Last Minute Board Review
Cardiovascular
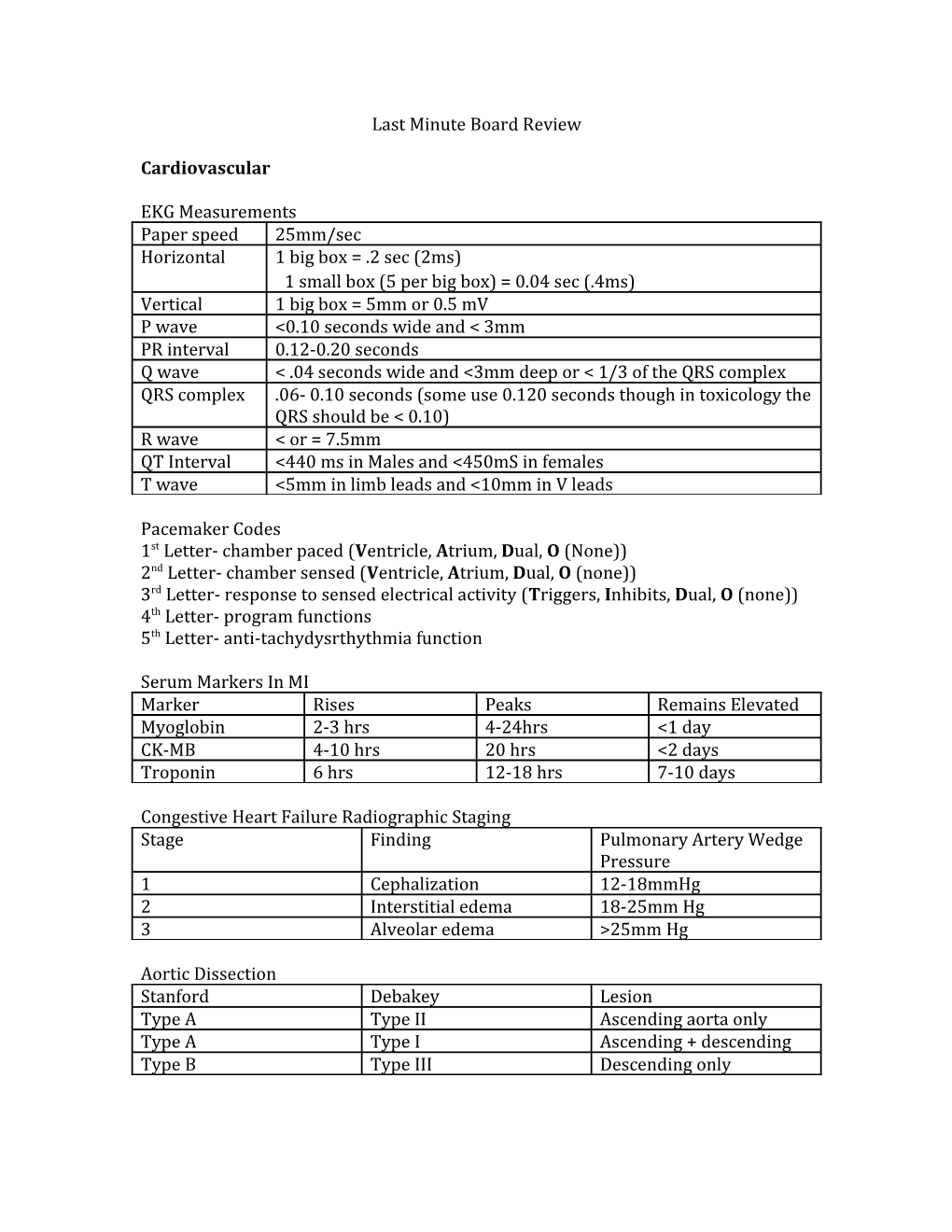
EKG Measurements Paper speed 25mm/sec Horizontal 1 big box = .2 sec (2ms) 1 small box (5 per big box) = 0.04 sec (.4ms) Vertical 1 big box = 5mm or 0.5 mV P wave <0.10 seconds wide and < 3mm PR interval 0.12-0.20 seconds Q wave < .04 seconds wide and <3mm deep or < 1/3 of the QRS complex QRS complex .06- 0.10 seconds (some use 0.120 seconds though in toxicology the QRS should be < 0.10) R wave < or = 7.5mm QT Interval <440 ms in Males and <450mS in females T wave <5mm in limb leads and <10mm in V leads
Pacemaker Codes 1st Letter- chamber paced (Ventricle, Atrium, Dual, O (None)) 2nd Letter- chamber sensed (Ventricle, Atrium, Dual, O (none)) 3rd Letter- response to sensed electrical activity (Triggers, Inhibits, Dual, O (none)) 4th Letter- program functions 5th Letter- anti-tachydysrthythmia function
Serum Markers In MI Marker Rises Peaks Remains Elevated Myoglobin 2-3 hrs 4-24hrs <1 day CK-MB 4-10 hrs 20 hrs <2 days Troponin 6 hrs 12-18 hrs 7-10 days
Congestive Heart Failure Radiographic Staging Stage Finding Pulmonary Artery Wedge Pressure 1 Cephalization 12-18mmHg 2 Interstitial edema 18-25mm Hg 3 Alveolar edema >25mm Hg
Aortic Dissection Stanford Debakey Lesion Type A Type II Ascending aorta only Type A Type I Ascending + descending Type B Type III Descending only Murmur Maneuvers Maneuver Mitral Valve Prolapse HOCM Decrease LV volume Longer murmur, click Increases murmur (valsalva, sudden moves closer to S1 (earlier standing) and greater prolapse Increase LV volume Shorter murmur and Decreases murmur (squat, passive leg raise, delayed click (decrease in hand grip) prolapse)
Jones Criteria (For Rheumatic Fever) Need 2 major (or 1 major + 2 minor) plus evidence of preceding GABH infection Major (CASES)- Carditis, Arthritis, Sydenham Chorea, Erythema Marginatum, Subcutaneous Nodules) Minor- fever, arthralgia, history of rheumatic fever, lab findings (elevated WBC, ESR, CRP, or long PR interval)
Reperfusion Times for STEMI (symptoms less than 12 hours) Door To Balloon (PCI) < 90 minutes Door To Needle (Fibrinolysis) <30 minutes
Fibrinolytic Contraindications Absolute Any prior intracranial hemorrhage Known structural cerebral vascular lesion Known malignant intracranial neoplasm Ischemic stroke within 3 months (if they have had stroke symptoms for less than 3 hours though you’re in the clear) Suspected aortic dissection Active bleeding or bleeding diathesis (excluding menses) Significant closed head or facial trauma within 3 months Relative Hx of chronic, severe, or poorly controlled HTN Severe uncontrolled HTN on presentation (>180 SBP or >110 DBP) History of prior ischemic stroke >3 months, dementia, or known intracranial pathology not covered in contraindications Traumatic or prolonged (>10 min) CPR Major surgery <3 weeks Recent (within 2-4 weeks) internal bleeding Noncompressible vascular punctures For streptokinase/anistreplase: prior exposure (>5 days ago) or prior allergic reaction to these agents Pregnancy Active peptic ulcer Current use of anticoagulants (the higher the INR, the higher the bleeding risk) Hypertension
Stage SBP DBP Treatment Pre-HTN 120-140 80-90 Lifestyle change Stage I 140-160 90-100 1-2 meds Stage II >160 >100 Start 2 meds
Pulmonary
A-a Gradient = 150-[PO2 + (PCO2/.08)] normal is 10-12
Wells for DVT (1 point each) Active cancer Recent immobilization/paralysis Bedridden for >3 days or major surgery within 4 weeks Localized tenderness along deep vein system Entire leg swollen Calf swelling >3cm compared to opposite leg Pitting edema Collateral superficial veins evident “Alternate diagnosis”= if you really think its something else then subtract 2 0 = low risk (<10%) 1-2 moderate risk (10-65%) 3 = high risk (>65%)
Wells Criteria for PE Suspected DVT 3 points “Alternative Diagnosis” so if you think it is a PE 3 points Pulse >100 bum 1.5 points Immobilization (or surgery) within 4 weeks 1.5 points Hx of previous DVT/PE 1.5 points Hx of hemoptysis 1 point Hx of malignancy 1 point <2 = low pretest prob (3.6% risk) 2-6= mod prob (20.5%) >6 high prob (66.7%)
PCP Pneumonia CD4 count usually <200 Treat with steroids if pO2 <70 or A-a gradient is >35mmHg
Pleural Effusions Exudate if Pleural fluid protein/serum protein >0.5 Pleural fluid LDH > 200 Pleural fluid LDH/serum LDH >0.6 Pleural fluid cholesterol >60 mg/dL Pneumothorax Reabsorb 1% per day without oxygen and 5% a day with 100% oxygen
ARDS PaO2:FiO2 <200
PFTs Obstructive Pathology = FEV1/FVC of <80%
Massive hemoptysis= 50mL blood in one expectorant or >600mL/day
Gastrointestinal
Esophageal FB levels C6- cricopharyngeus (most common site of FB in kids) T4- aortic arch T10-11 = lower esophageal sphincter (most common site in adults)
Hepatitis Incubation Periods Hepatitis A = 15-50 days Hepatitis B = 45-160 days Hepatitis C = 15-150 days
Ranson’s Criteria (Remember “Georgia Law” GA LAW) at 24 hours Glucose > 200 AST > 250 LDH >350 Age >55 Leukocytosis >16,000
Peritoneal Fluid Analysis Serum Albumin- peritoneal fluid albumin= SAAG SAAG >1.1 g/dL is portal hypertension Spontaneous Bacterial Peritonitis WBC >500 cells/uL WBC >250 cells/uL with 50% neutrophils (more conservative)
Orthopedics
Compartment Pressure > 30mmHG = fasciotomy Synovial Fluid Analysis Normal Traumatic Inflammatory Septic WBC <250 WBC/mm3 200-2000 2,000-50,000 5,000->50,000 Neutrophils <25% of WBC <25% 50-75% >75% Glucose 95-100% serum 95-100% 75% <50% glucose
Trauma
Hemorrhagic Shock Classification Class I Class II Class III Class IV Volume Loss % 0-15% 15-30% 30-40% >40% Volume Loss (mL) 0-750mL 750-1500mL 1500-2000mL >2000mL Heart Rate <100 >100 >120 >140 Pulse Pressure Normal Decreased Decreased Decreased Blood Pressure Normal Normal Decreased Decreased Mental Status Slightly Mildly anxious Anxious, Confused, anxious confused lethargic Urine Output >30ml/hr 20-30 ml/hr 5-15 ml/hr Negligible Fluid Replacement Crystalloid Crystalloid Add blood Add blood
Indications for Thoracotomy with Hemothorax Initial output of >1500mL of blood 50% hemothorax >200ml/hr for the first 2-4 hours Persistent decompensation or need for transfusions
Diagnostic Peritoneal Lavage Positive DPL >10mL of gross blood >100,000 RBC for blunt trauma >100,000 RBC for most stab wounds >5,000 RBC for gunshot wounds (and “low chest” stab wounds)
Cervical Spine Injuries in Children Children <8 years old have mostly high C-spine injuries Children >12 years old are like adults and have low C-spine injuries
Spinal Injuries Extension Type Hangman’s (C2 fx) Extension teardrop Posterior atlanto-axial dislocation Neural Arch fracture (of C1) All of the rest are flexion (except for burst which is compression)
Spinal Cord Injuries Central Cord (Hyperextension)- arm greater than leg weakness Anterior Cord (Hyperflexion)- paralysis and decreased sensation Brown Sequard (hemisection)- ipsilateral hemiplegia with contralateral sensory deficits
Glasgow Coma Scale (best response) Score Eye Opening Verbal Motor 6 X X Obeys commands 5 X Oriented, Localize to pain conversant 4 Spontaneous Confused Withdraws 3 To voice Inappropriate Abnormal flexion words (decorticate) 2 To pain Moaning Extension (decerebrate) 1 None none None
Obstetrics/Gynecology
Pre-Eclampsia Mild Severe Blood Pressure SBP >140 DBP >90 SBP >160 DBP>110 Protein 0.3gm/24 hour >5gm/24 hour
Urology/Nephrology
Urine Sodium- Low = <20, High = > 40
FENa <1 is pre-renal
Urine osmolality >500 is concentrated and <300 is dilute
Urine culture results- Positive if: >100,000 (105)/mL >100 (102)/mL if symptomatic
Pediatrics
Shock Blood 10ml/Kg Fluid 20ml/kg Maintenance fluids 4ml/kg for the first 10kg 2ml/kg for the next 10kg 1ml/kg for each kg after this
ET tube diameter= (Age in years/4) + 4
Cardioversion Synchronized = 0.5J/kg Defibrillating= 2J/kg
APGAR Score 0 1 2 Activity (tone) Limp Minimal flexion Good flexion Pulse Absent <100 >100 Grimace (to None Some motion Cry irritation) Appearance Blue Body pink/ ext Pink blue Respirations Absent Slow/irreg Good, crying
Causes of death Birth-1month = infection 1month- 1year = SIDS >1 year = trauma
Kawasaki Disease Fever for 5 days plus 4 out of the following: Changes of the lips/oral cavity (strawberry tongue, redness Bilateral nonsuppurative conjunctivitis Extremity features (palmar/plantar erythema, induration) Rash- lacey erythematous on the trunk Cervical lymphadenopathy (usually unilateral)
Cyanotic Heart Lesions (remember the hand mnemonic) 1. Truncus arteriosis 2. Transposition of the great vessels 3. Tricuspid atresia 4. Tetralogy of Fallot 5. Total Anomalous pulmonary venous return
Metabolic/Allergic
Serum Osmolality: 2(Na) + Glucose/18 + BUN/2.8 + Ethanol/4.6
Anion Gap Na- (HCO3 + Cl)
Winter’s Formula Expected PCO2 (+/- 2)= 1.5 x HCO3 +8
Allergic/Hypersensitivity Reactions Type I: Immediate, IgE, bee stings, PCN allergy Type II: Cytotoxic/compliment mediated, ITP, Blood transfusion rxn Type III: Immune Complex ,(IgE with antigen clump up), serum sickness Type IV: Delayed, T-cell mediated, TB test or poison ivy Toxicology
Activated Charcoal: 1g/kg or 10:1 charcoal to toxin
Lithium 0.6-1.2 mEq/L therapeutic Dialysis for Clinical signs of mod to severe poisoning Worsening of clinical condition despite falling levels Dysrhythmias Decreasing urine output or renal failure Serum level >4 mEQ/L
Salicylates (draw levels at 4-6 hrs then every 4 hours) Dialysis for Serum ASA >90-100mg/dL Neurologic signs/symptoms (confusion, coma, sz) Renal failure Pulmonary edema Severe cardiac toxicity Severe acid-base imbalance Rising ASA levels despite urinary alkylinization
Acetaminophen Phase Time Symptoms 1 0-24hr N/V, anorexia 2 24-72hr Increasing hepatic enzymes but may be quiescent 3 3-4 days Hepatic failure and encephalopathy 4 4days- If survive stage III then will have complete resolution of 2week hepatic dysfunction Iron Potential toxicity at 40-70mg/kg Blood levels and toxicity Mild: 150-300 Moderate 300-500 Severe >500 Iron Concentrations (Feels So Good as you go down) Ferrous Fumarate = 30% elemental iron Ferrous Sulfate = 20% elemental iron Ferrous Gluconate = 10% elemental iron Stages (very much like APAP) Stage Time Manifestations 1 0-6hr V/D, abdominal pain, GI bleeding 2 4-12 hrs Improvement in symptoms (developing acidosis) 3 6-72 hrs Coma, shock, sz, coagulopathy 4 12-96hr Hepatic failure, hypoglycemia 5 2-4 wks Pyloric scarring and bowl obstructions
Hydrocarbons Badness= low viscosity and high volatility
Amanita Poisoning (again, a lot like APAP) Phase Time Manifestations 1 6-10hr N/V/d 2 24-48hr Symptoms resolve but LFT rise 3 1-6days Hepatic failure, renal failure, encephalopathy, death With mushrooms you would always rather vomit immediately then have delayed vomiting (the bad mushrooms cause delayed vomiting)
Taylor Cyanide Kit Amyl/Sodium nitrite- induce Methemoglobinemia (don’t use in a fire victim) Sodium thiosulfate- sulfur donor
Carbon Monoxide (suggested hyperbaric therapy- very controversial) CoHb level >25% COHb level >10% and pregnant Any neuro symptom other than HA (including brief syncope) Coma MI Worsening symptoms with oxygen therapy Electrolytes/Fluids
Total Body Water= 60mL/kg male and 50ml/kg in female Total Blood Volume in adults 70ml/kg (7% body weight) Total Blood Volume in children 90ml/kG (9% body weight)
3:1 rule- for every 3 L of crystalloid you infuse, only 1L stays intravascular
Neurology
Strokes made simple MCA-contralateral upper more than lower weakness/sensation, aphasia/agnosia ACA- contralateral lower more than upper weakness/sensation, no frontal lobe PCA- Ipsilateral CN III palsy, contralateral homonymous hemianopsia, memory loss All vertebral/brainstem lesions have crossing/mixed signs VA- ipsilateral cranial nerve palsy, contralateral sensory defect, cerebellar signs Wallenberg Syndrome (Lateral Medullary Plate)- Horner’s, vertigo, ipsilateral facial numbness Basilar- bilateral signs, Locked-in Lacunar- small, focal, isolated motor or sensory
Tetanus mimic? = Strychnine
Physostigmine crosses the blood brain barrier
Lower CO2 to between 30-35mmHg for acute ICP increase
Uncal herniation- Ipsilateral pupil dilation and fixation Central herniation- sudden respiratory changes and posturing Cerebellar tonsillar herniation- pinpoint pupils, apnea
Fibrinolytics in Stroke (must be >18 YO, <3 hrs since normal, and measurable defect Absolute Contraindications Evidence of intracranial bleeding (clinical or on head CT) Multilobar infarct (greater than 1/3 the cerebrum) History of any intracranial hemorrhage Known AVM, neoplasm, aneurysm Witnessed seizure at stroke onset SBP >185 or DBP >110 after treatment Active internal bleeding or trauma Bleeding diathesis (Plt <100,000, Heparin in 48 hrs, INR >1.7) Within 3 months of intracranial surgery, spinal surgery, prior stroke Arterial puncture at non-compressible site in past 7 days Relative Contraindications Only minor or rapidly improving symptoms Within 14 days of major trauma or surgery Recent GI or GU hemorrhage (21 days) Recent MI (in 3 months) Post MI pericarditis Blood glucose <50 or >200
Environmental
Burn Transfer Criteria Second- or third-degree burns greater than 10% total body surface area (TBSA) in patients younger than 10 years or older than 50 years Second- or third-degree burns greater than 20% TBSA in persons of other age groups Second- or third-degree burns that involve the face, hands, feet, genitalia, perineum, or major joints Third-degree burns greater than 5% TBSA in persons of any age group Electrical burns, including lightening injury Chemical burns Inhalational injury Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality Any patients with burns or concomitant trauma A lack of qualified personnel or equipment for the care of children (transfer to facility with these qualities)
Parkland Formula (only includes 2nd and 3rd degree burns >20%) 4ml/kg X BSA- give LR and give half in the first 8 hours (AFTER THE BURN NOT AFTER PRESENTATION TO THE ER) Brooke Formula uses 2ml/kg Add maintenance fluids for children
High Voltage is >1,000 volts
AC effects are usually worse than DC effects b/c you can’t let go
Voltage= current x resistance
Hypothermia Temperature Type Rewarming 34-36 C Mild Passive external 30-34 C Moderate Active external (noninvasive active internal) <30 C Severe Invasive Active internal Moderate altitude = 8,000-10,000 ft High altitude is 10,000-18,000 ft
High Altitude Pulmonary Edema is uncommon below 10,000 ft
High Altitude Cerebral Edema is uncommon below 12,000 ft
Radiation Doses Mild dose (n/v/d)= 75-125 rads Moderate dose (Acute radiation syndrome)= 100-200 rads Severe (massive fluid loss, sepsis)= 500 rads
Absolute Lymphocyte count at 48 hours >1200/mm3= good prognosis 300-1200/mm3= fair prognosis <300/mm3= poor prognosis
Hematologic/Oncologic
Factor Replacement in Hemophilia Severity Examples Factor Replacement Severe Head injury, major trauma, intra-abdominal 50 units/kg Moderate Oral lacerations, dental extractions, late 26 units/kg hemarthrosis Mild Early hemarthrosis, hematuria, deep 18 units/kg laceration
Cyanosis requires 5mg/dL of deoxygenated hemoglobin
EMS/Legal
Negligence (must have the 4 components) 1. Duty to treat- they belong to you 2. Breach of duty- you didn’t follow standard of care 3. Causation- you caused an injury and this could be foreseen 4. Damages- the result is actually a problem
Laws you might have to know Highway Safety Act of 1966- established DOT and EMS EMS Act of 1973- development of EMS standards of care ER planning 12-14 parking spaces per 20,000 annual patient visits 1 patient space per 2000 annual visits
Minimum Staffing levels 30,000 annual patient visits = 5 full time docs with double coverage during peak hours 40,000 annual patient visits = 6 full time docs with double coverage during peak hours