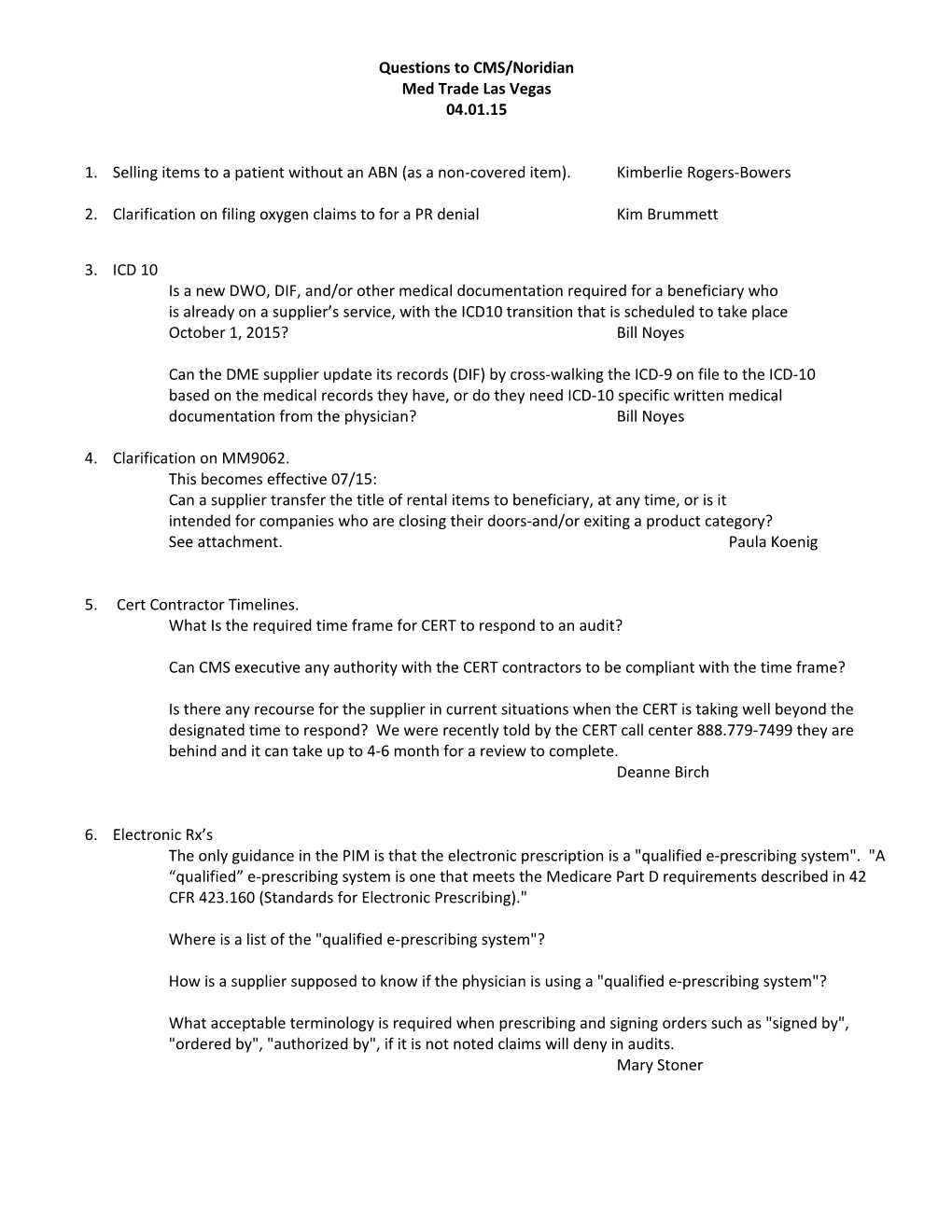
Questions to CMS/Noridian Med Trade Las Vegas 04.01.15
1. Selling items to a patient without an ABN (as a non-covered item). Kimberlie Rogers-Bowers
2. Clarification on filing oxygen claims to for a PR denial Kim Brummett
3. ICD 10 Is a new DWO, DIF, and/or other medical documentation required for a beneficiary who is already on a supplier’s service, with the ICD10 transition that is scheduled to take place October 1, 2015? Bill Noyes
Can the DME supplier update its records (DIF) by cross-walking the ICD-9 on file to the ICD-10 based on the medical records they have, or do they need ICD-10 specific written medical documentation from the physician? Bill Noyes
4. Clarification on MM9062. This becomes effective 07/15: Can a supplier transfer the title of rental items to beneficiary, at any time, or is it intended for companies who are closing their doors-and/or exiting a product category? See attachment. Paula Koenig
5. Cert Contractor Timelines. What Is the required time frame for CERT to respond to an audit?
Can CMS executive any authority with the CERT contractors to be compliant with the time frame?
Is there any recourse for the supplier in current situations when the CERT is taking well beyond the designated time to respond? We were recently told by the CERT call center 888.779-7499 they are behind and it can take up to 4-6 month for a review to complete. Deanne Birch
6. Electronic Rx’s The only guidance in the PIM is that the electronic prescription is a "qualified e-prescribing system". "A “qualified” e-prescribing system is one that meets the Medicare Part D requirements described in 42 CFR 423.160 (Standards for Electronic Prescribing)."
Where is a list of the "qualified e-prescribing system"?
How is a supplier supposed to know if the physician is using a "qualified e-prescribing system"?
What acceptable terminology is required when prescribing and signing orders such as "signed by", "ordered by", "authorized by", if it is not noted claims will deny in audits. Mary Stoner Previously Submitted Questions to CMS
Foscarnet Injection Pricing Foscarnet Sodium Injection, J1455, per 1000mg unit. Brand name product: Foscavir Injection, manufactured by Hospira, available in the U.S. Generic name: Foscarnet Sodium (no longer available in the U.S.)
Background:
Foscarnet Sodium is antiviral injection medication used to treat certain types of viral infections in HIV- infected patients and otherwise immunocompromised patients. It is covered under Medicare Part B and requires a pump for safe administration. If a patient meets certain criteria, the External Infusion Pump and Supplies to administer the medication are also covered.
Medicare’s current reimbursement is $13.07 per 1000mg unit. This pricing was based on the generic product. However, production of the generic Foscarnet was discontinued a number of months ago and is not expected to return. The only product available now is the Brand name Foscavir Injection. The Average Wholesale Price of Foscavir Injection is $47.18 per 1000mg unit as of 10/24/2014.
What is happening now in home care:
Home infusion providers are declining to provide this medication to patients at home due to the limited reimbursement. Therefore, patients are being forced to inpatient care, skilled nursing facility, or traveling to an outpatient infusion center multiple times per day to receive this medication. This is putting an unnecessary strain on acute health care resources and resulting in higher Medicare Part A expenditures.
What must happen for change:
CMS must work with the manufacturer of Foscavir Injection, which is Hospira, to adjust the current allowable reflecting current product availability. Deanne Birch
Q. 18. IF a patient wants to switch to another company for PAP supplies but the documentation is not available because the original setup was done over 7 years ago in 2002:
a. Is it sufficient to document a statement that medical records older than 7 years are not required to be produced in the event of an audit?
b. Are we still required to prove the patient qualified at setup?
c. What are the minimum number of elements necessary to justify in an audit the billing for ongoing supplies for an “archived medical record” patient? (e.g. current office notes documenting DX of OSA along with use and benefit, a new script, a copy of the original sleep study, etc.)? Deanne Birch