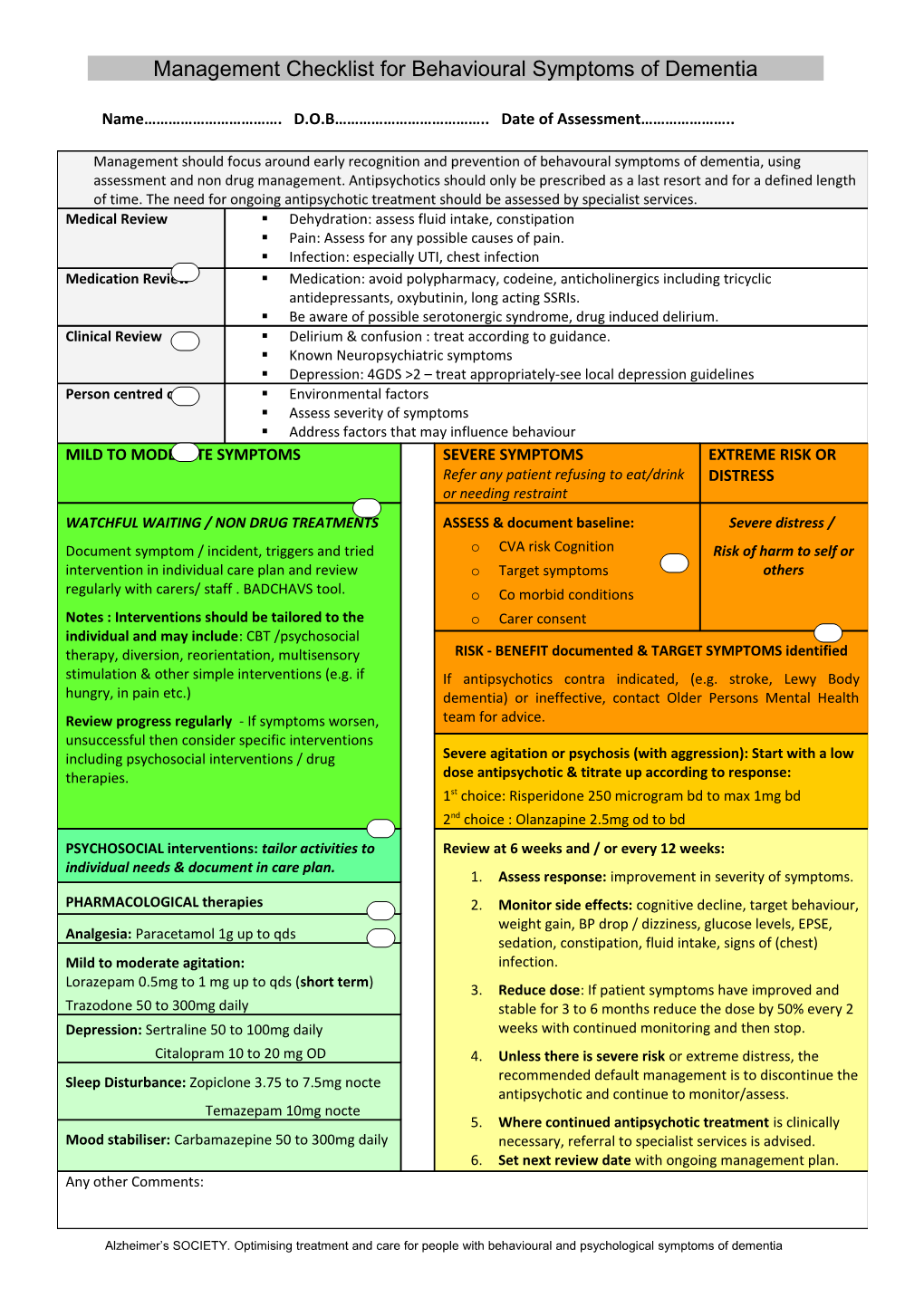
Management Checklist for Behavioural Symptoms of Dementia
Name……………………………. D.O.B……………………………….. Date of Assessment…………………..
Management should focus around early recognition and prevention of behavoural symptoms of dementia, using assessment and non drug management. Antipsychotics should only be prescribed as a last resort and for a defined length of time. The need for ongoing antipsychotic treatment should be assessed by specialist services. Medical Review . Dehydration: assess fluid intake, constipation . Pain: Assess for any possible causes of pain. . Infection: especially UTI, chest infection Medication Review . Medication: avoid polypharmacy, codeine, anticholinergics including tricyclic antidepressants, oxybutinin, long acting SSRIs. . Be aware of possible serotonergic syndrome, drug induced delirium. Clinical Review . Delirium & confusion : treat according to guidance. . Known Neuropsychiatric symptoms . Depression: 4GDS >2 – treat appropriately-see local depression guidelines Person centred care . Environmental factors . Assess severity of symptoms . Address factors that may influence behaviour MILD TO MODERATE SYMPTOMS SEVERE SYMPTOMS EXTREME RISK OR Refer any patient refusing to eat/drink DISTRESS or needing restraint WATCHFUL WAITING / NON DRUG TREATMENTS ASSESS & document baseline: Severe distress / Document symptom / incident, triggers and tried o CVA risk Cognition Risk of harm to self or intervention in individual care plan and review o Target symptoms others regularly with carers/ staff . BADCHAVS tool. o Co morbid conditions Notes : Interventions should be tailored to the o Carer consent individual and may include: CBT /psychosocial therapy, diversion, reorientation, multisensory RISK - BENEFIT documented & TARGET SYMPTOMS identified stimulation & other simple interventions (e.g. if If antipsychotics contra indicated, (e.g. stroke, Lewy Body hungry, in pain etc.) dementia) or ineffective, contact Older Persons Mental Health Review progress regularly - If symptoms worsen, team for advice. unsuccessful then consider specific interventions including psychosocial interventions / drug Severe agitation or psychosis (with aggression): Start with a low therapies. dose antipsychotic & titrate up according to response: 1st choice: Risperidone 250 microgram bd to max 1mg bd 2nd choice : Olanzapine 2.5mg od to bd PSYCHOSOCIAL interventions: tailor activities to Review at 6 weeks and / or every 12 weeks: individual needs & document in care plan. 1. Assess response: improvement in severity of symptoms. PHARMACOLOGICAL therapies 2. Monitor side effects: cognitive decline, target behaviour, weight gain, BP drop / dizziness, glucose levels, EPSE, Analgesia: Paracetamol 1g up to qds sedation, constipation, fluid intake, signs of (chest) Mild to moderate agitation: infection. Lorazepam 0.5mg to 1 mg up to qds (short term) 3. Reduce dose: If patient symptoms have improved and Trazodone 50 to 300mg daily stable for 3 to 6 months reduce the dose by 50% every 2 Depression: Sertraline 50 to 100mg daily weeks with continued monitoring and then stop. Citalopram 10 to 20 mg OD 4. Unless there is severe risk or extreme distress, the Sleep Disturbance: Zopiclone 3.75 to 7.5mg nocte recommended default management is to discontinue the antipsychotic and continue to monitor/assess. Temazepam 10mg nocte 5. Where continued antipsychotic treatment is clinically Mood stabiliser: Carbamazepine 50 to 300mg daily necessary, referral to specialist services is advised. 6. Set next review date with ongoing management plan. Any other Comments:
Alzheimer’s SOCIETY. Optimising treatment and care for people with behavioural and psychological symptoms of dementia