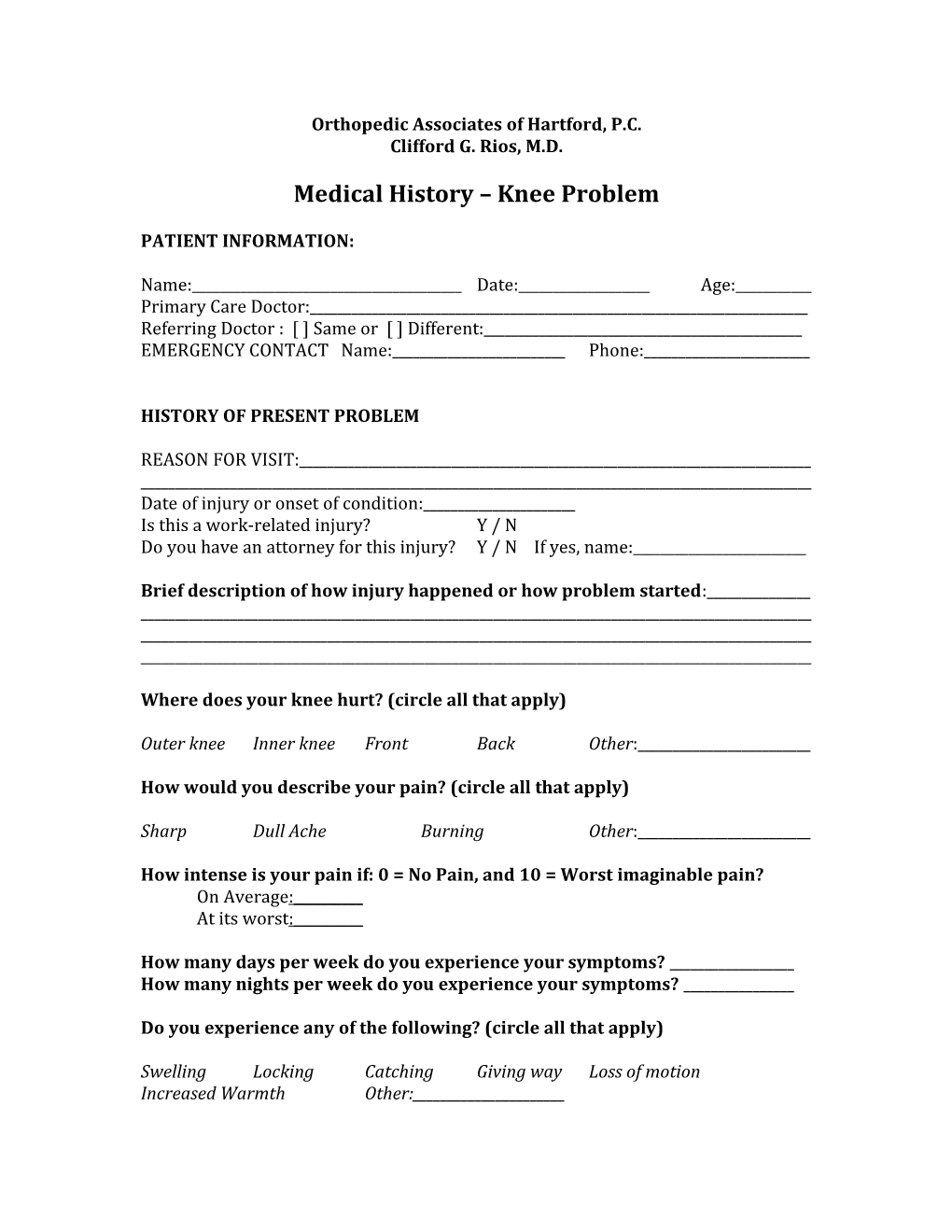
Orthopedic Associates of Hartford, P.C. Clifford G. Rios, M.D.
Medical History – Knee Problem
PATIENT INFORMATION:
Name:______Date:______Age:______Primary Care Doctor:______Referring Doctor : [ ] Same or [ ] Different:______EMERGENCY CONTACT Name:______Phone:______
HISTORY OF PRESENT PROBLEM
REASON FOR VISIT:______Date of injury or onset of condition:______Is this a work-related injury? Y / N Do you have an attorney for this injury? Y / N If yes, name:______
Brief description of how injury happened or how problem started:______
Where does your knee hurt? (circle all that apply)
Outer knee Inner knee Front Back Other:______
How would you describe your pain? (circle all that apply)
Sharp Dull Ache Burning Other:______
How intense is your pain if: 0 = No Pain, and 10 = Worst imaginable pain? On Average:______At its worst:______
How many days per week do you experience your symptoms? ______How many nights per week do you experience your symptoms? ______
Do you experience any of the following? (circle all that apply)
Swelling Locking Catching Giving way Loss of motion Increased Warmth Other:______What makes your symptoms worse? (Circle all that apply)
Walking Running Squatting Ascending stairs Descending stairs Kneeling Sitting with knee bent Pivoting Jumping Other:______
What treatments have you tried and did they help?
Ice: Y / N Helped: Y / N Rest: Y / N Helped: Y / N Physical therapy: Y / N Helped: Y / N Non-prescription medication: Y / N Helped: Y / N Prescription medication: Y / N Helped: Y / N Braces/orthotics Y / N Helped: Y / N Other treatment: ______Helped: Y / N
Do you participate in any recreational activities or sports and are you currently able to participate?
Activity:______Able to participate: Y / N / Haven’t tried Activity:______Able to participate: Y / N / Haven’t tried Activity:______Able to participate: Y / N / Haven’t tried
PAST MEDICAL HISTORY / REVIEW OF SYSTEMS
Seizures: Y / N Fevers / Chills / Sweats: Y / N Strokes: Y / N Poor vision: Y / N Heart disease / Arrhythmia: Y / N Headaches: Y / N Lung disease / Asthma: Y / N Chest pain / Palpitations: Y / N Reflux / Gastritis / Ulcers: Y / N Shortness of breath: Y / N Kidney / Bladder disease: Y / N Heartburn / Nausea: Y / N Diabetes: Y / N Urinary pain / urgency: Y / N Thyroid disease: Y/ N Joint pains / swelling: Y / N High Blood Pressure: Y / N Skin changes/poor healing: Y / N High cholesterol: Y / N Numbness / Tingling: Y / N Rheumatoid disease: Y / N Anxiety / Depression: Y / N Plebitis / Blood clots: Y / N Easy bleeding / bruising Y / N Hepatitis: Y / N Anemia: Y / N Cancer: Y / N Other:______
Do you take any medications (prescription or over-the-counter) on a regular basis? Med Dose # Times per day Med Dose #Times per day ______Do you have any allergies? Latex: Y / N Food: Y / N Specify if yes:______Iodine: Y / N Drugs: Y / N Drug:______Reaction:______
Have you ever been hospitalized or had surgery? (Please include dates) ______
PERTINENT FAMILY HISTORY: PARENTS/SIBLINGS AGES & HEALTH (IF DECEASED, AGE AT DEATH AND CAUSE) ______
SOCIAL HISTORY
Are you (please circle): Single Married Widowed Employment status: Full-time Part-time Unemployed Student Do you have children? Y / N Age(s) ______Do you consume alcohol? Y / N If yes, how much/often ______Do you use tobacco products? Y / N If yes, how much/often ______Do you use illicit drugs? Y / N If yes, how much/often ______
CONSTITUTIONAL SIGNS
Height: ______’ ______” Weight: ______lbs
PATIENT SIGNATURE:______DATE:______
DOCTOR SIGNATURE:______DATE:______
RETURN VISITS DATE/INITIALS: PMH/ROS: DETAILS IF YES: ______Y / N ______Y / N ______Y / N ______Y / N ______Y / N ______Y / N ______Y / N ______