be the most desirable mode of administration for the prevention of venous acidosis during CPR Level of Evidence 6 Quality Good Evidence - neutral
Guerci, A. D.Chandra, N.Johnson, E. et al Failure of sodium bicarbonate to improve resuscitation from ventricular fibrillation in dogs Circulation 1986;74(Suppl IV) 75-79
Objective To determine the value of sodium bicarbonate in resuscitation from ventricular fibrillation and the prevention of spontaneous refibrillation. Methods Randomized placebo controlled study. Adult dogs (n=16) were administered sodium bicarbonate (1 meq/kg) or placebo 18 min after the induction of ventricular fibrillation and cardiopulmonary resuscitation. Defibrillation was attempted 2 min after the administration of bicarbonate or placebo. Results All animals were successfully defibrillated, but three of eight bicarbonate-treated and two of eight control animals died in electromechanical dissociation (p = NS). Spontaneous refibrillation occurred in three animals in each group (p = NS). Successful resuscitation was not dependent on treatment, arterial or mixed venous PCO2, or arterial or mixed venous pH but correlated strongly with coronary perfusion pressure (p < .003).
Comments The data do not suggest a primary role for sodium bicarbonate in resuscitation following ventricular fibrillation in adult dogs. The relevance to the neonate who presents with bradycardia is unclear. Level of Evidence 6 Quality Fair Evidence –supportive
Federiuk, C. S. Sanders, A. B. Kern, K. B et al The effect of bicarbonate on resuscitation from cardiac arrest Ann Emerg Med 1991;20: 1173-77
Objective To determine the effect of bicarbonate administration on resuscitation in a porcine model of prolonged cardiac arrest. Methods Adult pigs (m=26) were subjected to ventricular fibrillation for 15 minutes (16 animals) or 20 minutes (ten animals) with no resuscitative efforts. Resuscitation attempts with open-chest cardiac massage and epinephrine were used in all animals after the arrest period. The experimental group was given sodium bicarbonate (3 mEq/kg), and the control group received 3% saline (5 mL/kg) at the initiation of cardiac massage. Results : There was no difference in resuscitation rates between bicarbonate and nonbicarbonate- treated swinei.e. 6/8 bicarbonate-treated swine were resuscitated successfully compared with 5/8 06f294d2760d96a36a00a71d6946c15d.doc Page 16 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT hypertonic saline-treated animals. There was no difference in systolic or diastolic blood pressures or myocardial perfusion pressure between the bicarbonate and hypertonic saline-treated animals.
Comments The use of sodium bicarbonate did not improve resuscitation from prolonged cardiac arrest Level of Evidence 6 Quality Fair Evidence- supportive
Kette, F.Weil, M. H.Gazmuri, R. J. Buffer solutions may compromise cardiac resuscitation by reducing coronary perfusion pressure JAMA 1991;266:2121-6
Objective To compare the infusion of sodium bicarbonate, Carbicarb and sodium chloride infusion on cardiac hemodynamics.. Methods Adult pigs (n=44) had cardiac arrest induced by ventricular fibrillation. Precordial compression was started at the third minute of untreated ventricular fibrillation and maintained for an interval of 8 minutes. A hypertonic solution of sodium bicarbonate, Carbicarb or an isotonic solution of sodium chloride was infused into the right atrium over a 1-minute interval starting at the sixth minute of ventricular fibrillation. Results Infusion of hypertonic buffer and sodium chloride solutions increased plasma osmolality from an average of 280 to 330 mOsm/kg. This was accompanied by a significant decrease in the aortic pressures and CPPs generated during precordial compression. No such changes occurred after infusion of isotonic sodium chloride
Comments Sodium bicarbonate solution in the absence of vasopressor agents may adversely affect cardiac resuscitation by reducing the coronary perfusion pressure below critical thresholds. Level of Evidence 6 Quality Good Evidence-supportive
Leong, E. C. M., J. C. Bendall, et al. Sodium bicarbonate improves the chance of resuscitation after 10 minutes of cardiac arrest in dogs. Resuscitation 2001; 51: 309-315. Objective To determine whether administration of sodium bicarbonate and/or adrenaline in combination with a brief period of cardiopulmonary resuscitation (CPR) prior to defibrillation would improve the outcome of prolonged cardiac arrest in dogs. Methods VF was induced and after 10 min of VF, animals(n=24) received either immediate defibrillation (followed by treatment with bicarbonate or control) or immediate treatment with bicarbonate or saline (followed by defibrillation). Results Treatment with bicarbonate was associated with increased rates of restoration of spontaneous circulation. This was achieved with fewer shocks and in a shorter time. Coronary perfusion pressure was significantly higher in NaHCO treated animals than in control animals. The best outcome in this study was achieved when defibrillation was delayed for approximately 2 min, during which time NaHCO and adrenaline were administered with CPR.
Comments These data suggest that following prolonged arrest bicarbonate therapy and a period of perfusion prior to defibrillation may increase survival. However longer-term outcome and in particular CNS outcome is not provided. There is biochemical, histological and clinical evidence that the cumulative energy dose delivered to the myocardium during defibrillation attempts is associated with 06f294d2760d96a36a00a71d6946c15d.doc Page 17 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT myocardial damage, which decreases the likelihood of successful resuscitation. This is not a concern to the neonatal population. Level of Evidence 6 Quality Good Evidence – neutral to opposing
Neumar, R. W., N. G. Bircher, et al. Epinephrine and sodium bicarbonate during CPR following asphyxial cardiac arrest in rats. Resuscitation 1995; 29: 249-63.
Objective To determine the impact of EPI and NaHCO3 given during CPR on long term outcome. Methods Sprague-Dawley rats (n=100) were prospectively studied in a block randomized placebo controlled trial. Each rat underwent 10 min of asphyxia, resulting in 6.8 +/- 0.4 min of circulatory arrest. Resuscitation was performed by mechanical ventilation and manual external chest compressions. EPI 0.0 (placebo), 0.01, 0.1, or 1.0 mg/kg IV was given at the onset of CPR, followed by NaHCO3 0.0 (placebo) or 1.0 mEq/kg IV. Neurologic deficit scores (NDS), cerebral histopathologic damage scores (CHDS) and myocardial histopathologic damage scores (MHDS) were determined in rats that survived 72 h. Results EPI improved CoPP and ROSC in a dose-dependent manner up to 0.1 mg/kg. Rats receiving EPI 0.1 and 1.0 mg/kg during CPR exhibited prolonged post-ROSC hypertension and metabolic acidemia, increased A-a O2 gradient, and an increased incidence of post-ROSC ventricular tachycardia or fibrillation. Overall survival was lower with EPI 0.1 and 1.0 mg/kg compared to 0.01 mg/kg. Although NDS was significantly less with EPI 0.1 mg/kg compared to placebo, there was no difference in CHDS between groups. In contrast, MDS was significantly higher with EPI 0.1 mg/kg compared to placebo or EPI 0.01 mg/kg. There was an overall trend toward improved survival at 72 h in rats that received NaHCO3, which was most evident in the EPI 0.1 mg/kg group. Comments EPI during CPR has a biphasic dose/response curve in terms of survival, when post- resuscitation effects are left untreated. Thus high dose epinephrine was associated with ROSC hypertension and acidemia and ventricular tachycardia that appears to be attenuated with sodium bicarbonate. Thus administration of sodium bicarbonate when high dose EPI is used may help to counter some of epinephrine’s systemic side effects. It is noteworthy that sodium bicarbonate did not affect histology in any of the groups studied. Level of Evidence 6 Quality Good Evidence- Neutral
Rubertsson, S. Wiklund, L. Hemodynamic effects of epinephrine in combination with different alkaline buffers during experimental, open-chest, cardiopulmonary resuscitation. Crit Care Med 1993; 21: 1051-57
OBJECTIVE: To evaluate the hemodynamic actions of epinephrine combined with different alkaline buffers during experimental, open-chest, cardiopulmonary resuscitation (CPR). DESIGN: Prospective, randomized, controlled trial. SETTING: Experimental animal laboratory in a university hospital. SUBJECTS: A total of 28 anesthetized piglets. INTERVENTIONS: After catheterization and application of a pulmonary artery flow probe (transit-time ultrasound flowmetry), the animals were stabilized. Induction of ventricular fibrillation was followed by a 15-min period of CPR, including manual heart compressions and mechanical ventilation with pure oxygen. On commencement of CPR, a 4-min alkaline buffer infusion began, with 50 mmol of sodium bicarbonate (n = 7), tris buffer mixture (n = 7), or tris buffer (n = 7), or, as a control (n = 7), the same volume of normal saline. After 8 mins of CPR, 0.5 mg of epinephrine was given intravenously; after 15 mins, direct current shocks were used to 06f294d2760d96a36a00a71d6946c15d.doc Page 18 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT revert the heart to sinus rhythm. MEASUREMENTS AND MAIN RESULTS: Blood flow measured in the pulmonary artery during open-chest CPR was approximately 20% of normal cardiac output. Administration of epinephrine reduced pulmonary artery flow irrespective of buffer. Sodium bicarbonate alone resulted in higher systemic blood pressure than pure tris: tris buffer mixture and normal saline were intermediate. Sodium bicarbonate combined with epinephrine tended to produce lower systemic blood pressure than other combinations. CONCLUSIONS: Experimental open-chest CPR generates pulmonary artery blood flows (20% of normal cardiac output) that are at best at the lower level of those blood flow rates previously reported (25% to 40% of normal cardiac output) from studies of closed-chest CPR. Different alkaline buffers influence circulatory and acid-base parameters differently before and after administration of epinephrine.
Comments Combination of high dose epinephrine and sodium bicarbonate produced lower systemic blood pressure
Level of Evidence 6 Quality Good Evidence -supportive
Vukmir, R. B., N. G. Bircher, et al. Sodium bicarbonate may improve outcome in dogs with brief or prolonged cardiac arrest. Critical Care Medicine 1995 23: 515-522.
Objective: To determine the effects of bicarbonate therapy on outcome in a canine model of ventricular fibrillation cardiac arrest of brief (5-min) and prolonged (15-min) duration. Methods Prospective, randomized, controlled trial involving adult dogs (n=32) .VF was induced and maintained in arrest for 5 mins (n = 12) or 15 mins (n = 20). Canine advanced cardiac life-support protocols were instituted, including defibrillation, cardiopulmonary resuscitation (CPR), and the administration of epinephrine (0.1 mg/kg), atropine, and lidocaine. The bicarbonate group received 1 mmol/kg of sodium bicarbonate initially, and base deficit was corrected to -5 mmol/L with additional bicarbonate, whereas acidemia was untreated in the control group. A neurologic deficit score was determined at 24 hrs after CPR. Results: The treatment group received an additional 2 to 3 mmol/kg of bicarbonate in the early postresuscitation phase. Compared with controls, the bicarbonate group demonstrated equivalent (with brief arrest) or improved (with prolonged arrest) return of spontaneous circulation and survival to 24 hrs, with lessened neurologic deficit. The acidosis of arrest was decreased in the prolonged arrest group without hypercarbia. Improved coronary and systemic perfusion pressures were noted in the bicarbonate group with prolonged arrest, and the epinephrine requirement for return of spontaneous circulation was decreased. Comments The empirical administration of bicarbonate improves the survival rate and neurologic outcome in a canine model of cardiac arrest. These observations support the current recommendation of sodium bicarbonate administration following prolonged resuscitation in the context of adequate ventilation. Level of Evidence 6 Quality Good Evidence- supportive
Wiklund, L.Ronquist, G.Stjernstrom, H. Waldenstrom, A Effects of alkaline buffer administration on survival and myocardial energy metabolism in pigs subjected to ventricular fibrillation and closed chest CPR Acta Anaesthesiol Scand 1990;34: 430-439 06f294d2760d96a36a00a71d6946c15d.doc Page 19 of 19
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Objective To determine the effects of alkaline buffer administration on survival and myocardial energy metabolism Methods Anesthetized piglets (n=19) were investigated. VF was induced followed by a 10-min period of cardiopulmonary resuscitation (CPR) i.e. manual chest compression and mechanical ventilation with pure oxygen. After 1 min of CPR an infusion of alkaline buffer was begun and was completed within 5 min. A total of 50 mmol of one of two different buffer solutions was given, either sodium bicarbonate (n = 6) or tris buffer mixture (n = 7). These two groups were compared with a third control group (n = 6) receiving the same volume of normal saline. After 8 min of CPR all animals were given 0.5 mg adrenaline i.v., Myocardial biopsies were then taken immediately in all animals. Results Successful CPR was more frequent in the animals given normal saline or tris buffer mixture and no effect was seen in the group given sodium bicarbonate. Survival was statistically correlated to low myocardial content of creatine phosphate and low base excess values in blood. Such parameters as myocardial content of ATP or ACP (adenylate charge potential) had no direct correlation to survival. Sodium bicarbonate induced significantly higher base excess and PCO2 values, while the tris buffer mixture seemed to have a greater alkalizing effect intracellularly.
Comments Sodium bicarbonate infusion was associated with higher PCO2. Level of Evidence 6 Quality Good Evidence- supportive