The Sight Loss and Vision Priority Setting Partnership
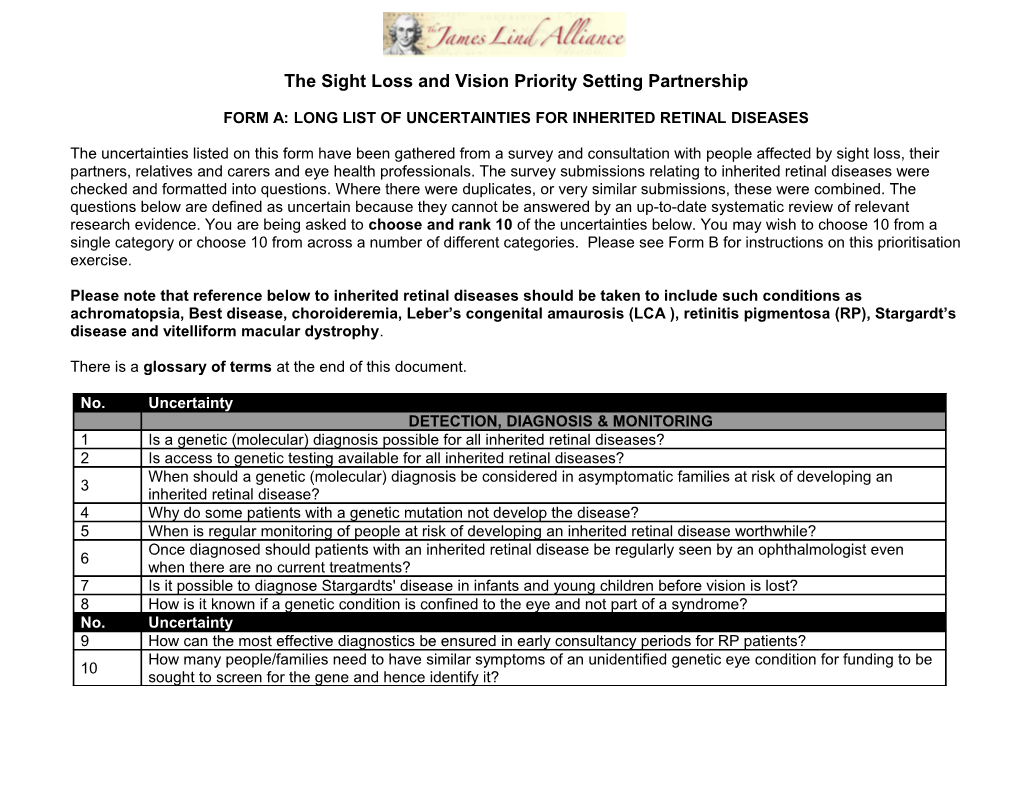
FORM A: LONG LIST OF UNCERTAINTIES FOR INHERITED RETINAL DISEASES
The uncertainties listed on this form have been gathered from a survey and consultation with people affected by sight loss, their partners, relatives and carers and eye health professionals. The survey submissions relating to inherited retinal diseases were checked and formatted into questions. Where there were duplicates, or very similar submissions, these were combined. The questions below are defined as uncertain because they cannot be answered by an up-to-date systematic review of relevant research evidence. You are being asked to choose and rank 10 of the uncertainties below. You may wish to choose 10 from a single category or choose 10 from across a number of different categories. Please see Form B for instructions on this prioritisation exercise.
Please note that reference below to inherited retinal diseases should be taken to include such conditions as achromatopsia, Best disease, choroideremia, Leber’s congenital amaurosis (LCA ), retinitis pigmentosa (RP), Stargardt’s disease and vitelliform macular dystrophy.
There is a glossary of terms at the end of this document.
No. Uncertainty DETECTION, DIAGNOSIS & MONITORING 1 Is a genetic (molecular) diagnosis possible for all inherited retinal diseases? 2 Is access to genetic testing available for all inherited retinal diseases? When should a genetic (molecular) diagnosis be considered in asymptomatic families at risk of developing an 3 inherited retinal disease? 4 Why do some patients with a genetic mutation not develop the disease? 5 When is regular monitoring of people at risk of developing an inherited retinal disease worthwhile? Once diagnosed should patients with an inherited retinal disease be regularly seen by an ophthalmologist even 6 when there are no current treatments? 7 Is it possible to diagnose Stargardts' disease in infants and young children before vision is lost? 8 How is it known if a genetic condition is confined to the eye and not part of a syndrome? No. Uncertainty 9 How can the most effective diagnostics be ensured in early consultancy periods for RP patients? How many people/families need to have similar symptoms of an unidentified genetic eye condition for funding to be 10 sought to screen for the gene and hence identify it? 11 How would pre-screening pregnant mothers reduce the risk of congenital blindness such as in the case of LCA? 12 What is the most effective way to support patients with inherited retinal disease? 13 How often should someone with Marfans syndrome without any evidence of a sight problem be monitored? PROGNOSIS How much is known about the long term prognosis (natural history) for inherited retinal diseases and is it related to 14 the genotype? Can the diagnosis of retinal dystrophies be refined so that individuals can be given a clearer idea about their 15 specific condition and how it is likely to progress? 16 What genetic factors affect the rate and degree of visual deterioration for people with LCA? 17 Can the rate of sight loss for people with RP be predicted? 18 Will Sorsby's fundus dystrophy cause retinal problems later in life? 19 What is the impact of the second mutation in autosomal recessive disease on RP progression? 20 What factors affect the progression of sight loss in inherited retinal diseases? CAUSE & PREVENTION 21 What is the cause of sight loss in adult vitelliform macular dystrophy? 22 How can adult vitelliform macular dystrophy be prevented? 23 What are the genetic faults that cause achromatopsia? 24 With cone dystrophy, why is the colour lens affected in some families and not in others? 25 What causes the cones to stop working efficiently in cone dystrophy? 26 What are genetic and environmental influences on juvenile macular disease such as Stargardts and Best disease? No. Uncertainty 27 What causes sight loss in RP? 28 Does stress increase progression of sight loss in inherited retinal diseases? 29 What is the relationship between sight loss and mental health for people with LCA? 30 Is there any evidence that certain drugs can cause genetic mutations leading to RP? 31 How can RP be prevented? 32 What are the genetics of RP? 33 Can lifestyle or dietary factors trigger or prevent the onset of sight loss in RP? 34 Why do genetic defects due to RP only affect the eye and not other organs? 35 How can people with cerebral palsy get RP if there is no family history of this disease? 36 What is the likelihood that hereditary form of RP (X-linked RPGR) is revealing as sight loss in female carriers? 37 What is the likelihood that the use of sunglasses from an early age can prevent sight loss in RP? 38 Is there any known link between Sorsby's fundus dystrophy and emphysema? 39 Could Sorsby's fundus dystrophy manifest earlier in the children of someone with Sorsby's? 40 How can Sorsby's fundus dystrophy be prevented? 41 What causes vision loss in Stargardts disease? 42 Can the genetic defects be corrected in utero to prevent RP and other inherited retinal diseases? 43 What is the role of pre-natal and pre-implantation diagnosis in preventing inherited retinal diseases? How do people with achromatopsia who have never seen colour 'learn' what their shades of grey are in terms of 44 colour? TREATMENT 45 How can sight loss be treated in people with an inherited retinal disease? 46 Can a treatment to slow down progression or reverse sight loss in inherited retinal diseases be developed? No. Uncertainty 47 Can eye transplants be developed for people with inherited retinal diseases? 48 Could a treatment in the form of eye drops be developed for inherited retinal diseases? Will gene therapy stop the progression of sight loss and reverse sight loss in inherited retinal diseases and in 49 syndromes associated with RP, such as Usher and Alström syndromes? 50 Is it possible to determine which inherited retinal diseases are likely to be treatable with gene therapy? Would having a treatment for an inherited retinal disease (e.g. retinal implants) preclude a patient from having 51 another treatment (gene therapy)? Can a stem cell therapy stop progression of sight loss and restore sight for inherited retinal diseases and for 52 syndromes associated with RP, such as Usher and Alström syndromes, be developed? 53 Are there any potential long term risks associated with gene therapy for inherited retinal diseases? 54 Are there any potential long term risks associated with potential stem cell therapies for inherited retinal diseases? Can dietary measures, nutritional supplements, vitamins, complementary therapies or lifestyle changes affect the 55 progression of sight loss in inherited retinal diseases? 56 Are there any drugs that are harmful for patients with RP and other inherited retinal diseases? 57 What types of glasses/lenses can be beneficial for people with RP? 58 Should vitamin A supplements be avoided in people with Stargardts? What is the likelihood that computerised artificial eyes/retinal implants can restore sight loss due to inherited retinal 59 disease? 60 How can symptoms of photopsia in people with RP be treated? 61 What treatment options exist for people with Stickler syndrome? 62 Is it possible to develop a treatment for vision loss in Alström syndrome? 63 Can dietary measures, nutritional supplements or vitamins slow the progression of sight loss in Usher syndrome? Glossary of terms:
Achromatopsia: A non-progressive and hereditary visual disorder which is characterized by decreased vision, light sensitivity, and the absence of color vision.
Alström syndrome is a very rare genetically inherited disease with sight loss due to RP.
Asymptomatic: An individual is a carrier for a disease, infection or condition but no symptoms are physically apparent.
Autosomal recessive means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
Best disease: A hereditary form of progressive macular dystrophy also known as Best vitelliform macular dystrophy.
Cone dystrophy: An inherited ocular disorder that is characterised by the loss of cone cells, the photoreceptors responsible for both central and color vision.
Dystrophy: The degeneration of cells.
Emphysema: A form of long-term lung disease.
Gene therapy: The introduction of genes into the body to treat disease.
Genetic factors: The science of heredity which attempts to understand inheritance factors.
Genotype: The genetic coding an individual has for a particular trait.
Mutation: A change in the genetic coding sometimes causing a different physical trait. Photopsia: Is the presence of apparent flashes of light and is associated with an array of different eye disorders.
Sorsby fundus dystrophy: An inherited macular dystrophy.
Sticklers syndrome: A group of genetic disorders affecting different tissues across the body and resulting in a range of eye conditions.
Usher syndrome: A genetic disorder causing both visual loss (due to RP) and hearing loss.
X-linked RPGR: A gene which can cause X-linked RP if a mutation or error occurs.