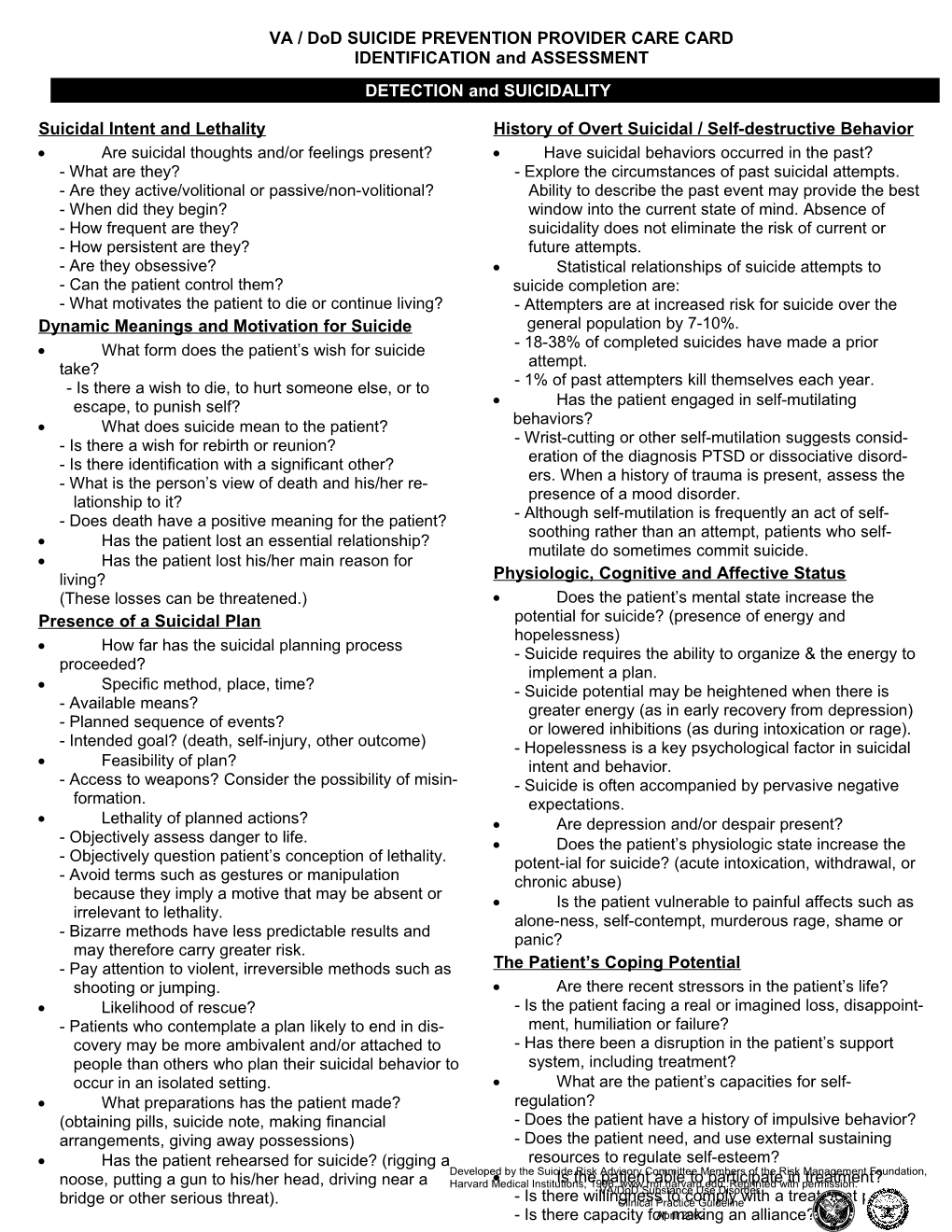
VA / DoD SUICIDE PREVENTION PROVIDER CARE CARD IDENTIFICATION and ASSESSMENT DETECTION and SUICIDALITY
Suicidal Intent and Lethality History of Overt Suicidal / Self-destructive Behavior Are suicidal thoughts and/or feelings present? Have suicidal behaviors occurred in the past? - What are they? - Explore the circumstances of past suicidal attempts. - Are they active/volitional or passive/non-volitional? Ability to describe the past event may provide the best - When did they begin? window into the current state of mind. Absence of - How frequent are they? suicidality does not eliminate the risk of current or - How persistent are they? future attempts. - Are they obsessive? Statistical relationships of suicide attempts to - Can the patient control them? suicide completion are: - What motivates the patient to die or continue living? - Attempters are at increased risk for suicide over the Dynamic Meanings and Motivation for Suicide general population by 7-10%. - 18-38% of completed suicides have made a prior What form does the patient’s wish for suicide take? attempt. - Is there a wish to die, to hurt someone else, or to - 1% of past attempters kill themselves each year. escape, to punish self? Has the patient engaged in self-mutilating What does suicide mean to the patient? behaviors? - Is there a wish for rebirth or reunion? - Wrist-cutting or other self-mutilation suggests consid- - Is there identification with a significant other? eration of the diagnosis PTSD or dissociative disord- - What is the person’s view of death and his/her re- ers. When a history of trauma is present, assess the lationship to it? presence of a mood disorder. - Does death have a positive meaning for the patient? - Although self-mutilation is frequently an act of self- soothing rather than an attempt, patients who self- Has the patient lost an essential relationship? mutilate do sometimes commit suicide. Has the patient lost his/her main reason for living? Physiologic, Cognitive and Affective Status (These losses can be threatened.) Does the patient’s mental state increase the Presence of a Suicidal Plan potential for suicide? (presence of energy and hopelessness) How far has the suicidal planning process - Suicide requires the ability to organize & the energy to proceeded? implement a plan. Specific method, place, time? - Suicide potential may be heightened when there is - Available means? greater energy (as in early recovery from depression) - Planned sequence of events? or lowered inhibitions (as during intoxication or rage). - Intended goal? (death, self-injury, other outcome) - Hopelessness is a key psychological factor in suicidal Feasibility of plan? intent and behavior. - Access to weapons? Consider the possibility of misin- - Suicide is often accompanied by pervasive negative formation. expectations. Lethality of planned actions? Are depression and/or despair present? - Objectively assess danger to life. Does the patient’s physiologic state increase the - Objectively question patient’s conception of lethality. potent-ial for suicide? (acute intoxication, withdrawal, or - Avoid terms such as gestures or manipulation chronic abuse) because they imply a motive that may be absent or Is the patient vulnerable to painful affects such as irrelevant to lethality. alone-ness, self-contempt, murderous rage, shame or - Bizarre methods have less predictable results and panic? may therefore carry greater risk. - Pay attention to violent, irreversible methods such as The Patient’s Coping Potential shooting or jumping. Are there recent stressors in the patient’s life? Likelihood of rescue? - Is the patient facing a real or imagined loss, disappoint- - Patients who contemplate a plan likely to end in dis- ment, humiliation or failure? covery may be more ambivalent and/or attached to - Has there been a disruption in the patient’s support people than others who plan their suicidal behavior to system, including treatment? occur in an isolated setting. What are the patient’s capacities for self- What preparations has the patient made? regulation? (obtaining pills, suicide note, making financial - Does the patient have a history of impulsive behavior? arrangements, giving away possessions) - Does the patient need, and use external sustaining Has the patient rehearsed for suicide? (rigging a resources to regulate self-esteem? Developed by the Suicide Risk Advisory Committee Members of the Risk Management Foundation, noose, putting a gun to his/her head, driving near a Harvard Medical Institutions,Is the 1996. patient www.rmf.harvard.edu. able to participate Reprinted with in permission.treatment? VA/DoD Substance Use Disorder bridge or other serious threat). - Is there willingnessClinical Practice to comply Guideline with a treatment plan? - Is there capacity forApril making 2002 an alliance?
VA / DoD SUICIDE PREVENTION PROVIDER CARE CARD IDENTIFICATION and ASSESSMENT MENTAL HEALTH DISORDERS CORRELATED with SUICIDAL BEHAVIOR Mood Disorders (15% lifetime risk of suicide) Schizophrenia (10% lifetime risk of suicide) The absence of psychosis does not imply safety. Relatively uncommon during psychotic episodes. A misleading reduction of anxious or depressed The relationship between command hallucinations affect can occur in some patients who have resolved and actual suicide is not clearly causal. the ambivalence by deciding to commit suicide. A Suicidal ideation occurs in 60-80 % of patients. patient who has made the decision to die may appear Suicidal attempts occur in 30-55% of patients. at peace and not show signs of an inner struggle. Suicide potential is increased by good premorbid Concern is warranted; especially when the patient functioning, early phase of illness, hopelessness or appears emotionally removed, shows constricted depression, and/or recognition of deterioration (during a affect, or is known to have given away belongings. post-psychotic depressed phase). The likelihood of suicide within one year is Panic Disorders (7-15% lifetime risk of suicide) increased when the patient exhibits panic attacks, Suicide rate may be similar to that of mood psychic anxiety, anhedonia, and/or alcohol abuse. disorders. The likelihood of suicide during the ensuing 1-5 Greater likelihood is correlated with more severe years is increased when the patient exhibits increased illness or comorbidity. hopelessness, suicidal ideation, and/or history of Suicide does not necessarily occur during a panic suicide attempts. attack. Borderline Personality Disorder (7% lifetime risk of Demoralization or significant loss increases the suicide) likelihood of suicide. Much higher risk associated with comorbidity, Agitation may increase the likelihood of especially with mood disorder and substance abuse. translating impulses into action. Psychopathology associated with increased risk Alcoholism (3% lifetime risk of suicide) includes: impulsivity, hopelessness and despair, Abusers of alcohol/drugs comprise 15-25% of antisocial features (with dishonesty), interpersonal suicides. aloofness (“malignant narcissism”), self-mutilating Alcohol is associated with nearly 50% of all tendencies, and psychosis with bizarre suicide suicides. attempts. Increased suicide potential in an alcoholic patient Psychopathology associated with diminished risk correlates with active substance abuse, adolescence, includes: infantile personality (with hysterical features) second or third decades of illness, and/or recent or and masochistic personality. anticipated interpersonal loss. Substance abuse can represent self-treatment to blunt the anxiety or mood disturbance associated with a masked, comorbid psychiatric disorder. SUICIDE RISK FACTORS The following risk factors provide explicit criteria for identifying the presence of factors correlated with a greater likelihood of suicide risk. With any individual patient, they assume greater or lesser importance. Under the Age of 30: (Adolescents & Young Adults) Over the Age of 30: Family history of suicide Family history of suicide Males > females Males > females History of previous attempts History of previous attempts Psychiatric diagnosis - mood disorders & substance Native American abuse Psychiatric diagnosis - mood disorders, schizophrenia White > black alcoholism Mini-epidemic in community Single, especially separated, widowed or divorced History of delinquent or semi-delinquent behavior Lack of social supports even without depression in current mental state Concurrent medical illness (es) Presence of firearms (when other factors are Unemployment present) Decline in socioeconomic status History of adverse childhood exposures Psychological turmoil History of adverse childhood exposures OTHER CONDITIONS WHICH CAN INCREASE SUICIDE RISK Physical illness, particularly associated with Family history of psychiatric illness & particularly of chronic pain suicide Delirium associated with organic illness Other personality disorders/states Psychopathology in family & social milieu, The presence of firearms in the home (particularly for including life stress & crisis adolescents) Developed by the Suicide Risk Advisory Committee Members of the Risk Management Foundation, Harvard Medical Institutions, 1996. www.rmf.harvard.edu. Reprinted with permission.